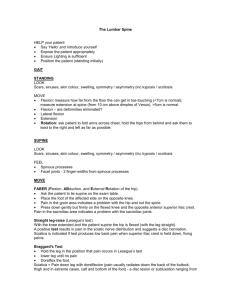
Hip Joint Orthopedic Tests
advertisement

Hip fractures occur most frequently in the elderly population. Most common types are intertrochanteric and intracapsular. Intertrochanteric and femoral head fractures typically do NOT disrupt the blood supply. Intracapsular fractures disrupt the blood supply to the femoral head and can lead to avascular necrosis. Clinical Signs and Symptoms Hip pain Shortened extremity Externally rotated extremity Referred pain to medial thigh Procedure: Patient supine. Tap the inferior calcaneous with your fist. Positive Test: Local pain in the hip joint may indicate a femoral head fracture or joint pathology. Pain in the thigh or leg secondary to trauma may indicate a femoral, tibial, or fibula fracture. Pain local to the calcaneous may indicate a calcaneal fracture. A hip joint contracture is a condition of soft tissue stiffness that restricts joint motion. This can be caused by immobility due to spasticity, paralysis, ossification, bone trauma, or joint trauma. A frequently moved joint is unlikely to develop a contracture deformity. The joint capsule, ligaments, or muscle tendon units can be involved. Clinical Signs and Symptoms Stiff hip joint Limited hip range of motion Inability to position joint in the neutral position Hip joint pain on range of motion Procedure: Supine patient. Approximate each knee to the chest one at a time. Palpate quadriceps on the unflexed leg. Positive Test: No tightness – suspect restriction at the hip joint structure or joint capsule. If tightness is palpated on the side of the involuntary flexed knee – hip flexure contraction is suspected. Common problems associated with the hip joint include the following: Osteoarthritis, sprains, fractures, dislocations, bursitis, tendinitis, synovitis, and avascular necrosis of the femoral head. The following tests determine whether a general lesion of the hip is present. Further diagnostic imaging can determine the exact pathology. Clinical Signs and Symptoms Hip pain Shortened extremity Externally rotated extremity Referred pain to medial thigh Procedure: Patient supine. Flex leg and place foot flat on table. Grasp femur and press it into the acetabular cavity. Cross leg to opposite knee. Stabilize ASIS opposite and press down on knee of side tested. Positive Test: Pain in the hip – inflammatory process in the hip joint Pain secondary to trauma – may indicate fracture Pain may indicate avascular necrosis of femoral head Faber – Flexion, abduction, & external rotation Procedure: Patient standing. Grasp waist. Thumbs on PSIS b/l. Instruct patient to flex one leg at a time. Positive Test: If the patient cannot stand on one leg because of pain If the opposite pelvis falls or fails to rise This tests the integrity of the hip joint opposite the side of hip flexion Procedure: Patient supine. Flex the hip and knee to 90degrees. Rotate the thigh outward and the knee medially. Press down on the knee with one hand and pull up on the ankle with the other. Positive Test: This test externally forces the head of the femur into the acetabular cavity. May indicate an inflammatory process in the joint such as osteoarthritis. Pain secondary to trauma – suspect fracture of the acetabular cavity or rim. The menisci are C-shaped discs of fibrocartilage that are interposed between the condyles of the femur and tibia. Primary function is load transmission or weight bearing. Secondary function is shock absorption during gait. Contribute to joint stability and lubrication. Nerve endings provide proprioceptive feedback for joint position. A tear or loss of the menisci, either partial or complete, hinders their ability to perform. A twisting injury to the knee with the foot in weight bearing can injure the menisci. The outer 20% is vascular – peripheral injuries may heal. Clinical Signs and Symptoms Local medial or lateral joint pain Limited knee range of motion Crepitus upon movement Joint effusion Knee buckling Pain on walking up and down stairs Pain on squatting Procedure: Patient prone. Flex leg to 90 degrees. Grasp the patient’s ankle and apply downward pressure while you internally and externally rotate the leg. Positive Test: Flexing the knee distorts the meniscus. Downward pressure further stresses the meniscus. Pain or crepitus on either side indicates a meniscus injury on that side. The major ligaments of the knee are the anterior and posterior cruciate and the medial and lateral