Hospital * Physician Affiliations
advertisement

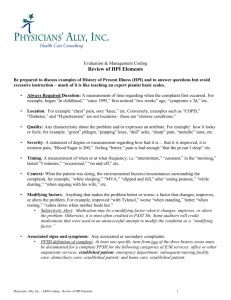
Physician Documentation & Billing IMPACT ON HOSPITAL REVENUE Trends in Healthcare • H O S P I TA L S H AV E B E E N A C Q U I R I N G P H Y S I C I A N PRACTICES. • H O S P I TA L S H AV E B E E N E S TA B L I S H I N G J O I N T VENTURES WITH PHYSICIANS. • H O S P I TA L S H AV E B E E N F O R M I N G A F F I L I AT I O N S WITH PHYSICIANS Hospital – Physician Affiliations The Effect on the Hospital Revenue Cycle • P H Y S I C I A N B I L L I N G S F R O M A F F I L I AT E D P R A C T I C E S N O W I M PA C T H O S P I TA L R E V E N U E . • PHYSICIAN BILLING ERRORS CAN NOW C R E AT E C O M P L I A N C E I S S U E S F O R T H E PA R E N T H O S P I TA L . • RAC AUDITORS ARE NOW FOCUSING ON E/M BILLINGS WHY YOU SHOULD BE CONCERNED Reason #1 Medicare Carrier Finds 50-90% Error Rate for E/M Codes Written by Leigh Page | February 22, 2011 Tags: claims | error rates | Medicare | Part B A random survey of claims by the Medicare Part B carrier in five states has uncovered average error rates of 50-90 percent for E/M codes, according to a report by Part B News. TrailBlazer, the carrier in Colorado, New Mexico, Oklahoma, Texas and Virginia, said the most common cause was "documentation errors." TrailBlazer also cited some obvious errors, such as the reason for encounter was to receive lab results, which doesn't count as an E/M and also some not so obvious ones, such as that the frequency of E/Ms billed per beneficiary exceeded documented needs for management of stable, chronic conditions. "I could see maybe 20 percent (error rate) or a little higher. But 90 percent I just haven't seen before," said Seth Canterbury, an education specialist for the University of Florida Jacksonville Physicians. OUR EXPERIENCE IN AUDITING THE DOCUMENTATION AND BILLING RECORDS FOR OVER 200 PHYSICIANS WE HAVE SEEN AVERAGE ERROR RATES BETWEEN 35% AND 70% WITH SOME MUCH HIGHER. WE FOUND BOTH UNDER CHARGED AND OVER CHARGED ERRORS. MOST ERRORS WERE CAUSED BY POOR OR INADEQUATE DOCUMENTATION BY THE PHYSICIANS. DOCUMENTATION?? WHY YOU SHOULD BE CONCERNED Reason #2 RACs Expand into Physician Practices, Adding Pressure to Existing Audit Burden Written by Lori Brocato | Thursday, December 20, 2012 HDI and Connolly Make First Strides Two RACs recently mentioned upcoming reviews of physician practices and medical groups. One is taking a generic approach, while the other will hone in on specific issues sorted by provider type. Regardless of the methodology used, however, we predict that other RACs will follow suit. WHAT YOU CAN DO: 1. Install sophisticated electronic medical documentation and billing systems in all affiliated physicians’ offices. (Can be expensive and will be effective only if physicians properly use it) 2. Hire medical scribes to assist each affiliated physician. (Very expensive and depends on the training of the scribes) 3. Teach the physicians to properly document and correctly bill for services. (A reasonably priced alternative that will be effective with most physicians) TYPICAL DOCUMENTATION FROM ELECTRONIC MEDICAL RECORD SYSTEM E & M BILLING THE OVERWHELMING MAJORITY OF PHYSICIAN BILLING IS FOR EVALUATION AND MANAGEMENT (E & M) SERVICES. THERE ARE CLEARLY DEFINED PROTOCOLS FOR THE PROPER DOCUMENTATION AND CORRECT BILLING OF E & M SERVICES. THERE ARE PUBLISHED AUDIT GUIDELINES FOR ESTABLISHING THE ACCURACY OF E & M BILLING. YET MANY PHYSICIANS ARE UNAWARE OF THESE PROTOCOLS AND GUIDELINES. EVALUATION & MANAGEMENT PROCESS E&M Encounter Take Patient History Document History Perform Examination Document Exam Make Clinical Decision Document Decision Making Code & Bill E & M Documentation Clear and concise medical documentation is required to provide patients with quality care, and is critical to receive accurate and timely payment. It is also necessary to ensure that a service is consistent with the patient’s insurance coverage and to validate the following: The medical necessity and appropriateness of the diagnostic or therapeutic services