05. Deformations and defects of the upper and lower jaws
advertisement

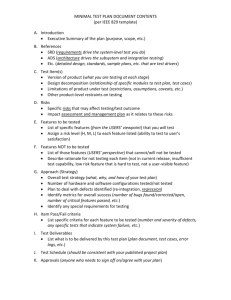
LECTURE 5 Deformation and defects of the upper and lower jaws: etiology, pathogenesis, classification, clinic, diagnostics. The essence of the methods of surgical treatment and indications for them. Distraction and compression therapies defects and deformities of the upper and lower jaw treatment. The two jaws are: upper jaw (maxilla) lower jaw (mandible) Macrogenia refers to a chin that grows beyond normal size, causing the nose and eyes to look disproportionately small. This may be corrected surgically by shortening or setting the chin back. Microgenia refers to a chin that hasn’t developed to normal/full size, causing the nose and eyes to look disproportionately large. This may be corrected surgically by adding more tissue. Macrognathia refers to an overgrown lower jaw that juts out beyond the upper jaw. This may be corrected by surgically reducing excess bone. Micrognathia refers to a lower jaw that hasn’t grown enough to be normally-sized. This may be treated with early orthodontics to align the teeth, followed by surgical chin advancement. Malocclusion refers to an excessively long upper jaw, resulting in a smile that shows most of the gums. This may be treated surgically by shortening and reshaping the jaw, followed by orthodontics to align the upper and lower jaws. Long Maxilla refers to a chin that grows beyond normal size, causing the nose and eyes to look disproportionately small. This may be corrected surgically by shortening or setting the chin back. Short Maxilla refers to an upper jaw that is proportionately too short for the face, which may hide the teeth and create an abnormal bite. Whether part of a birth anomaly or a result of an injury, it may be treated by surgically lengthening the jaw, followed by orthodontics to align the upper and lower jaws. Face Defects / Deformities What are Face Defects / Deformities? Face Defects / Deformities, also known as Facial Defects / Deformities are deformities in the growth of the skull and facial bones. These are congenital deformities (present at birth) and can be corrected by reconstructive surgery. Face Defects / Deformities can be Craniofacial Deformities (affecting the skull), Maxillofacial Deformities (affecting the upper jaw) and Dentofacial Deformities (affecting the bony structure and teeth). What are the different types of Face Defects / Deformities? •Cleft Lip - Cleft Lip or Hare Lip is a birth defect where the upper lip is split or separated either in the middle, on one side or on both the sides. •Cleft Palate - Cleft Palate is a condition when there is a cleft or a gap in the palate or the hard part of the roof of your mouth •Facial Cleft - This is a rare Face Defect / Deformity where a bone or skin in the middle of the face may be missing. •Craniosynostosis - This is a congenital Face Defect where the sutures (fibrous joints) of the skull bones fuse inappropriately and prematurely. Plagiocephaly - In this type of Face Defect / Deformity, the forehead and the brow stop growing. This Face Defect / Deformity produces a flattening of the forehead and the brow on the affected side while the forehead on the opposite side tends to be excessively prominent. Brachycephaly - This type of Craniofacial Deformity refers to a wide and high forehead region to be wide and high and the eyes may appear wide apart. Trigonocephaly - In this type of Face Defect / Deformity, the forehead looks pointed, like a triangle, with closely placed eyes. This Face Defect occurs due to closure of a suture that runs from the top of the head down the middle of the forehead, toward the nose. Scaphocephaly - This type of Face Defect / Deformity occurs when the suture that runs front to back, down the middle of the top of the head fuses prematurely. As a result, the shape of the skull becomes long and narrow. The skull is long from front to back and narrow from ear to ear. •Facial Palsy - This occurs due to paralysis of the facial nerve. In this kind of Face Defect, there is loss of control over facial expressions. •Chin Deformity - In this type of Face Defect / Deformity the chin is unusually small (mirognathia) or may be unusually large (macrognathia) •Upper Jaw (Maxillary) Deformity - One of the most common type of Upper Jaw (Maxillary) Deformity is called vertical maxillary excess. In this Facial Defect, there is excess bone of the upper jaw, the face appears long, the chin is recessed and the nose large in the profile view. •Lower Jaw (Mandibular) Deformity - There are two most common mandibular deformities; mandibular excess (protrusion) and mandibular deficiency (retrusion). •Deformational Plagiocephaly - This refers to asymmetrical shape of the head from repeated pressure to the same area of the head. This kind of Craniofacial Deformity usually results from keeping the infant's head in one position for long periods of time or it also be due to torticollis which is persistent tilt of the head to one side. •Vascular