Climate change and infectious diseases
advertisement

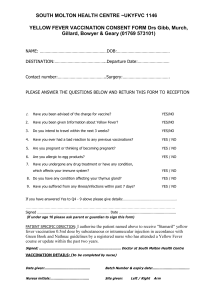
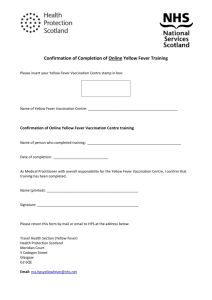
The Possible Effect of Climate Change on Selected Infectious Diseases in South Florida Office of Epidemiology and Disease Control Miami-Dade County Health Department Juan A. Suarez Regional Environmental Epidemiologist Presentation at the Medical Campus of Miami Dade College January 28, 2008 Contributors This presentation was adapted from a November 2007 version prepared by: Fermin Leguen, MD, MPH, Director Office of Epidemiology and Disease Control Juan A. Suarez Regional Environmental Epidemiologist Menhel Kinno, MPH candidate, Intern OEDC Some additional data slides from the Bureau of Community Environmental Health-FDOH Introduction Climate change in the form of global warming and extreme weather are increasingly mentioned in the media and journal articles as issues to be dealt with in the next decades. Human health will be affected by changes in the environment of insects and microorganisms that in turn are vectors or agents for disease in man. Assumptions The following discussion assumes rise in sea levels, global increase in temperature, and intrusion of the ocean water on fresh bodies of water and drinking water wells. The science behind these assumptions is based on observations but also on predictions. Causes of these effects remain controversial. Anthropogenic vs. natural variations. The physical results are based on the Intergovernmental Panel on Climate Change’s report. Selected Infectious Diseases Vector borne diseases Water borne diseases Rodent borne diseases Rabies Vector-borne diseases: Mosquito transmitted diseases: Dengue & Dengue Hemorrhagic Fever Yellow Fever West Nile Fever Malaria Other insects transmitted diseases: Lyme disease Tularemia Chagas disease Dengue Fever & Dengue Hemorrhagic Fever genus Flavivirus There are four serotypes of the virus that cause the disease. Transmitted by Aedes aegypti (a domestic, daybiting mosquito, has a world wide distribution in tropical area) Clinical features: High Fever, headache, Backache, joint pain, eye pain, Rash Nausea and vomiting Hemorrhagic manifestation (DHF) which is potentially lethal. No specific treatment is available. No vaccination is available. Mosquito control. Source: CDC, 2007 Dengue Fever & Dengue Hemorrhagic Fever In 2005, 2.5 billion people at risk of Degue fever. The Aedes mosquito has a worldwide distribution in the tropical and sub-tropical areas. Source: CDC, 2005 Yellow Fever Genus Flavivirus It is also transmitted by Aedes mosquito. This virus is restricted to only 2 regions: Africa and South America. Clinical Features (incubation period of 3-6 days): Asymptomatic. Acute phase: Fever (sometimes Paradoxical fever with low pulse rate), aches, Nausea and vomiting, 15% Toxic phase: jaundice, abdominal pain with vomiting. Bleeding can occur from the mouth, nose, eyes and/or stomach. ½ die within 10-14 days. Three types of transmission cycle: Sylvatic (jungle): sporadic cases in forest. Intermediate yellow fever: in Africa only. Urban yellow fever: epidemics. No specific treatment is available. Prevention: Vaccination and mosquito control WHO, Fact Sheet, 2001 West Nile Fever: Genus Flavivirus Transmitted by female Culex pipiens mosquitoes Clinical Features: Incubation period: 2-15 days fever, headache, tiredness, and body aches, occasionally with a skin rash and swollen lymph glands 1 in 150 ( Neuro-invasive disease, West Nile encephalitis or meningitis or West Nile poliomyelitis) Treatment: no specific treatment (antiviral “Ribravirin”) Prevention: mosquito control, vaccination only available for horses. CDC, 2007 2007 West Nile Virus Activity in the United States (Reported to CDC as of November 6, 2007) Source: CDC, 2007 Malaria Parasitic infection by Plasmodium Human malaria is caused by four species: Plasmodium vivax & ovale P. malariae P. falciparum 41% of the global population lives in area at risk of