Provider payment
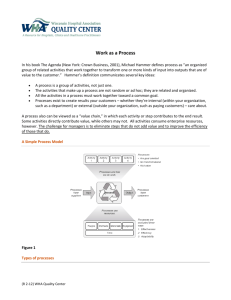
advertisement

Provider payment Dr Wai Hnin Aye Lecturer Community Medicine Field Training Center (Hlegu) Health Systems Goals • Better health outcomes • More responsive health system • Equitable health care Dr.WHA 2 Objectives of health care financing • Provide resources for health services • Ensure access to health care services • Ensure equity in health care coverage • Provide quality care • Provide efficient care Dr.WHA 3 Healthcare Financing comprise : 1.collecting revenue 2. Pooling of risk 3. Purchasing 4.Financial Protection Financial Issues in Healthcare System of Developing Countries • limited amount of financial resources in health care • distribution of resources is inequitable • gross inefficiency in management of resources • poverty is a major obstacle to access health care Dr.WHA 5 Reforms in the health care systems of developing countries focus on “getting the incentives right” Aim To use provider payments to optimize the utilization of scarce health care resources, transform clinical practice, and improve the quality of care Dr.WHA 6 Purchasing • Passive purchasing – No selectivity of providers – No quality control and monitoring – Use of norms to set fees and related concerns • Strategic purchasing – Performance-based model – Contestable contracts – Ongoing quality control and monitoring Dr.WHA 7 Who Purchases: Organizational Forms Government Private Sector Ministry of Health Insurer Regions Employer Social Insurance Managed Care Public Enterprises Organization (Insurance or Budget) Individual (Medical Savings Account) Dr.WHA 8 4 Performance Tools of Purchasing For Whom to Buy? ”Coverage decisions” What to Buy, in which form, and what to exclude “Benefits Package” From Whom, at what price and how much, “Contracting” How to Pay, and what incentives to meet, which policy objectives. “Payment method” Dr.WHA 9 provider payment method define as the mechanism used to transfer funds from the purchaser of health care services to the providers Dr.WHA 10 Why Payment Method is Important? Cost Containment Measures Efficiency Influence Provision of Services Incentives or disincentives Preventive vs Curative Services Basic Health Services Influence Quality of Care Technical Quality Client Satisfaction Viability of Health Financing Scheme Disbursement of funds Dr.WHA 11 Provider payment • focuses on providers’ incentives and behaviour also affect payers’ behaviour and consumers’ behaviour (pts’ ) • way they practice with regard to: – staff mix (technical efficiency) – choice of technology (technical efficiency) – choice of services (allocative efficiency) Dr.WHA 12 Provider Payment & Financial Risk • financial risk is the potential to lose money, earn less money, or spend more time or effort without additional payment on a reimbursement transaction • whenever providers or patients are bearing little risk, the system encourages higher levels of use of resources – e.g : OOP – Patient carries all the risk – Health insurance- Insurer carries the risk Dr.WHA 13 Payment Methods 1.Retrospective Payment 2.Prospective Payment Dr.WHA 14 Retrospective Payment - payment rate is selected during or after the service has been rendered - cost-based reimbursement - well known for being cost enhancing rather than cost reducing. • Fee-for-service • Payment per itemized bill • Payment per diem Dr.WHA 15 • fee-for-service (a typical form ) • but prices for each service set in advance, providers are not limited by predetermined agreement on the types and number of services rendered Dr.WHA 16 Prospective Payment payment rate for a package of health care services is negotiated and agreed upon before the treatment takes place Dr.WHA 17 • increase the incentive for efficiency • health provider faces higher financial risk These are• Capitation payment • Global budget • Case-mix payment Dr.WHA 18 Methods of Payments Physician Hospitals 1. Payment per procedure: Fee for Service 2. Payment per episode of illness 3. Payment per patient: Capitation 4. Payment per time: Salary 1. Payment per procedure: Fee for Service 2. Payment per day: Per Diem 3. Payment per episode of hospitalization: DRG 4. Payment per patient: Capitation 5. Payment per institution: Global Budget Dr.WHA 19 Current trends in Provider Payment System • Strategic Purchasing • Performance based system (payment linked to quality and out come) • Shift financial risks to providers • Bundling to avoid fragmentation • Reduce Admin cost Dr.WHA 20 Payment Models for PHC in Malaysia Health Centre / PHC Clinic Doctors / Providers Line Item Budget Fee-For-Service Global Budget Salary Patient Visit Salary plus Bonus