Malformations - Also known as lymphangioma, anteriovenous malformations or vascular gigantism. Vascular malformations are present at birth and increase in size as the child grows. •Hemangiomas - Also unknown as port wine stain, strawberry Hemangiomas and salmon patch. These are also called birth marks and mostly are present at birth (congenital). •Hemifacial Microsomia - In this Face Defect, the soft tissues and bones of the ear, mouth and jaw areas on one side of the face are under developed. •Microtia - In this Facial Deformity, the ear on one or both sides does not grow properly and may be accompanied by atresia of the ear canal. How are Face Defects / Deformities treated? The optimal time to seek surgical treatment for your child to repair Face Defects is before one year of age since the bones are still very soft and easy to work with. Surgical intervention may be necessary at a much earlier age depending upon the severity of Craniofacial Deformity. In some cases, surgery may have to be performed in stages to obtain optimum results. Your child's healthcare team will comprise of several health professionals (Craniofacial Team) with different expertise to assess and monitor your child's progress as he/she grows up. The Craniofacial Team will educate you and your family on how to best care for your child at home, and will also outline specific problems that require immediate medical attention. It is important to note that Craniofacial Deformities do not exist in isolation and may be accompanied by other congenital abnormalities. •Cleft Lip - The surgery for Cleft Lip is performed as a single procedure which also closes the nostril deformity. Bilateral Cleft Lip sometimes requires two surgeries. Depending on how extensive the birth defect is, surgery for Cleft Lip can take anywhere from 2 - 3 hours. •Cleft Palate - This attempt at restoration of normal anatomy of mouth would hopefully enable your child to eat and speak properly over time. The operation to repair Cleft Palate may take 2 - 3 hours and your child will be required to stay in the hospital for 3 - 4 days. •Craniosynostosis - The goal of surgical treatment to treat this Face Defect is to reduce the pressure in the head and correct the deformities of the face and skull bones. Following the operation to correct this Facial Deformity, it is common for the child to have a turban-like dressing around his / her head. The head may be reshaped by a non-surgical method i.e. a cranial molding helmet which allows growth in areas which appear flattened, and restricts growth in areas which appear prominent. •Hemengiomas - Hemangiomas can sometimes be quite disfiguring and may require treatment which may consist of steroid medications, embolization of blood vessels or removal by laser or surgical excision. Following surgical excision, your surgeon may perform Skin Grafting or use the technique of Skin Flap Grafting to reconstruct the damaged tissue. •Vascular Malformations - Facial Defects due to Vascular Malformations can be treated either by laser therapy (capillary malformations or port wine stains), embolization (arterial malformations) or by direct injection of a sclerosing, (clotting) medicine (venous malformations). •Deformational Plagiocephaly - This Craniofacial Deformity can be treated non-surgically. This can be done by alternating you child's sleep position (re-positioning) may resolve this problem. If the deformity is severe and cannot be resolved by re-positioning, then a remodeling band or helmet may be recommended. the helmet is made of a hard outer shell and soft inner lining and will help in correcting this deformity by applying mild pressures to inhibit growth in the prominent areas and allowing for growth in the flat regions. •Hemifacial Microsomia - For severely underdeveloped lower jaw, reconstruction using a bone graft taken from the ribs may be recommended. The external ear and the soft tissue of the cheeks would be reconstructed to attain facial symmetry. •Chin Deformity - This deformity can be treated by osseous genioplasty, or bony chin advancement, which is a simple procedure that moves a patient's own chin. Variety of facial implants can also be used to correct this Facial Deformity. Unusually large chins can be treated by bone reduction. What will my child's Craniofacial Team comprise of? Craniofacial team will comprise of pediatrician, pediatric plastic surgeon with expertise in Craniofacial Deformities, neurosurgeon, pediatric dentist, orthodontist, speech therapist, E.N.T. specialist, eye specialist, hearing specialist, psychiatrist, social worker and genetic counselor. Your child's craniofacial team will play a very important role in his care, education and rehabilitation that would be on-going depending on his or her needs. What is Distraction Osteogenesis procedure to treat Face Defects / Deformities? Distraction Osteogenesis (DO) - Also known as Bone Expansion. The method of Distraction Osteogenesis stimulates natural growth of new bone by stretching eventually leading to