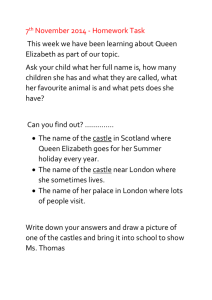
Dr. Pector's presentation from December 2007
advertisement

Stress and the Health Care Worker: Psychosocial Perspectives Elizabeth A. Pector, M.D. Naperville, Illinois synspectrum.com steps to master stress 1. Claim it: everyone has stress. 2. Name it: everyone’s stressors are different. (ABCs of needs,TWERPS) 3. Reframe it: Look at your stress & stressors in a different way. Hardiness, coping. 4. Tame it: prepare, self-care, share, dare, be aware December 2, 2007 ©Elizabeth A. Pector, M.D. 2 1. Claim it: Stress 101 “Stake your claim in the gold mine of stress” • • • • • • Stress: present in all organisms – Nonspecific response to any demand placed on the organism – Impulse pushes us out of balance or equilibrium Stressors: factors that provoke stress response Stress responses – Acute Fight-or-Flight Chronic stress. Healthy stress (Eustress)- adaptive – Motivates growth & learning. Unhealthy stress (Distress):- maladaptive – Can result from “impossible” demands. Biopsychosocial effects Job stress: – “Harmful … responses that occur when requirements of the job do not match the capabilities, resources or needs of the worker.’’ NIOSH – 10% of total occupational disease claims are due to stress. Marine et al 2007 December 2, 2007 ©Elizabeth A. Pector, M.D. 3 Mental Health • • • • • • 2. Name it: ABCs of basic human needs Accomplishment—reach worthwhile goals Belonging—relationships help define us Comfort—feeling secure Dependability—predictable aspects of life Esteem—feeling good about yourself Finances—enough funds for a fulfilling life – Maddi & Khoshaba, 2005. December 2, 2007 ©Elizabeth A. Pector, M.D. 4 Stressful Twerp • • • • • • 2. Name it: Your stressors: “TWERPS” Tasks, Time Worries Environment, Expectations, Events Roles, Responsibilities People (yourself, others, communication) Situations: all of the above put together – How much is in your control? – How much is from outside circumstances? December 2, 2007 ©Elizabeth A. Pector, M.D. 5 Stress occurs at interface between work & worker • • • • Work factors Personal (worker) factors Do they fit well together? If they don’t fit, can work or worker change to lower stress levels? – Limited evidence shows worker- and work-directed interventions lowers stress in health care workers. – Marine et al. 2007 December 2, 2007 ©Elizabeth A. Pector, M.D. 6 Job stress & health Job stressors Job Demands Workload Shift work Limited worker control Technology Client demographics (age, culture) Organizational Factors Role demands Management style Career security Interpersonal relations Change Physical Environment Space, noise, heat, cold, lighting, etc. December 2, 2007 Individual factors Acute stress Personality traits Motivation Talent Training Chronic stress Reactions: Physical Stressrelated Illness: Psychological Behavioral Finances Family Hx trauma Non-work stressors Social support Coping skills Hardiness Buffer factors ©Elizabeth A. Pector, M.D. Heart disease Depression Infections OR Healthy worker Adapted from NIOSH Publ. 87-111; 7 Vachon & Pakes; Maddi& Khoshaba Name it: Burnout • Burnout is “the index of dislocation between what people are and what they have to do.” (Maslach & Leiter, 1997) – – – – High Depersonalization (“hardened, withdrawn”) High Emotional Exhaustion (“drained”) Low Personal Accomplishment. (“ineffective”) Major contributor: Unsupportive work environment. (Siebert critique: worker factors underrepresented in Maslach Burnout Inventory.) – Gradual, predictable. “Progressive loss of idealism, energy & purpose…as a result of work conditions.” (Edelwich & Brodsky, 1980) – Relief occurs with vacation or job change. December 2, 2007 ©Elizabeth A. Pector, M.D. 8 Burnout • 6 main components of burnout (Maslach & Leiter, 1997) – – – – – – Overload Lack of control Too little reward Unfairness Value conflict Lost sense of community at work • Management can work with employees to: – Increase engagement, involvement, effectiveness & hardiness (Maslach & Leiter, Judkins & Furlow). December 2, 2007 ©Elizabeth A. Pector, M.D. 9 Name it: Compassion Fatigue • Compassion fatigue is “the cost of caring” (Figley) also called: Secondary traumatic stress, vicarious traumatization (Boscarino et al., 2004) – Less able to show empathy or bear clients’ suffering. (Boscarino 2004) – Exposure to & preoccupation with clients’ trauma. – Symptoms like Post-Traumatic Stress Disorder: • • • • Re-experiencing (flashback, memories, dreams) Avoidance (people, situations, feelings). Withdrawn, numb. Hyperarousal (startle, anger, vigilance, insomnia) See Figley 1995/1997 in handout, p. 2 • Compassion fatigue is related to clients’ experiences. Example: 9/11 social workers. December 2, 2007 ©Elizabeth A. Pector, M.D. 10 Compassion fatigue model December 2, 2007 ©Elizabeth A. Pector, M.D. 11 Maladaptive stress response (Vachon & Pakes, 1984) • Physical: fatigue, headache, insomnia, abdominal pain, diffuse aches, frequent viral illness, increased sick days, weight and appetite change, lack of exercise. • Psychological: depression, frustration, denial, anxiety, conflictladen dreams, over-identification with patients, anger, projecting blame onto others, awareness of own vulnerability, substance abuse, feeling robotic (unable to feel anything), unresolved grief for patients • Social: Bringing job stress home, changed libido, fear of pregnancy, fear for family member’s health, no time for friends or no friends outside work, conflict between job and personal life. • Occupational: Unrealistic expectations (science can cure everything, humans can be perfect), more & more time at work, feeling overwhelmed by job, inability to detach from job, overinvolvement with clients outside work, cynicism (insults, morbid jokes, dehumanizing attitude), role ambiguity (trouble defining one's duties and area of responsibility), decreased job satisfaction, role reversal with clients (they become your therapist). December 2, 2007 ©Elizabeth A. Pector, M.D. 12 Danger! Compassion Crisis • It is a crisis when you experience or practice: • • • • – Repeated errors and omissions – Drug or alcohol abuse – Numb, robotic functioning – Feeling suicidal, useless – Abusing patients – Blaming & criticizing other team members – High absenteeism – Tardiness Compassion Fatigue/Burnout are contagious to coworkers, family. It is not a sign of failure to realize you need a break, or a change! Consider transition to less stressful situation that uses your talents Treatment – CBT more effective than relaxation or multimodal intervention in stress reduction for all occupations (including non-health care) -van der Klink et al, 2001 – CF/PTSD: trauma-focused cognitive behavioral therapy (CBT), exposure-memory/site, stress management, EMDR. Debriefing controversial, may harm. December 2, 2007 ©Elizabeth A. Pector, M.D. 13 Name it: healthcare workplace stress Job Demands (General) Workload Shift work Limited worker control Technology Client demographics (age, culture) Organizational Factors Role demands Management style Career security Interpersonal relations Change Physical Environment Space, noise, heat, cold, lighting December 2, 2007 Health care (Specific) Work overload, paperwork Shortage of staff Shifts/schedule issues, overtime Lack of control Patients older, sicker, and heavier Management style, culture Lack of supervisor & peer support Work not valued, low salary Lack of advancement options Fear of errors Conflict with coworkers, pts., staff Moral dilemmas, death, dying Risk of violence at work Work environment in disaster response “Fishbowl” in ICU Isolation (lab, dietician, SW, rural) ©Elizabeth A. Pector, M.D. 14 Work factors by occupation • Physicians: (Spickard et al., 2002) – Work overload • Drop in payment, insurer business practices, regulations. – – – – – – Family/personal life suffer: medicine is put first, family “later.” Isolation: i.e. rural solo physicians. Worries: Money, Medicare/Medicaid audit, Malpractice, errors. More control less burnout risk. Management, leadership style, organization culture Male doctors: Poor childhood or poor