provided The site of service That services furnished have been accurately reported E & M General Principles The documentation of each patient encounter should be legible and include: •Reason for the encounter and relevant history, physical examination findings, and prior diagnostic test results •Assessment, clinical impression, or diagnosis •Medical plan of care •Date and legible identity of the observer Defining the levels of E & M services Key components: I. Patient History II. Examination III. Medical decision making Contributory components • Nature of presenting problem • Time • Counseling • Coordination of care PATIENT HISTORY History includes some or all of the following elements: Chief Complaint (CC) is required for any level of service and validates the medical necessity of the service. It should be a concise statement describing the symptoms, problem, condition, diagnosis, physician recommended return, or other factor that is the reason for the encounter. It is usually stated in the patient’s own words. History of present Illness (HPI) or Status of Chronic Conditions is required for any level of service and Must be documented by the MD. Review of Systems (ROS)* Past Family and/or Social History (PFSH)* *Must include Physician Notation, MD signature and date The extent of the history documented should depend on the nature of the problem HISTORY DOCUMENTATION SUMMARY Type of History History of Present Illness (HPI) Review of Systems (ROS) Past Family and/or Social History (PFSH) Problem Focused (PF) Brief 1 – 3 elements N/A N/A Expanded Problem Focused (EPF) Brief 1 – 3 elements Problem Pertinent 1 system N/A Detailed (D) Extended 4+ elements Extended 2 – 9 systems Pertinent 1 area Comprehensive (C) Extended 4+ elements Complete 9+ systems Complete 3 areas PHYSICAL EXAMINATION The extent of examinations performed and documented is dependent upon clinical judgment and the nature of the presenting problem. They range from limited examinations of single body areas to general multi-system or complete single-organ system examinations. PHYSICAL EXAMINATION DOCUMENTATION The body areas: • Head, including face • Back, including spine • Chest including breasts and axillae • Abdomen • Neck • Genitalia, groin, buttocks • Each extremity The organ systems: • Constitutional • Eyes • Ears, nose, mouth, throat • Cardiovascular • Respiratory • GI • GU • Musculoskeletal • Neurological • Skin • Psychiatric • Hem/lymph/imm 4 LEVELS OF EXAMINATION - CPT Problem Focused (PF): a limited examination of the affected body area or organ system. Expanded Problem Focused (EPF): a limited examination of the affected body area or organ system and other symptomatic or related organ systems. Detailed (D): an extended examination of the affected body area and other symptomatic or related organ systems. Comprehensive (C): a general multi-system examination or complete examination of a single organ system. MEDICAL DECISION MAKING Medical decision making refers to the complexity of establishing a diagnosis and/or selecting a management option, determined by considering the following factors: 1. Number of possible diagnoses and/or number of management options considered; 2. Amount and/or complexity of medical records, diagnostic tests, and/or other information that must be obtained, reviewed, and analyzed; 3. Risk of significant complications, morbidity and/or mortality as well as comorbidities associated with the patient’s presenting problems, diagnostic procedures, and/or possible management options. To qualify for a given type of medical decision making, two of the three above elements must be met or exceeded. MEDICAL DECISION MAKING SCORING FOR COMPLEXITY A Number of diagnoses and treatment options B Amount and Complexity of Data 1 Minimal/Low 2 Limited 3 Multiple 4 Extensive C Highest Risk Minimal Low Moderate High Type of Decision Making Straight forward Low Complexity Moderate Complexity High Complexity 1 Minimal 2 Limited 3 Moderate 4 Extensive If no column contains more than one entry, choose “Low Complexity” BILLING E&M