crf - mcstmf
advertisement

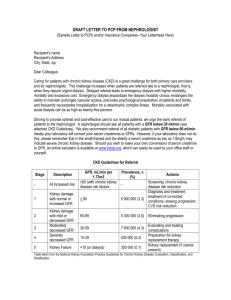
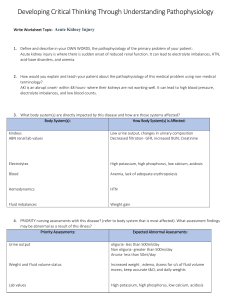
Acute and Chronic Renal Failure By Dr. Hayam Hebah Associate professor of Internal Medicine AL Maarefa College Objectives: O Definition O Classification O Signs and symptoms O Lab diagnosis O Complications O Management Function of the normal kidneys: -DETOXIFICATION of wastes. -ENDOCRINE FUNCTION: *Erythropoietin *active form of vitamin D *renin -BODY FLUIDS AND ELECTROLYTES REGULATION. Classifications O Acute versus chronic O Pre-renal, renal, post-renal O Anuric, oliguric, polyuric Acute Versus Chronic O Acute O sudden onset O rapid reduction in urine output O Usually reversible O Tubular cell death and regeneration O Chronic O Progressive O Not reversible O Nephron loss ACUTE RENAL FAILURE AKI: O It is sudden and usually reversible loss of kidney function which develops over days or weeks and usually accompanied by reduction of urine volume. O Rise of serum creatinine may be : ---acute injury ------acute on chronic kidney disease. Causes of AKI: O PRERENAL:-cardiac failure -sepsis -blood loss or dehydration. -vascular occlusion RENAL:- glomerulonephritis - interstitial nephritis. - small vessel vasculitis - ATN. - drugs , toxins, infections. POST RENAL:- stones -SEP -prostatic or cervical cancer -urethral valve or stricture or meatal stenosis. Symptoms of ARF: O c/p in volume overloaded patient . Pulmonary edema x-ray O c/p of O Dehydrated man with -Sunken eyes , -Dry mouth, -Loss of skin turgor , -oliguria Hyperkalemia symptoms: O Weakness O Lethargy O Muscle cramps O Paresthesias O Hypoactive DTRs O Dysrhythmias Investigations of patients with AKI: A. Confirmation of AKI: urea and creatinine. B. Complications:- electrolytes : k, calcium and phosphate - anemia: CBC -ECG C. Cause of renal failure: urine analysis, urine C&S, CRP, Abdominal u/s , renal biopsy. CPK D. Serology : HIV & hepatitis serology if urgent dialysis is indicated MANAGEMENT OF AKI: 1-Hemodynamic status :correct hypovolemia and optimise systemic hemodynamics with inotropes if necessary. O 2-Hyperkalemia : O Calcium gluconate (carbonate) O Sodium Bicarbonate O Insulin/glucose O Kayexalate O Lasix O Albuterol O Hemodialysis . 3- Acidosis: sodium bicarbonate if PH<7 4-Cardiopulmonary complications:( pulmonary edema): -dialysis - massive diuresis 5-electrolytes disturbance 6-fluid management : match intake to output (with 500ml for insensible losses). 7-discontinue nephrotoxic drugs and reduce dose of medications according to renal function level. 8- Ensure adequate nutritional support Treatment of any intercurrent infections. -PPI for reduction of upper GIT bleeding risk. O Treatment of the primary cause e.g steroids and immunosuppressives in cases of crescentic GN. O Surgical relieve of obstructions O Dialysis may be needed : - hemodialysis -CRRT. - Peritoneal dialysis. Chronic Renal Failure Stages in Progression of Chronic Kidney Disease and Therapeutic Strategies Complications Normal Screening for CKD risk factors Increased risk CKD risk reduction; Screening for CKD Damage GFR Kidney failure Diagnosis Estimate Replacement & treatment; progression; by dialysis Treat Treat & transplant comorbid complications; conditions; Prepare for Slow replacement progression CKD death Prevalence of CKD in the US according to different stages Stage Description GFR (ml/min/1.73 m2) 1 Kidney Damage with Normal or GFR 2 Prevalence* N (1000s) % 90 5,900 3.3 Kidney Damage with Mild GFR 60-89 5,300 3.0 3 Moderate GFR 30-59 7,600 4.3 4 Severe GFR 15-29 400 0.2 5 Kidney Failure < 15 or Dialysis 300 0.1 *Stages 1-4 from NHANES III (1988-1994). Population of 177 million with age 20. Stage 5 from USRDS (1998), includes approximately 230,000 patients treated by dialysis, and assuming 70,000 additional patients not on dialysis. GFR estimated from serum creatinine using MDRD Study equation based on age, gender, race and calibration for serum creatinine. For Stage 1 and 2, kidney damage estimated by spot albumin-to-creatinine ratio 17 mg/g in men or 25 mg/g in women in two measurements. Common causes of ESRD: Diabetes mellitus 20-40% Interstitial diseases 20-30% Hypertension 5-20% Glomerular diseases 10-20% systemic inflammatory diseases (SLE, Vasculitis) 5-10% Congenital and inherited 5% Unknown 5-20% Investigations in CKD: O Urea and creatinine O Urine analysis and urine quantification O K and PH O Calcium, phosphorus ,PTH and 25(OH)D O Albumin O CBC,IRON PROFILE O U/S O Hepatitis and HIV Acute Problems in CRF O Relating to underlying disease O Relating to ESRD O Dialysis related problems Problems Related to ESRD O Metabolic – K/Ca O Volume overload O Anemia, platelet disorder, GI bleed O HTN, pericarditis O Peripheral neuropathy, dialysis dementia O Abnormal immune function Dialysis O ½ of patients with CRF eventually require O O O O dialysis Diffuse harmful waste out of body Control BP Keep safe level of chemicals in body 2 types O Hemodialysis O Peritoneal dialysis CRF Indications of HD: O GFR<10ml/min O the uremic syndrome O hyperkalemia O acidosis O fluid overload Absolute Indications of RRT. HYPERKALEMIA II. ACIDOSIS III. FLUID OVERLOAD AND PULMONARY EDEMA IV. SEVERE UREMIA WITH PERICARDITIS V. UREMIC ENCEPHALOPATHY I. Hemodialysis: Peritoneal dialysis: Renal transplantation: Take home messages: O A great category of renal failure can be prevented with early diagnosis and proper Management .