widening and lengthening of upper and lower jaw. Distraction Osteogenesis involves making small cuts in your jaw bone and applying forces by a distraction apparatus (DO device) which is attached to the teeth. The new bone will be formed (to fill the gaps in between the cuts) in response to the forces applied by this apparatus. The DO device is adjusted periodically until the desired lengthening and widening of the jaw bones is achieved. The device stays in place for about six to eight weeks to ensure that the gap is filled-in with stable new bone. It is removed in the operating room under sedation. New bone grows at the rate of one millimeter per day. Bone distraction requires two surgeries, one to implant the device and another to remove the device after the desired bone growth is achieved. It takes about six weeks for the new bone to heal and consolidate, and the device usually leaves only small scars. Distraction Osteogenesis is performed in 2 stages; first stage is implantation of the DO device and the second stage is removal of DO device. What is the outcome of procedure(s) to treat Face Defects / Deformities? The procedure(s) to treat Face Defects / Deformities have a good success rate provided they are diagnosed and treated in a timely fashion. A multidisciplinary approach to the treatment of Face Defects / Deformities has improved the management strategies and thus the outcomes. The multidisciplinary team provides care and support for the medical, physical, and psychosocial needs of the child and the family. B . R . A . N . D . of corrective treatments for Face Defects / Deformities Benefits of corrective treatments for Face Defects / Deformities •With the availability of state-of-art computer imaging system, you will have a better idea of the results that might be achieved by surgical intervention. A formal treatment plan will be put together utilizing the skills and expertise of craniofacial team. Corrective treatments for Face Defects / Deformities will most definitely improve the esthetics of your child's face, it will also improve breathing and feeding problems that are associated with Face Defects / Deformities. Risks of corrective treatments for Face Defects / Deformities Like all other Cosmetic & Plastic Surgery procedures, corrective treatments for Face Defects / Deformities involves the risk of complications including: •Asymmetry of your child's face - This a common problem when one side of your mouth and nose do not match the other side. In such a case, a revision surgery is performed to try and match both the sides of the face as closely as possible. •Incomplete repair of the Face Defects / Deformities - A second operation or revision surgery may be required for complete correction. •Infection of the incision site •Allergic reaction to anesthesia •Bleeding, swelling, bruising and delayed healing - It is normal to have some bruising and oozing of bloody discharge from the face areas which will soon subside. Alternatives to corrective treatments for Face Defects / Deformities •The treatment options discussed above are the best available for children born with Craniofacial Deformities. Now or Never Face Defects / Deformities can range from mild abnormalities of the teeth to extensive deformities involving the entire face and skull. Sophisticated reconstructive surgical techniques yield tremendously gratifying and outstanding aesthetic and functional results. Decision to have corrective treatments for Face Defects / Deformities •Each child's and family's needs are unique for corrective treatments for Face Defects / Deformities and the treatment plans are customized to meet all of a child's physical and emotional needs i.e. from special dietary or language requirements, to educational or emotional considerations. Craniometry and Functional Craniology Lecture outline 1. Introduction: definition, scope, and objectives 2. Kinematics and dynamics 3. Biomechanics: forces, deformation, stresses, strains 4. Form and Function 5. Bone remodeling and growth directions 6. Moss’ Hypothesis: Functional Matrix Hypothesis 7. Clinical applications Functional Craniology • Definition: The study of the craniofacial complex in relation to the fields of functional anatomy, comparative anatomy, embryology, and growth and development. • Scope: anatomy, embryology, histology, physiology, growth and development of the head and neck regions; theories of craniofacial growth; craniometry and cephalometry; and others • Objectives: 1) to relate the function to the morphology of the craniofacial complex. 2) to apply the theories of craniofacial growth and biomechanics to better understand the morphology, ontogeny and phylogeny of the craniofacial complex 3) to provide the scientific basis for the clinical applications in the treatment of craniofacial anomalies. Kinematics The measurement and description of the changes in size, shape, and location of the craniofacial complex. Dynamics The interpretation and description of the biological processes of the changes in size, shape, and location of the craniofacial complex. Kinematics The description of measurement. The description of the changes in size, shape, and location based on observations and measurements. The why, who, how, which and where, and what in measurement. 