malaria. Malaria is transmitted by female anopheles mosquito. Clinical Feature (incubation period of 10-14 days): Fever Rigor Sweating Treatment: anti-malarial medication and supportive therapy Prevention: prophylactic treatment and mosquito WHO, 2007; CDC, 2007 control. Lyme disease Bacterial infection by Borrelia burgdorferi. It usually lives in small animals (mice, squirrels, Transmitted by: Ixodes scapularis, Ixodes pacificus (blacklegged ticks) Clinical Feature (incubation period 3-30 days): fever, headache, fatigue Erythema migrans (characteristic rash in 70-80%). In untreated patient it can cause a wide ray of symptoms (Nervous system, heart, and joint). Treatment: oral antibiotics, intravenous AB in severe cases Prevention: vaccine is no longer available, tick control This disease may be more of an issue in the Northeast/Central states, unclear if South Florida would be affected. Reported Cases of Lyme Disease by Year, United States, 1991-2005 Source: CDC, 2005 Chagas disease It is a parasitic infection by Trypanosoma cruzi Transmitted by kissing bud (triatomine vector). Clinical Feature: Acute: occurs after infection and it is characterized by fever or swelling around the site of inoculation Chronic Intermediate: asymptomatic stage. Chronic (30%): life-threatening chronic complications (dilated cardiomyopathy, dilated esophagus, toxic megacolon) Treatment: Prevention: insect control. CDC, 2007 Why there will be an increase in Vector Transmitted disease? Warm temperature and surface water are essential for insect breeding (especially mosquito) Stagnant water with humid condition are both necessary for breeding. Warmer temperature leads to: Enhance vector breeding, Increase vector survival, Increase vector biting rate, Reaching higher altitude, and reduce the pathogen’s maturation period with the vector. Very hot temperature with dry condition can reduce the survival of insects. WHO, 2007 Water & Food borne diseases: Giardiasis Cholera and other Vibrios Salmonella Giardiasis Parasitic infection by Giardia lamblia Transmitted mainly through contaminated water. Clinical Feature (incubation period 1-2 weeks): Asymptomatic. Diarrhea, Nausea and Vomiting, gas and flatulence, abdominal cramps Chronic diarrhea and malabsorption and weight loss. Treatment: oral antibiotics Prevention: good hygiene, avoidance of contaminated water and food. CDC, 2007 Cholera Causative agent: Vibrio cholera It is mainly a water-borne disease Clinical symptoms: Acute, watery (rice water like) diarrhea. Vomiting Leg cramps Rapid loss of body fluids and dehydration that might lead to death within hours without treatment. Treatment: antibiotics and IV fluids Prevention: oral vaccine, avoid contaminated water and food. WHO, 2007 Salmonella Bacterial infection by Salmonella Water & food borne disease Clinical features: Fever Diarrhea, and abdominal cramps Reiter's syndrome Chronic carriers Treatment: oral antibiotics Prevention: avoidance of raw or undercooked eggs, poultry, or meat. WHO, 2007 Vibrio vulnificus Causative agent: marine bacterium Vibrio vulnificus Water-borne (wounds) and consumption of raw oysters and shellfish Incubation: 12-72 hours Clinical picture: Septicemia in immunosuppressed, or chronic liver disease, or hemochromatosis, or cirrhosis Case fatality from 50-90% Cellulitis, myositis, shock, hypotension, bullous skin lesions, intravascular coagulation, thrombocytopenia Treatment: antibiotics Prevention: avoid contact of wounds with seawater and avoid eating raw or undercooked oysters and shellfish Vibrio vulnificus in Florida, 1990-2006 Exposure Wound Oysters Unknown Crab Clams Shrimp Total # Cases 211 156 55 7 3 1 433 Deaths from Vibrio vulnificus in Florida, 1990-2006 Exposure Oysters Wound Unknown Crab Shrimp Clams Total # Deaths 66 24 20 2 1 1 114 % Total Cases 15.2 5.5 5.2 0.5 0.3 0.3 26.4 Vibrio vulnificus Cases and Deaths from Various Exposures, Florida 1990-2006 Exposure # Cases # Deaths Deaths % Total Cases Wound 211 24 5.5% Oysters 156 