Fee-for- Service Capitation Case-Payment Capitation plus Bonus Capitation Case payment Dr.WHA 21 Global Budget • is a payment fixed in advance to cover the aggregate expenditures of that hospital over a given period to provide a set of services that have been broadly agreed upon (at the hospital level) • based on either inputs or outputs, or a combination of the two Dr.WHA 22 • determine on the basis of historical costs (in Canada and Denmark) • incorporated measures of output, such as bed-days or cases, into global budgets for hospitals (France and Germany) • Ireland introduced a case-mix adjustment to global budgets for acute hospital services in 1993 • nearly all EU countries use case-mix adjustment Dr.WHA 23 Payment per Procedure: Fee-for-Service • traditional method of reimbursing physicians, hospitals and other providers for their services • provider is paid for each procedure or service rendered • each provided service associated with a corresponding fee to be paid to the provider • fees increase when more services are provided or as more expensive services are substituted Dr.WHA for less expensive ones 24 - may be either input-based or output-based • input-based if services are not bundled, and fee schedules are not set in advance • providers are permitted to bill payers for all costs incurred to provide each service(US) • called “retrospective cost-based” payment Dr.WHA 25 • output-based if fees are set in advance ( Canada, Japan, and Germany) • services are bundled to some degree • provider is paid the fixed fee for the predefined service regardless of the costs incurred to deliver the service Dr.WHA 26 - economic incentive to perform more services - overconsumption of care - not encourage physicians to consider the cost of the treatments they provide to their patients - their remuneration is not tied to patient health outcomes - in US, rapid rise in health care costs due to it Dr.WHA 27 • overwhelming reliance on FFS lead to source of inefficiency in the health system • physician expenditure is 2nd to hospital expenditure • to reduce health expenditures ,use alternative payment mechanisms capitation, fund holding (a more complete form of capitation), mixed payments, pay-for-performance and profit sharing Dr.WHA 28 Payment per Episode of Illness - payment by episode of illness or case - physicians have the economic incentive to reduce the volume of services provided per illness episode or case – transfers portion of the risk to the provider – eg : Appendicitis episode Dr.WHA 29 Payment per Patient: Capitation • insurer pays physicians a pre-determined fixed amount and paid in advance for each covered person regardless of the type and number of services used • physician is responsible for delivering or arranging the delivery of services of a contracted persons Dr.WHA 30 - shifts the financial risk from the insurer to the physician (If he incurs costs > per capita budget, he is liable for these costs) (if the provider achieves efficiency gains and incurs costs < per capita budget, the provider can retain and reinvest this surplus) Dr.WHA 31 • output-based • unit of output is coverage of all pre-defined services for an individual for a fixed period of time (one month or one year) • is not linked to the inputs the provider uses or the volume of services provided Dr.WHA 32 - physicians have incentives to limit the use of services and the use of expensive resources and services – rewards go to physicians who limit referrals, stay within formularies, lessen laboratory use and reduce average hospitalization Dr.WHA 33 Payment per Time: Salary • fixed annual payment unrelated to workload (one lump sum per month or yearly) • as theory ,salary d/on performance • in practice d/on yrs of service • no risk carried by the physician • Incentive undermine to work hard Dr.WHA 34 low income country, low salary leads to less work hard need more hours of work find additional ways of generating income (informal ways) Dr.WHA 35 Per Diem • incentive no: of hospital days, bed occupancy, and bed capacity • shifting outpatient and community-based rehabilitation services to the hospital • incentive to intensity of service provided during each bed-day • high occupancy rates are achieved by increasing hospital admissions and ALOS • incentive to ALOS > admissions( b/of ---incentive to inputs/day --- hospital days early in a hospital stay is more expensive than later in stay) Dr.WHA 36 • average per diem rate is easy and quick to calculate • = total historical annual hospital costs total number of bed-days • adjusted with characteristics of patients, clinical specialty and variations in casemix across hospitals Dr.WHA 37 • appropriate