1) The history, scope, definition, and objectives of anthropometry 2) Introduction to craniometry and cephalometry 3) Define anatomical landmarks 4) Define anthropometric, craniometric, cephalometric measurements 5) Measuring devices and technical assessments 6) Data analysis, result descriptions a) qualitative vs quantitative b) absolute vs relative c) statistical analysis Dynamics What is the true meaning of a measurement? How to see beyond the numbers? And what are we looking for? What makes the changes in size, shape, and location of an organism or a structure (the transformation)? What are the modern hypotheses, paradigms, and syntheses in understanding these kinematic changes? 1) Introduction to functional craniometry 2) Basic principles in growth and development, especially in osteology and biomechanics. 3) The functional, biological, and mechanical interpretations of the transformation of an organism or a structure. 4) The evolutionary significance: the adaptation and the selection 5) Clinical applications Terminology used in Biomechanics Force: compression, tension, bending, shear, and torsion Deformation: Change of form due to the loading of forces Stress: the force per unit area Strain: the dimensional change expressed as a fraction (ratio) of the subject’s original size Force Compression, Tension, Shear, Bending, Torsion 1) Two basic forces: Compression & Tension 2) A combination of compression and tension: Shear & Bending 3) A combination of the above four forces: Torsion Compression: compression is the direct expression of the force, which pushes everything towards the center of an object. Tension: the opposite of compression; the force which pulls everything away from the center; where there is a compressive force, there must be a tensile force. Shear: shear is present, when two forces are thrusting in opposite directions but offset and slide past each other. Bending: is found between the pulling of tension and the pushing of compression. Torsion: a result of all the other four forces. Torsion is twist. Torsion is actually a specialized bending, a circular bending. Tension Original status Compression Shear Original status Bending Original status Torsion Facial Deformation Facial Deformation Skeletal Class III, concave profile Skeletal Class II, convex profile Source: Dr. Wisanu Charoenkul Source: Dr. Sonia Abraham Cephalic Form, Facial Form, and Arch Form Dolichocephalic (long and narrow head) Leptoprosopic (long and narrow face) Dolichuranic (V shape, narrow maxillary arch) Source: Dr. Christel Hummert FM, female,13y 6m * FM Female 13y 6m Source: Dr. Christel Hummert Mouth breather; Enlarged pharyngeal tonsil (adenoid) Form (Structure) and Function Form (structure) follows Function. Function determines form (structure). Function controls form (structure). Function regulates form (structure). Form (structure) is the realization of information and the product of the functional attributes. Cranial Sutures 1. Edge-to-edge suture No force loading 2. Beveled suture Shear force [Squamosal suture] 3. Serrated suture Intermittent tension force [Sagittal suture] 4. Beveled and serrated suture Intermittent tension and shear force 5. Butt-ended sutures Intermittent compressive force “Form Follows Function” Synovial Joints (I) 1. Plane (gliding) joint Sliding motion of all directions [ Intermetatarsal joint] 2. Hinge joint Flexion/extension [ Humeroulnar joint] “Form Follows Function” Illustrations: http://www.science.ubc.ca/~biomania/tutorial/bonejt/intro.htm Synovial Joints (II) 4. Ellipsoidal (condyloid) joint flexion/extension, adduction/abduction, circumduction, but no rotation 3. Pivot joint Rotation [Radioulnar joint] [Temporomandibular joint] “Form Follows Function” Illustrations: http://www.science.ubc.ca/~biomania/tutorial/bonejt/intro.htm Synovial Joints (III) 5. Saddle joint Similar to ellipsoidal joint, but freer 6. Ball and socket joint flexion/extension, adduction/abduction, circumduction, and rotation [First carpometacarpal carpometacarpaljoint] joint] [Glenohumeral joint] “Form Follows Function” Illustrations: http://www.science.ubc.ca/~biomania/tutorial/bonejt/intro.htm Functional Structure of Skull (From a mechanical point of view) In the force loading areas, pillarlike struts serve as mechanically efficient reinforcements to resist and dissipate pressure and traction, especially to the masticatory force. 