SERVICES When billing for patient visits, select the codes that best represent the services furnished during the visit. It is the provider’s responsibility to ensure that the submitted claim accurately reflects the service provided. Do not use the volume of documentation to determine which specific level of service to bill. In order to receive payment from Medicare, the service must also be considered reasonable and necessary. New Patient Office Visit (All 3 key components met or exceeded) Level History Exam Medical Decision 99201 Problem Focused Chief Complaint Brief history of present illness (1 – 3 HPI elements) Exam of affected body area/organ system (1995 guidelines – At least 1 system with 1 element or 1 comment) Straight-forward 99202 Expanded Problem Focused Chief Complaint brief Hx of present illness (1 – 3 HPI) Problem pertinent system review (1 ROS) Exam of affected body area/organ system Exam of other symptomatic or related body area/organ system (At least 2 systems with at least 1 element or 1 comment) Straight-forward 99203 Detailed Chief complaint Extended HPI (4 or more elements) Extended system review (2 – 9 ROS) One pertinent PFSH 99204 Complete Chief complaint Extended HPI (4+ elem) Complete ROS (10+) Complete PFSH (all 3) Complete 99205 Complex or Severe Chief complaint Extended HPI (4+ elem) Complete ROS (10+) Complete PFSH (all 3) Extended exam of affected body area/organ system Extended exam of other symptomatic or related body area/organ system (At least 4 systems with at least 4 elements or 4 comments - 4 X 4 rule) Low single system specialty exam or Complete multi-system exam (1995 guidelines – at least 9 systems with 1 element or 1 comment) Moderate complexity Complete single system specialty exam or Complete multi-system exam (1995 guidelines – same as Level 4 above) High complexity Established Patient Office Visit (2 key components met or exceeded) Level 99211 Problem Focused History Exam Does not require presence of a physician Presenting problems are minimal 99212 Expanded Problem Focused Chief Complaint Brief history of present illness (1 – 3 elements) 99213 Detailed Chief complaint Brief history of present illness (1 3 elements) Problem pertinent system review (1 ROS) 99214 Complete Chief complaint Extended HPI (4+ elements) Extended ROS (2 – 9 ROS) Pertinent PFSH (1 PFSH) 99215 Complex or Severe Chief complaint Extended HPI (4+ elements) Complete ROS (10+ ROS) Complete PFSH (2 of 3 PFSH for complete) Medical Decision Exam of affected body area/organ system (1995 guidelines – At least 1 system with 1 element or 1 comment) Straight-forward Exam of affected body area/organ system Exam of other symptomatic or related body area/organ system (At least 2 systems with at least 1 element or 1 comment) Low Detailed exam (At least 4 systems with at least 4 elements or 4 comments – 4X4 rule) Moderate complexity Complete single system specialty exam or Complete multi-system exam (1995 guidelines – at least 8 systems with 1 element or 1 comment) High complexity Evaluating E & M Documentation How others will judge The quality of your Documentation 1. The patient history 2. The Exam 3. The complexity of your decision making Copy of the Marshfield Clinic Audit Worksheet commonly used To evaluate E & M documentation THE TRAINING APPROACH Electronic medical documentation and the use of scribes can be effective methods to reduce the problem of physician billing errors, but they are expensive to install and maintain. Physician documentation/billing training is a less-expensive alternative that can produce significant documentation improvements, increased revenue and reduced risk of compliance errors and RAC vulnerability. PHYSICIAN TRAINING I. Group training for Physicians and practice support staff. II. Sample audits of the billings and documentation for each Physician. III. One-on-one training with each physician. IV. Remedial follow-up audits and training at regular intervals. I. GROUP TRAINING All physicians, billers and support staff attend a 2 – 4 hour training session covering the