postpartal care - Moodle at Southeastern
advertisement

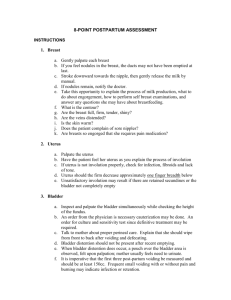
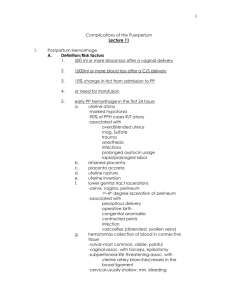
POSTPARTAL CARE LEARNING ACTIVITY MODULE SOUTHEASTERN LOUISIANA UNIVERSITY DEPARTMENT OF NURSING NURSING 403 1 POSTPARTAL CARE PURPOSE: To provide the student an opportunity to practice skills related to care of the client during the postpartal period. RATIONALE: The nurse is responsible for assessing and caring for the new mother during the fourth stage of labor to facilitate proper recovery and prevent complications. The nurse must be aware of signs indicative of normal/expected puerperal changes as well as warning signs of potential physiologic complications. OBJECTIVES: Identify the priorities of maternal care given during the fourth stage of labor including: 1. Identify the priorities of maternal care given during the fourth stage of labor. 2. Describe methods utilized for suppressing lactation. 3. Identify characteristics of uterine involution and lochia flow and the ways of measuring them 4. Perform selected perineal care techniques utilized with a new mother who has an episiotomy or laceration: a. Cleansing b. Ice Pack c. Dry Heat d. Topical medications e. Sitz bath 5. Demonstrate technique utilized for postpartal assessment. 6. Explain the procedure for Rhogam injection. REQUIRED RESOURCES: Medcom Trainex DVD (On library Reserve): Caring for the Postpartum Patient REQUIRED READINGS: Lowdermilk, D., & Perry, S. (2012). Maternity & women’s health care (10th ed.). St. Louis, MO: Mosby Elsevier. Ch 21 Nursing Care of the Family During the Postpartum Period 2 MATERIALS: Perineal Irrigation Bottle Tucks Anesthetic Spray (Dermaplast) RhoGam sample (if available) Disposable Gloves Sitz bath kit Disposable Pad Sanitary Napkin Bed Pan STUDENT LEARNING ACTIVITIES: 1. 2. 3. View the DVD. Wash hands. Go to designated station and begin. POSTPARTAL ASSESSMENT (BUBBLE HE) 1. BREASTS For breastfeeding mothers: 1. Feel the breasts for firmness or softness and note any lesions or redness. 2. Check the nipples for drying, cracking, or bleeding that may be due to poor latch during feedings. 3. Note if nipples are inverted-may necessitate additional measures to successfully breastfeed. 4. Assess for presence of colostrum (usually thick, yellow milk). For bottle feeding mothers: 1. Feel the breasts for firmness or softness and note any lesions or redness. Firm, hard breasts may indicate engorgement. In order to help suppress lactation, the following measures can be implemented: a. avoid nipple stimulation b. place back to shower so not to cause milk letdown c. ice packs d. anti-inflammatory medications e. tight bra In extreme cases, ace bandages are used to bind breasts during the fourth stage of labor to suppress lactation. Using the 6” ace bandage, wrap snugly around client’s torso beginning at the top of the breasts. The ace bandage should be applied over the client’s bra. If client has very large breasts, two ace bandages may be needed for sufficient support. Breast binders should be maintained for 48-72 hours. *** Ace bandage should be applied snugly, but not so tight to restrict breathing. 3 Remember to check doctor’s orders or standing protocol in clinical agencies prior to applying ace bandage. BREASTFEEDING MOTHERS SHOULD NOT HAVE BREASTS BOUND SINCE THIS WILL DECREASE LACTATION. 2. UTERUS The uterus involutes rapidly after childbirth, returning to the true pelvis within one week. Changes in lochia and fundal height are important indicators of the progress of normal involution, as well as indications of potential problems. Procedure: Fundal palpation 1. Put on clean examination gloves. 2. Position woman with knees flexed and head flat. 3. Just below the umbilicus, cup hand and press firmly into abdomen. At the same time, stabilize the uterus at the symphysis with the opposite hand. 4. If fundus is firm (and bladder is empty), with uterus in mid-line, measure its position relative to woman’s umbilicus. Lay fingers flat on abdomen under umbilicus; measure how many fingerbreadths (fb) or centimeters there are between the umbilicus and top of fundus. If the fundus is above the umbilicus, this is recorded as plus fb or cm; if below, as minus fb or cm. 5. If the fundus is not firm, massage it gently to help it contract and expel any clots before measuring the distance from the umbilicus. 6. Place hands appropriately; massage gently only until firm. 7. Fundus should be checked frequently to avoid complications. 8. Expel clots while keeping hands placed as shown in figure 20-3. With upper hand, apply firm pressure downward toward vagina; observe perineum for amount and size of expelled clots. NOTE: DAY 1 -- uterus located at umbilicus or just below; firm DAY 2 -- uterus 1 cm or more below umbilicus; firm Signs of Potential Complication – uterus deviated from the midline, boggy consistency, remains above the umbilicus after 24 hours. 3. BLADDER Assess bladder for fullness by palpation. A full bladder often displaces the uterus to the RUQ of the abdomen. A full bladder can interfere with contraction of the uterus and must be emptied (catheter or void). It is also necessary to assess bladder function following birth to identify possible infection or injury. The first 3 voids should be at least 200ml and no longer than 6 hours apart. 4. BOWEL Assess the return of bowel functioning. Bowel sounds should be active and C-section patients should be passing gas. Encourage ambulation and hydration to assist in the return of bowel regularity. 