father relationship more burnout risk. – Female doctors: more likely than males to burn out. • Greater risk with more hours worked; risk of sexual harassment – Personality: compulsive, doubt, guilt, sense of responsibility December 2, 2007 ©Elizabeth A. Pector, M.D. 15 Work factors by occupation • Pharmacist 67% satisfied with job; 68% have stress. – – – – – – – – – – – Stress greater in chain, mass merchandise, hospital (Mott et al 2004) More demand: increased workload (pts older, on more drugs) Interruptions Unqualified/inadequate staff, especially chain & hospital Undesirable schedules Less satisfied if too little time spent in pt consults/managing drug use. Work not valued; management/leadership style Fear of committing error Conflict with other professionals or non-clinical individuals Women more satisfied than men. Unmarried, female, nonwhite more likely to leave current setting • Gaither et al. J. Am Pharm Ass 2007;47(2):165-173. – Unmarried, low salary, no children, more time in filling rxs, more than 5 years experience: More likely for burnout in HMO setting • Gireesh et al, J Managed Care Pharm 1998:495-503 December 2, 2007 ©Elizabeth A. Pector, M.D. 16 Work factors by occupation • Pharmacy tech: Less stress than pharmacists – Excessive workload – Interruptions – Inadequate staffing – Work/life conflict, schedules. – Work not valued – Lack of advancement options – Support by supervisor is important • Instead of education on error avoidance, most pharmacists just pointed out error and asked tech to correct. Desselle Am J Health Syst Pharm 2005. December 2, 2007 ©Elizabeth A. Pector, M.D. 17 Work factors by occupation • Respiratory therapists/technicians – Work environment: stress in critical care, hospital floor, emergency settings. – Downsizing, roles assigned to others (e.g. nursing) – (Source: U.S. Dept. of Labor; AARC) • Registered dieticians: increased need expected – – – – – – – Most in hospital, nursing facilities & office Pay rate, overtime Inpatient consults, dying patients Monotony in patient types Noncompliance in patients (obesity, diabetes, others) Lack of respect, lack of contact with MDs. (Source: Dept. of Labor, posts on dieticiancentral.com) December 2, 2007 ©Elizabeth A. Pector, M.D. 18 Work factors by occupation • Lab technologists – In 2000, 7-20% shortage in positions (ASCP survey) – Work overload due to shortage, downsizing. – Excessive hours, paperwork – Lower sense of purpose with automation or changes in procedures – Monotony, boredom with repetitive tasks – Lack of management explanations for changes – Lack of control or input re: changes and work flow. – Fear of making mistake (e.g. blood bank) – Isolation from other health professionals • Martin B. Burnout in the lab: symptoms, stages, strategies, Medical Lab Observer 1986. • Maher Medical Lab Observer 1996 • Dowie et al. 2006 December 2, 2007 ©Elizabeth A. Pector, M.D. 19 Work factors by occupation • Radiology tech – Serious imbalance in supply/demand of techs – Better productivity with filmless systems…but there are limits. – Staffing shortage worst in rural/academic: especially general techs – Dropping morale – Inadequate compensation – Limited advancement options • Reiner et al, J Digital Imaging, 2004. December 2, 2007 ©Elizabeth A. Pector, M.D. 20 Work factors by occupation • Nursing: – 17% fewer RNs in acute care hospitals in 2005 than 2000 (Reineck & Furino) – Workload: pts. old, ill, obese. Paperwork, language. (Reineck & Furino) – Each added pt/nurse 23% higher risk of burnout & 7% higher pt. mortality. (Aiken 2002) – Inadequate/inexperienced staff & inadequate staff budget, agency RNs – Shift work (nights), overtime, & pressure to reduce “time on clock” – 12-hour vs. 8- or 10-hour shifts. Float/prn responsibilities – Fast pace not meeting pt needs or own expectations, fear of errors – Leadership/management style. – Professional/mgt/pt/family conflict – Lack of input in care, including moral distress/conflict – “Fishbowl” environment in ICU settings – Proximity to death and dying pts – Threatening/difficult/demanding pts (especially psych) – Lack of advancement options December 2, 2007 ©Elizabeth A. Pector, M.D. 21 Work factors by occupation • EMT/paramedic Risk of PTSD, physical & burnout symptoms – More job dissatisfaction & negativity toward pts, less physical distress, lower coping than nurses/doctors. High cortisol/catechol. – Physical symptoms, stress, +negativity higher with worker substance use. – PTSD increased with critical incidents: disaster, child, suicidal. • Risk of burnout increases with: – – – – Experience & age (greater experience/age more stress) Commercial service Work in poor areas high in violent trauma Low sense of coherence (confidence in predictability, manageability & meaningfulness of challenges). – Conflicts with ER personnel or poor communications w/ mgt. – Worry about work conditions, safety/health threats (crime, O/D) – Less support from supervisor & colleagues – Boudreaux & Mandy; Jonsson et al., vanderPloeg et al. December 2, 2007 ©Elizabeth A. Pector, M.D. 22 Work factors by occupation • Social work: 39% current burnout in N. Carolina – Work hours correlate with burnout • Staff cutbacks result in higher caseloads & work overload – Bureaucracy, funding limits, limited autonomy – Stressful clients, i.e. “underprivileged, socially maladjusted.” – Stressful environment • Hospital, child welfare workers have more stress-related symptoms • Proximity, identification, transference issues in disaster care • Discharge planning is hurried, too little time for counsel – Feeling responsible for clients • Unreasonable self-expectations to “do it all” – Personal history of troubled parent or childhood emotional abuse – Job isolation, lack of support. – Support from supervisors lessens stress socialworker.org, Lahad, Siebert, Felton. December 2, 2007 ©Elizabeth A. Pector, M.D. 23 Work factors by occupation • Clergy: 40% depressed or worn out; obesity, heart dz (Pector, 2005) – Emotional demands of role (baptism to funeral) • Compassion fatigue risk, “need to be needed” • Sometimes need professional help to learn to accept help – Pastor’s own communication difficulties – Client (congregational) conflicts or unrealistic expectations • If clients don’t have mental health insurance, they turn to clergy for help. – Workload: Less help than in past years from family, congregation – Lack of career control • Frequent relocation, occasional forced resignations – Isolation from peers • Denominations with strong, supportive tradition, e.g. Roman Catholic, fare better – Bureaucracy, budget, low salary – Lack of mentors, clinical pastoral education, counseling coursework – Lack of support for stressed pastors or their families December 2, 2007 ©Elizabeth A. Pector, M.D. 24 Name it: Worker factors in HCW stress • Personal traits – Age, partner/family status, race/ethnic, economic – Personality – Motivation • Gain knowledge, use technical skills, help or work with people • “Need to be needed” to boost self-esteem is a risk for work overload and CF • Talents & training – Innate abilities that are advantageous in job – Occupational training – Experience • Non-work stressors – Current personal stressors – Previous personal or job trauma or crisis • Buffer factors – Hardiness – Coping style – Social support December 2, 2007 ©Elizabeth A. Pector, M.D. 25 3. Reframe it: Hardiness A “personal protective factor” • Commitment: strive to stay involved – Engagement with job, effort to stay involved, even when times are rough – Worker believes work deserves full attention & effort. • Control: strive to influence outcomes – Worker perceives high degree of control in work role – Exerts influence thru imagination, knowledge, skill, choice. – We can’t control what happens; we can control how we respond. • Challenge: view as opportunity, not obstacle – Change is the rule, not the exception – React with openness, flexibility, innovation • Transform and grow in response to change • Don’t seek to preserve & protect the status quo December 2, 2007 ©Elizabeth A. Pector, M.D. 26 Reframe it: Hardiness A “personal protective factor” • Transformational coping: – – – – Put changes in perspective Realize you’re not facing change alone Learn what change means for you: worst/best case How can I take advantage of change? • Learn from past success & failure • Plan how to make best-case scenario happen • Social support—Maddi & Khoshaba – – – – Work with others, don’t alienate them Work toward constructive win-win solutions Believe that problems can strengthen relationships No matter what happens, don’t burn bridges. December 2, 2007 ©Elizabeth A. Pector, M.D. 27 Reframe it: Effective Coping Strategies • December 2, 2007 Brief COPE – Active coping – Planning – Positive reframing – Acceptance – Religion – Using emotional support – Using instrumental support – Self-distraction – Denial – Venting – Behavioral Disengagement – Self-blame – Humor (avoid ridicule, self-defeating) Blue: positive, Yellow negative Tan neutral ©Elizabeth A. Pector, M.D. 28 Think Reframe it: a new view • • Adopt a Hardy perspective – Commonplace: Others have experienced same stressors. – Manageability: The present is between the worst & best that could happen – Improvability: Think how YOU can improve situation. – Time: Estimate when stress will ease (e.g. short-term deadline stress) – Unpredictability: Do what you can, the rest is out of your hands. Attitude: Turn lemons into lemonade; “Attitude of Gratitude” – Cognitive behavioral therapy works to change thoughts, which in turn changes feelings & behaviors. Accentuate positive, reduce negative. – Live in the present moment (Mindfulness) – Adjust expectations. – Serenity prayer: change what you can, accept what you can’t. – Humor: shifts perspective to less threatening. ? Mixed effects in coping with health care stress. December 2, 2007 ©Elizabeth A. Pector, M.D. 29 4. Tame it: TWERPs revisited • Tasks: Do, Delegate, or Drop. • Time: Manage it & schedules. – Budget sleep and personal time! • Worries: Change what you can, Accept what you can’t, Know the difference. • Environment: Advocate positive change. • Events: Discuss critical incidents; Counseling. • Expectations: Change unrealistic to realistic. • Roles: Control responsibilities, Delegate tasks. • People: Assertiveness, Communication (with management & colleagues) December 2, 2007 ©Elizabeth A. Pector, M.D. 30 Tame it: Prepare, Self-care • Prepare for the expected and the unexpected. • Self-care: “Balance PIES” – Balance: Clear line between work and “life.” Set limits! • Work: – Improve protocols, build teams & communicate. – Maintain & upgrade skills. – Network with others, followup with clients at home. • Life: – Make time (prioritize) for friends, family, hobbies. – Relax, see nature, vacations, mental health days. – Limit off-work time with clients. – Physical: Diet, exercise, sleep, preventive care – Intellectual: Advanced education, change or add roles – Emotional: Self-acceptance. Counseling, meds as needed (anxiety/depression). Positive outlook, ? humor. – Spiritual: Morals, ethics, values, beliefs/religion, relax, meditate. December 2, 2007 ©Elizabeth A. Pector, M.D. 31 Tame it: Dare, Share, Be Aware • Dare to Dream, Decide, & Act – Meet with colleagues, research options – Approach management with suggestions • Share burdens with others – Social support, support groups F2F & online, professional help • Be aware – – – – Journaling helpful in coping with stress Ask others for feedback Monitor progress in personal wellness Stages of change model December 2, 2007 ©Elizabeth A. Pector, M.D. 32 Tame it: Dare Stages of Change for new/old habits December 2, 2007 ©Elizabeth A. Pector, M.D. 33 Tame it: Self-care Alternative individual strategies & effectiveness • Music (A)—patient’s preference • Aromatherapy (lavender) (B) – Essential oils in massage or in oil burner (check natural health/New Age shops) • Yoga in healthy people (B) • Relaxation techniques (B to C) many types – Autogenic training, breath therapy, guided relaxation, muscle relaxation techniques, Qi gong, self-hypnosis, visualization, biofeedback. • Massage, meditation, acupuncture, acupressure, guided imagery, therapeutic touch, other methods (C) A= strong, B= good, C= unclear evidence December 2, 2007 ©Elizabeth A. Pector, M.D. 34 Tame it: Relaxation (Natural Standard, 2007) • Goal: non-directed relaxation. 