collateral ligaments. Ligament injuries are among the most serious knee disorders. Usually due to traumatic stress to the knee while bearing weight. Valgus stress may sprain or tear the medial collateral ligament. Varus stress may sprain or tear the lateral collateral ligament. Both of these stresses with a rotational force may sprain or tear the anterior and/or posterior cruciate ligaments. Clinical Signs and Symptoms Knee pain Limited range of motion Difficulty in weight bearing Joint effusion Knee giving out; chronic unstable knee Procedure: Patient supine. Flex the leg and place the foot on the table. Grasp behind the knee and pull and push on the leg. Hamstring tendons must be relaxed. Positive Test: More than 5 mm of tibial movement on the femur when leg is pulled - injury or tear to one or more of the following structures is indicated: Anterior cruciate ligament Posterolateral capsule Posteromedial capsule Medial collateral ligament (more than 1cm movement) Iliotibial band Posterior oblique ligament Arcuate-popliteus complex If excessive movement occurs when the leg is pushed, an injury to one or more of the following structures in indicated: Posterior cruciate ligament Arcuate-popliteus complex Posterior oblique ligament Anterior cruciate ligament Procedure: Patient prone. Flex leg to 90°. Stabilize patient’s thigh with your knee. Pull on the ankle while internally and externally rotating the leg. Positive Test: Distraction of the knee takes pressure off the meniscus and puts strain on the medial and lateral collateral ligaments (non-specific). The patella protects the anterior aspect of the knee. It acts as a fulcrum that increases the mechanical advantage of the quadriceps. The patella lies in the trochlear groove. With normal flexion and extension it tracks smoothly in the groove. Many causes of anterior knee pain involve abnormal tracking of the patella or direct trauma to the patella. Patellofemoral injuries include fractures, dislocations, malalignment syndrome, chondromalacia patellae, and patellofemoral arthritis. Clinical Signs and Symptoms Anterior knee joint pain Knee joint effusion Popping sensation Joint crepitus Discomfort with stair climbing Knee buckling Procedure: Patient supine. Manually displace the patella laterally. Positive Test: A look of apprehension on the patient’s face and a contraction of the quadriceps muscle indicates a chronic tendency to lateral patella dislocation. Pain is also present with this test. Ligaments Anterior and posterior talofibular, anterior tibiofibular, and deltoid ligaments. If any of these ligaments are torn, the tibia can separate from the fibula and the talus may become unstable. Common mechanism of injury is a supination or inversion force. The foot turns under the ankle after walking or running on uneven surfaces or when landing on an inverted foot after a jump. The most common injured ligament is the anterior talofibular ligament. Ligament laxity can lead to chronic ankle sprains. Clinical Signs and Symptoms Ankle swelling Static ankle pain Pain on passive motion Tenderness over affected ligament Procedure: Patient supine. Stabilize ankle with one hand. Press posterior on tibia with the other hand. Next, grasp anterior aspect of the foot with one hand and the posterior aspect of the tibia with the other. Pull anterior. Rationale: Gapping with posterior push – tear anterior talofibular Gapping with anterior pull – tear posterior talofibular Achilles tendon rupture generally occurs in adults aged 30 to 50. It is usually spontaneous in athletes who account for most of these injuries. Decreased vascularity of the Achilles tendon as the patient ages may contribute. Mechanism of injury - forced dorsiflexion of the foot as the soleus and gastrocnemius contract. Rupture occurs 2 to 6 cm from the insertion of the Achilles tendon into the calcaneus. As the proximal aspect of the tendon retracts, there is usually a palpable defect of the tendon. Clinical Signs and Symptoms Severe posterior ankle pain Inability to stand on toes Posterior leg and heel swelling Posterior leg and heel ecchymosis Procedure: Patient prone. Flex knee. Squeeze the calf muscles against the tibia and fibula. Rationale: The the gastrocnemius and soleus are squeezed, they mechanically contract. They are attached to the Achilles tendon, which plantar-flexes the foot. If the tendon is ruptured, contraction of the gastrocnemius and soleus muscles will NOT plantarflex the foot.