intermediate step for transition to a case-based system • administratively simple to implement • used to begin collecting the data that are necessary to design a case-based system Dr.WHA 38 Case-Based • incentives to no: of cases • to minimize the inputs used on each case (because providers have more control over resource use per case than the total no: of treated cases) • to control costs and reduce capacity in the hospital sector Dr.WHA 39 provider treats a patient with a broken arm -- for fee for service the provider is paid for each treatment ($40 for consultation, $25 per x-ray, and $35 for cast) -- in the case-based model the provider is paid a flat fee for the illness ($100 to fix a broken arm) Dr.WHA 40 Case-Mix (DRG) classification of patient treatment episodes designed to create classes which are relatively homogenous in respect of the resources used and which contain patients with similar clinical characteristics (George Palmer, Beth Reid,2000) Dr.WHA 41 Line Item Budget • allocation of a fixed amount to a health care provider to cover specific line items, or input costs for a certain period of time (e.g., personnel, utilities, medicines and supplies) • offer strong administrative controls, often valued by government-run systems Dr.WHA 43 • technical and allocative efficiency of health interventions by manipulating the government budget lines over time to increase delivery of cost-effective health interventions and decrease delivery of less cost-effective interventions • governments can track and understand the right combination to achieve these outputs • in reality, lack of good monitoring information Dr.WHA 44 Dr.WHA 45 Dr.WHA 46 Dr.WHA 47 Dr.WHA 51 • according to heterogeneity among health care providers, diversity of institutions, practices, and preferences ,health care systems in developing countries divides into 3 patterns • in Nepal, Tanzania, many of the smallest and poorest nations in sub-Saharan Africa • large public hospitals are in the capitals and a few in largest cities • smaller public hospitals, clinics, and health posts are scattered in rural areas Dr.WHA 53 • physicians and nurses are salaried • supplement their incomes by selling goods and services under the table • pt with varying severity crowd emergency rooms • little medical information is passed from one facility to another • shortages of supplies • in rural ,use traditional healers, drug sellers, and semi- trained health providers (they work isolated from the public facilities) • pay out-of-pocket or thin insurance market Dr.WHA 54 • 2nd pattern is as Pakistan and Kenya (poor countries with larger and more concentrated populations) • resembles the first with one exception: • semi-trained private providers dominate the supply of health care in most rural and marginal urban areas Dr.WHA 55 • private providers utilize a mix of Western and indigenous medical concepts • make money purchasing and reselling drugs from local chemists • engage in agricultural or other activities part time • limited contact with the formal, public health care system Dr.WHA 56 • pt are usually uninsured • out-of-pocket • about three-quarters of HE in India come directly from households Dr.WHA 57 • 3rd pattern is middle- income countries (Chile, Mexico, Thailand, South Africa) • risk-pooling (finance with formal sector payroll taxes) • government- managed social security organization collects taxes • pays physicians and hospitals(either public or contracted private providers) Dr.WHA 58 • general revenue financed hospitals and clinics for informal sector workers • growing or already substantial private insurance markets for the relatively well-off • many countries’ systems are hybrids, with different patterns Dr.WHA 59 payment methods may be used in combination to enhance or mitigate the incentives that are created by each method individually Dr.WHA 60 • • • • Reference Daniel Maceira, M.S:1998 . “ Provider Payment Mechanisms in Health care :Incentives, Outcomes, and Organizational Impact in Developing Countries “,major applied research 2, working paper 2 from www.phrproject.com (Accessed 2nd October 2011) JOHN C. LANGENBRUNNER, CHERYL CASHIN, AND SHEILA O’DOUGHERTY ,2009 ,“Designing and Implementing Health Care Provider Payment Systems How-To Manuals “ from www.rbfhealth.org (Accessed 2nd October 2011) Pierre-Thomas Léger ,2011, “Physician Payment Mechanisms: Overview and options for Canada” Canadian health service research foundation from www.chsrf (Accessed 2nd October 2011) Varun Gauri “Are Incentives Everything? Payment Mechanisms for Health Care Providers in Developing Countries” Development Research Group ,The World Bank Dr.WHA 61 h Dr.WHA 62