1) repetitive focus (on word, sound, prayer phrase, sensation, or muscular activity), 2) passive attitude towards intruding thoughts, and 3) return to the focus. • Deep methods: autogenic, progressive muscle relaxation (PMR), meditation ("thoughtless awareness," differs from relaxation). – Progressive relaxation: client taught how to relax by comparing relaxation with muscle tension. After months of practice, may evoke relaxation response within seconds. • Brief methods: self-control relaxation, paced respiration, and deep breathing. Require less time, often a short form of a deep method. • Applied relaxation: imagining relaxing situations, to induce muscular and mental relaxation. • Other techniques: guided imagery, deep breathing/breathing control, passive muscle relaxation, refocusing. • Instruction in hospitals, communities, books, audio/video, online December 2, 2007 ©Elizabeth A. Pector, M.D. 35 Tame it: Relaxation, Meditation Online training • allaboutdepression.com/relax/index.html (free, choice of techniques, no music) • healingchronicpain.org/content/relax/default.asp From Beth Israel. Guided Imagery. Choose type of imagery, male, female. • relax-online.com/imageryonline.htm (music, imagery, mind-body (progressive muscle) relaxation, breathing) • e-help.com/free_e-z_load_big_screen_relaxation_videos_online.htm • learningmeditation.com – http://www.learningmeditation.com/reduc1.htm • Healthjourneys.com: Free 15-min. guided imagery audio • Wilddivine.com Healing Rhythms: biofeedback hardware & sensors, $299.00. Andrew Weil demo wilddivine.com/content/HR_Demo1B_WD_QT384K.mov December 2, 2007 ©Elizabeth A. Pector, M.D. 36 Tame it: Biofeedback • Biofeedback amplifies small physiological signals (i.e. muscle tension, brain waves) and displays them to client in real time. • Client uses this information to learn to consciously change “subconscious” physiological functions (heartbeat, muscle tension, brain wave activity). (aapb.org) December 2, 2007 ©Elizabeth A. Pector, M.D. 37 Tame it: Types of biofeedback • EMG (forehead, upper back, other): For muscle tension backache or headache, neck pain, bruxism (grinding teeth). • Temperature (sensor on finger): For Raynaud’s, migraine. • Galvanic skin response (sweat): stress. • EEG (brainwave or neurofeedback). Attention deficit, anxiety. • Heart rate variability: the more variability, the better. IBS, asthma, non-cardiac chest pain. December 2, 2007 ©Elizabeth A. Pector, M.D. 38 Tame it: Biofeedback in action December 2, 2007 ©Elizabeth A. Pector, M.D. 39 Tame it: Biofeedback efficacy in stress-related disorders • Efficacious (Fourth level evidence): – – – – – • • • Anxiety Attention Deficit Disorder Headache- Adult Hypertension Temporomandibular Disorders Probably efficacious (Third level evidence): – Alcoholism/Substance Abuse – Arthritis – Chronic Pain – Insomnia Source: aapb.org quotation from Yucha C. & Gilbert C. (2004). Evidence-Based Practice in Biofeedback and Neurofeedback. More info: aapb.org, bcia.org. December 2, 2007 ©Elizabeth A. Pector, M.D. 40 Tame it: Share Therapy, e-therapy • Traditional counseling – Cognitive behavioral therapy – CBT/exposure/EMDR for traumatic stress • “Coaching” -- personal or professional • E-therapy Barak et al.: – Online therapy, via email, website programs etc. can be as effective as traditional therapy for anxiety & stress. No studies cited specific to work stress. – http://www.metanoia.org/imhs/ How to find a therapist online, cautions etc. Older info. – Ismho.org, onlineclinics.com December 2, 2007 ©Elizabeth A. Pector, M.D. 41 Tame it: Share Face-to-Face (F2F) & Online Groups Present in F2F & online: Unique online: • • • • • • • • Anonymity: Sense of community Empathy Information & advice exchange Self-disclosure Shared experiences