following: A. A detailed explanation of how to correctly document an E & M encounter with relevant examples. B. Instruction on standard billing protocol and proper selection of the appropriate E & M code. C. Introduction to the standard audit worksheet used by outside auditors to evaluate the quality of the physician documentation and the accuracy of the billing. II. AUDIT OF SAMPLE BILLINGS A sample of 20 to 30 E & M bills are randomly selected for each physician. Each bill is carefully audited, using standard audit protocols, to confirm the accuracy of the bill and the completeness of the documentation Every error and inadequacy is clearly explained with indication of the correct or more appropriate choice. A report is prepared outlining the accuracy and completeness of the billings for each physician. III. ONE-ON-ONE PHYSICIAN TRAINING A qualified trainer meets with each physician for an individual one-hour post-audit training session. The audit report is presented and explained so the physician clearly understands every error or inadequacy and the correct way to document and bill. SAMPLE OF ACTUAL AUDIT RESULTS M. LECO & ASSOCIATES ABC MEDICAL PRACTICE PROVIDER E/M AUDIT RESULTS SUMMARY Provider DR. A DR. B DR. C DR. D DR. E DR. F DR. G DR. H DR. I DR. J DR. K DR. L DR. M DR. N DR. O DR. P DR. Q DR. R DR. S TOTALS Audit Date 10/3/2012 10/4/2012 10/31/2012 10/31/2012 10/23/2012 11/7/2012 10/22/2012 11/7/2012 11/7/2012 11/7/2012 10/31/2012 11/7/2012 12/18/2012 11/29/2012 12/19/2012 12/18/2012 12/19/2012 11/30/2012 12/4/2012 Post Audit Final Report Interview 10/8/2012 10/10/2012 10/18/2012 10/29/2012 11/15/2012 11/19/2012 11/15/2012 11/19/2012 11/15/2012 11/19/2012 12/13/2012 12/14/2012 12/13/2012 12/14/2012 12/13/2012 12/14/2012 12/19/2012 12/20/2012 12/19/2012 12/19/2012 12/19/2012 12/20/2012 12/21/2012 12/21/2012 1/5/2013 1/7/2013 1/8/2013 1/9/2013 1/8/2013 1/9/2013 1/9/2013 1/9/2013 1/10/2013 1/15/2013 1/11/2013 1/15/2013 1/17/2013 1/18/2013 Under Over Correct Total Coded Coded Audited 15 2 5 22 7 3 10 20 3 0 17 20 5 0 15 20 0 9 6 15 1 0 19 20 4 2 14 20 6 1 13 20 8 0 12 20 5 0 15 20 6 1 12 19 3 0 17 20 6 1 13 20 0 6 14 20 11 2 7 20 0 4 16 20 14 0 6 20 7 0 13 20 3 0 17 20 104 31 241 Typical report presented along with narrative to management staff 376 Error Rate 77.3% 50.0% 15.0% 25.0% 60.0% 5.0% 30.0% 35.0% 40.0% 25.0% 36.8% 15.0% 35.0% 30.0% 65.0% 20.0% 70.0% 35.0% 15.0% Revenue Impact $787.00 210.00 258.00 410.00 -505.00 20.00 50.00 140.00 220.00 145.00 10.00 90.00 200.00 -246.00 316.00 -160.00 420.00 370.00 120.00 35.9% 2,855.00 THE POTENTIAL BENEFITS Most physicians under code and under bill because of compliance concerns. Most physicians could code higher if they adequately documented. The average physician is under coding and under billing about $5 to $10 per patient encounter. Physicians can typically handle 20 – 40 encounters per day (approximately 500 per month or 6000 per year) That could mean $30,000 to $60,000 of under billing per year per physician. 100 physicians = $3 million to $6 million per year! RESULTS OF TRAINING Most physicians significantly improve the quality of their documentation and the accuracy of their billing. 2. Most physicians greatly reduce the risk of billing non-compliance because their improved documentation now supports their billing choice. 3. Many physicians increase their average amounts billed because the improved documentation adequately supports higher billing levels. 1. 2010 AVERAGE E/M CODE DISTRIBUTION FOR NEW PATIENT OFFICE VISITS 50 45 40 37 35 PERCENTAGE 35 30 25 20 13 15 13 10 5 2 0 99201 99202 99203 99204 E/M CODE Department of Health and Human Services Publication: "Coding Trends of Medicare Evaluation and Management Services"; May 2012 99205 ACCURATE E/M BILLING 2010 AVERAGE E/M CODE DISTRIBUTION FOR ESTABLISHED PATIENT OFFICE VISITS 50 46 45 40 36 PERCENTAGE 35 30 25 20 15 9 10 5 5 4 0 99211 99212 99213 99214 E/M CODE Department of Health and Human Services Publication: "Coding Trends of Medicare Evaluation and Management Services"; May 2012 99215