6 2, 3 1) Fronto-nasal pillar 2) Zygomatic arch pillar with vertical branch 3) Zygomatic arch pillar with horizontal branch 4) Basal arch in upper jaw 5) Basal arch in lower jaw 6) Occipital pillar 7) Pterygoid-palate pillars 1 4 5 Functional Structure of Skull (From a mechanical point of view) • In the non- or less force loading areas, adipose tissue and pneumatic cavities fill those mechanically neutral areas. a b c e d 1) Paranasal sinuses a) Frontal sinus b) Ethmoid sinus c) Sphenoid sinus d) Maxillary sinus 2) Accessory tympanic spaces e) Mastoid air cells Sagittal crests and temporal muscle orientations Hominids compared to pongids Hominid: Australopithecine Temporal muscle fibers oriented towards the posterior teeth; emphasis on the posterior teeth in mastication and dietary adaptation Pongid: male gorilla Temporal muscle fibers oriented towards the anterior teeth; emphasis on the anterior teeth in mastication and dietary adaptation Bone remodeling Deposition: the biological process of laying down the bone Resorption: the biological process of removing the bone Remodeling: A basic part of bone growth involves simultaneous deposition and resorption on all inner and outer surfaces of the entire bone. It provides regional changes in shape, dimensions, and proportions. Drift: Growth movement of an enlarging portion of a bone by the remodeling. The combinations of deposition and resorption result in growth movement toward the depository surface. Displacement: The growth movement of a whole bone as a unit. The bone is carried away from its articulation in relation to other bones. Direction of growth: 1) the direction of drift 2) the direction of displacement 3) the net direction of drift and displacement. The Growth of the Coronoid Process Deposition (+); Resorption (-); Direction of growth (arrow) The Growth of Mandible Deposition (blue arrow); resorption (white arrow) The Remodeling (Growth) Direction: The “V” Principle Drift vs Displacement Drift: the growth movement of an enlarging portion of a bone by the remodeling. Displacement: The growth movement of a whole bone as a unit. Direction of growth: the net growth direction of drift plus displacement. Head (craniofacial complex) is a region, where a series of functions are carried out. These functions include vision, hearing, speech, mastication, swallowing & digestion, respiration, neural integration, and others. The successful execution of a function requires biomechanical protection and support. Moss’ craniofacial growth theory: Function of the craniofacial complex region is performed by the Functional Cranial Components (F.C.C). Functional Matrix Hypothesis (Moss’ Hypothesis) “The functional matrix is primary and the presence, size, shape, spatial position, and growth of any skeletal unit is secondary, compensatory, and mechanically obligated to changes in the size, shape, spatial position of its related functional matrix” (Moss, 1968) Functional Matrix Hypothesis (Moss’ Hypothesis) “The origin, development and maintenance of all skeletal units are secondary, compensatory and mechanically obligatory responses to temporally and operationally prior demands of related functional matrices.” THE FUNCTIONAL MATRIX HYPOTHESIS One Function Functional Cranial Component Functional Matrix Skeletal Unit 1. Periosteal Matrix -------------------------------> 1. Microskeletal 2. Capsular Matrix --------------------------------> 2. Macroskeletal a. Masses b. Functioning spaces Types of Functional Matrix 1. Periosteal matrix (e.g., muscles) Active growth Deposition and resorption Affect size and/or shape 2. Capsular matrix (e.g., brain, oral cavity) Passive growth No deposition No resorption Affect location Growth Craniofacial Growth Active growth process Active growth (Periosteal) + Passive growth (Capsular) = Total growth 1) Sutural growth 2) Bone remodeling 3) Cephalic cartilage growth Passive growth process 1) The growth of neural, orbital, CSF, and other masses and real substances 2) The expansion of oro-nasopharygeal and other functioning spaces Use of the “Functional Matrix” in the therapy of orthodontics, dentofacial orthopedics, and orthognathic and craniofacial surgery 1. Orthodontics Periosteal Matrix [Teeth] ------------> Skeletal Unit [Alveolar Bone] 2. Dentofacial Orthopedics and Orthognathic Surgery Capsular Matrix -------------> Multiple Skeletal Units [Functional Appliances] [Jaw Bones] Capsular Matrix -------------> Multiple Skeletal Units [Distraction osteogensis: e.g., hemifacial microsomia] [Jaw Bones] 3. Craniofacial surgery Capsular Matrix -------------> Multiple Skeletal Units [Craniotomy: e.g. Crouzon Syndrome] [cranial bones] [Distraction osteogensis: e.g., Treacher Collin Syndrome] [facial and jaw bones] Introduction: definition, scope, and objectives Kinematics and dynamics Biomechanics: forces, deformation, stresses, strains Form and Function Bone remodeling and growth directions Moss’ Hypothesis: Functional Matrix Hypothesis Clinical applications References Enlow, D.H. (1990). Handbook of Facial Growth (3rd edition). Philadelphia, Pennsylvania: W.B. Saunders Company. Moyers, R.E. (1988). Handbook of Orthodontics (4th edition). Chicago, Illinois: Year Book Medical Publishers, Inc. Proffit, W.R. (2000). Contemporary Orthodontics (3rd edition). St. Louis, Missouri: Mosby, Inc. Ranly, DM (1980). A Synopsis of Craniofacial Growth. Norwalk, CT: AppletonCentury-Croft. THANK YOU FOR ATTENTION