66 15.3% 55 20 4.6% Crab 7 2 0.5% Clams 3 1 0.2% Shrimp 1 1 0.2% 433 114 26.4% Unknown Total Rodent-Borne Disease: Plague Plague Bacterial infection Yersinia pestis Transmitted by: Flea bite Contact with infected rodent Inhalation or ingestion of infected material. It is still widely distributed in the tropics and subtropics and in warmer areas of temperate countries. Clinical Feature: Bubonic form (most common type in which the disease is transmitted by flea and it mainly affects the lymph nodes (bubo) which became painful and may suppurate) Septicaemic form Pneumonic form (least common but most virulent) Treatment: antibiotics and supportive therapy Prevention: rodent control, flea control, vaccination only for high risk group. WHO, Fact Sheet, 2005 Rabies Viral infection by Animal bite (domestic and wild animals). Clinical Feature: Initially, non-specific symptoms Acute stage, signs of hyperactivity (furious rabies) or paralysis (dumb rabies) predominate. paralysis eventually progresses to complete paralysis followed by coma and death in all cases, usually due to respiratory failure. Without intensive care, death occurs during the first seven days of illness. Treatment: immediate cleaning of the wound, and post-exposure vaccination Prevention: vaccination of domestic animals, vaccination of individuals at high risk, avoidance and control of wild animals. WHO, Fact Sheet, 2006 Control Measures Control measures for these diseases and their vectors are well known and established. However, new challenges will be encountered in the control of insects and microorganisms under the new environmental conditions and new methods must be researched and implemented. Summary The true effects that climate change will have on infectious diseases will be hard to predict but we can, with the present knowledge, estimate which of these will be more of a problem. We must also not forget that today’s challenges with other issues in infectious diseases, not related to climate change, may also continue. Examples include antibiotic resistance, limited resources, and new emerging pathogens. UN Millennium Development Goals Goal # 7 Ensure environmental sustainability: Integrate the principles of sustainable development into country policies and programmes; reverse loss of environmental resources Reduce by half the proportion of people without sustainable access to safe drinking water Achieve significant improvement in lives of at least 100 million slum dwellers, by 2020 Dr. Julie Gerberding, CDC Oct 2007 Many of the activities needed to protect Americans from the health effects of climate change are mutually beneficial for overall public health….it is also important that potential health effects of environmental solutions be fully considered. I am persuaded that global climate change is one of the most important issues that we will face this century. With almost 1,200 miles of coastline and the majority of our citizens living near that coastline, Florida is more vulnerable to rising ocean levels and violent weather patterns than any other state…Florida will provide not only the policy and technological advances, but the moral leadership, to allow us to overcome this monumental challenge." References IPCC, 2007: Summary for Policymakers. In: Climate Change 2007: The Physical Science Basis. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change [Solomon, S., D. Qin, M. Manning, Z. Chen, M. Marquis, K.B. Averyt, M.Tignor and H.L. Miller (eds.)]. Cambridge University Press, Cambridge, United Kingdom and New York, NY, USA. http://ipcc-wg1.ucar.edu/wg1/Report/AR4WG1_Print_SPM.pdf References Control of Communicable Diseases Manual, 18th Ed. David L. Heymann, MD, Editor, APHA, WHO. Centers for Disease Control and Prevention http://www.cdc.gov/ Environmental Protection Agency http://www.epa.gov/climatechange/effects/health.html World Health Organization http://www.who.int/en/ United Nations. UN Millennium Development Goals. http://www.un.org/millenniumgoals/