4 5. LOCHIA Position woman with knees flexed. Observe lochia on perineal pads, perineum, and on linen under the mother’s buttocks. Determine amount and color; note size and number of clots and odor. Observe perineum for source of bleeding (for example, episiotomy, and lacerations). NOTE: DAY 1 -- rubra; moderate; few clots, if any; fleshy odor of normal menstrual flow. DAY 2 -- rubra to serosa; moderate to scant; odor continues to be fleshy or absent NOTE: Differentiation between lochial and non-lochial bleeding. Lochia Non-lochial Bleeding Lochia usually trickles from The vaginal opening. The Steady flow is greater as the Uterus contracts. If the bloody discharge spurts from the vagina, there may be cervical or vaginal tears in addition to the normal lochia. A gush of lochia may result as the uterus is massaged. If it is dark, it has been pooled In the relaxed vagina; the amount soon lessens to a trickle of bright red lochia (in the early puperium). If the amount of bleeding continues to be excessive and bright red, a cervical or vaginal tear may be the source. NOTE: Findings provide a data base to differentiate between lochia of normal involution and discharge signaling complications such as infection or hemorrhage. ****SIGNS OF POTENTIAL COMPLICATIONS:**** Heavy, Foul odor, Red bleeding that is not lochia 5 6. EPISIOTOMY Care of an episiotomy or laceration 1. Turn model on her side and flex upper leg on hip. 2. Lift upper buttock. 3. Inspect perineum in good lighting. 4. Assess episiotomy site or laceration repair for intactness, edema, bruising, and redness. NOTE: DAY 1 – Edematous, clean, healing, intact; episiotomy or laceration repair edges approximated. DAY 2 – Edema lessening; clean, healing Cleaning: 1. 2. 3. 4. 5. Wash perineum with mild soap and water or plain warm water every 8 hours and after each urination. Fill squeeze bottle with tap water warmed to approximately 100oF (comfortably warm on the wrist). An antiseptic solution may be used, depending on the preference of the primary health care provider or agency. Position model on bedpan or commode. Position squeeze bottle between model’s legs and squirt solution over perineum from front to back. The entire bottle should be applied to perineum. Blot area dry with tissue or washcloth. Avoid contamination from anal area. Apply new clean sanitary pad. NOTE: SIGNS OF POTENTIAL COMPLICATIONS Pronounced edema, Edges not intact, Signs of infection, Marked discomfort Sitz bath 1. 2. 3. 4. 5. 6. Prepare for sitz bath by filling one-third to one-half full with water at correct temperature: 100.40 to 1050 (380 to 40.60). Clamp tubing and fill bag with warm water. Raise toilet seat, place sitz bath bowl with overflow opening toward back of toilet. Place container above toilet bowl. Attach tube into groove at front of bath. Loosen tube clamp to regulate rate of flow; fill bath to about one-half full. (Sitz bath should be done for approximately 20 minutes bid.) Topical Applications Apply anesthetic cream or spray, if prescribed; use sparingly three to four times per day or with sanitary napkin changes. Offer witch hazel pads (Tucks) for woman to use after voiding or defecating; woman should first pat perineum dry from front to back; then apply witch hazel pads. 6 7. HOMAN’S SIGN A positive Homan’s sign is classic indication of thrombophlebitis. Individuals who are confined to bed longer than 8 hours are at increased risk for development of thrombophlebitis. 1. 2. 3. Place client in supine position with legs extended and slightly flexed at knees. Ask patient to dorsiflex foot. Pain and tenderness in the calf of the foot of the affected extremity is a positive Homan’s sign. Repeat procedure on other lower extremity. Other signs of thrombophlebitis are edema, redness, and warm to touch. A positive Homan’s sign should be reported to the physician immediately and the client should be placed on bedrest with the affected extremity elevated on pillows. 8. EMOTIONAL STATUS Assess the mother’s coping skills and caretaking of herself and newborn. Note behaviors and moods, crying or outbursts. Watch for signs of depression. Take into account risk factors such as financial resources, family support, psych disorders, etc. Refer to social services as needed. RHOGAM Rh0(D) immune globulin (Rhogam) is a solution of gamma globulin that contains Rh antibodies. If administered within 72 hours of childbirth, it will prevent sensitization in the Rh-negative woman who has had a fetomaternal transfusion of Rh-positive fetal red blood cells. The usual dose is 300 mcg. It is administered after the birth to any woman who meets the following 3 criteria: 1) Mother must show Rh0 (D) negativity with no Rh antibodies. 2) The infant must show Rh0 (D) or D11 positivity. 3) Results of direct Coombs’ test on the cord blood must be negative and indirect Coombs’ test on mother must be negative. There must be some disagreement about whether Rh0 (D) immune globulin should be considered a blood product. Keep this in mind when discussing Rh0 (D) administration with women whose religious beliefs conflict with receiving blood products. In most institutions, precautions similar to those used for the transfusion of blood or blood products are taken when Rh0 (D) immune globulin is administered. 1. 2. 3. 4. 5. 6. 7. 8. Check physician orders for specific order. Assess the woman’s understanding of the purpose of administration of Rh0 (D) immune globulin. Ascertain the woman’s consent to administration. Check to be sure that the identification number on the woman’s hospital wristband corresponds to the identification number on the laboratory slip. Make sure that the lot number on the laboratory slip corresponds to the lot number on the vial of Rh0 (D) immune globulin. Check the expiration date on the vial to be sure the product is usable. Verify the above information with another nurse. Inject Rh0 (D) immune globulin intramuscularly. 7