Catharsis Learning from peers and mentors • Helper role • Advocacy December 2, 2007 – Filters nonverbal cues – Hides disturbing personal characteristics – Encourages prompt intimacy/deception • Writing is therapeutic • Lurkers: 75-95% of members lurk, yet learn & identify with group • Response is delayed (except in chats) ©Elizabeth A. Pector, M.D. 42 Tame it: Share Benefits & Risks of Online Groups • Convenient access • Decreased isolation • Increased perceived social support • Easier discussion of sensitive & controversial topics (sexuality, ethics, atypical lifestyle, suicide, end of life) • Practical help received • Ability to help others December 2, 2007 • • • • • • • • Misinformation Delayed treatment Alternative medicine focus “Meeting” severely affected peers Strong emotions, arguments Privacy/Identity Concerns Stalking Deception ©Elizabeth A. Pector, M.D. 43 Healthy systems Team problems, Team solutions “ …similar to shipmates preparing for a storm. Just as shipmates understand that the ship must be made with solid materials and fortified with necessary provisions, so does the NICU crew rely on structure, interdependent relationships, harmony and leadership in their preparation.” Reddick, Catlin & Jellinek, Crisis within Crisis: Recommendations for Defining, Preventing, and Coping with Stressors in the NICU, J. Clinical Ethics, Fall 2001. December 2, 2007 ©Elizabeth A. Pector, M.D. 44 What do healthy systems look like? • Structure: High level of function and effectiveness. – Multidisciplinary team • Mutual respect, cross-training, awareness of others’ roles. – Flexible schedules, with staff input. – Adequate staffing with independent, empowered staff. – Education, training & development: for tasks, leadership, & coping with stress • Relationships: Communication – All team members feel valued: Everyone’s opinions count. – Communication flows both ways: workers to administration. – Discussions after deaths, adverse outcomes, difficult clients • Critical incident debriefing controversial for emergency workers – Outside the hospital • Reunions, classes, support groups • Contact with community resources (visiting nurse, home health, hospice, community pharmacists) December 2, 2007 ©Elizabeth A. Pector, M.D. 45 What do healthy systems look like? • Harmony: – Workers have input into decisions, workload, work flow. – Error response seeks system improvement, not scapegoat • Leadership: – Management listens and responds to employees, – Management encourages risk-taking, trying new processes. – Policies don’t “handcuff” employees to protocols, & allow independent, innovative action. – Mentoring – Employee assistance programs (not enough by itself) – Consultants, organizational changes – Psychological training on attitude, communication & job stress relieve stress. (Marine et al. 2007) – Support and advice given by nurse managers or quality care coordinators decrease Depersonalization on Burnout Inventory. (Marine et al. 2007) December 2, 2007 ©Elizabeth A. Pector, M.D. 46 Healthy systems: Harmony in tough times • Discussions for deaths, errors, stressful cases, moral dilemmas – Team case review (doctors & others) • Focus on learning and improvement • Kudos for good care – Informal and formal discussions with peers – Sharing memories & feelings with families • Verbal and written: discharge, death, later • Tears & appropriate touch can be professional – Attend funerals for client death December 2, 2007 ©Elizabeth A. Pector, M.D. 47 Healthy systems: Forgiveness “ Perhaps the single most useful piece of knowledge …is…that more is unknown than can ever be known. ...A part of wisdom … is…that ignorance should be accepted and forgiven…The forgiveness of families, colleagues, and--most of all--ourselves becomes the cushion against crises and the guiding spirit to coping in a sea of chaos.” Reddick, Catlin & Jellinek, Crisis within Crisis: Recommendations for Defining, Preventing, and Coping with Stressors in the NICU, J. Clinical Ethics, Fall 2001. December 2, 2007 ©Elizabeth A. Pector, M.D. 48