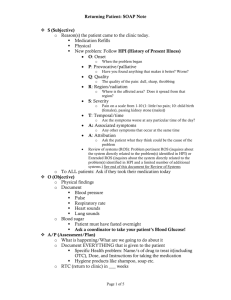
GENERIC NURSE PRACTITIONER Components of a SOAP Note
advertisement

GENERIC NURSE PRACTITIONER Components of a SOAP Note This is a generic SOAP note guide. Please refer to your specific course and faculty for the actual grading rubric and SOAP expectations. In general, please include all of the following in your SOAP note: Client ID Info: initials of client, age, gender, cultural heritage Chief Complaint [CC]: reason for visit in client’s own words or if a child, name historian, give their words, and identify the accuracy of the historian S History of Present Illness [HPI] If it is a well visit, inquire into any problems since last visit, for child--immunization status, developmental milestonesB for infant- formula amt./# night feedings/type or breast milk, solid food, water, and ask how the child is doing Symptom Analysis:: Include in order, going from general to specific for each symptom identified by the client. [Be specific; use as few words as possible to make point; use abbreviations where possible] =Bodily location of problem =What is the problem like? [Quality] pain/itching/felling is : sharp, dull, throbbing, stinging, gnawing Impact on life and activities Worries that led to seeking help =How bad is the pain? [Severity-Quantity] on a scale of 1-10, with 10 being the worst pain/itching ever had =Course/Timing: onset; duration; frequency =Setting in which problem occurs and does not occur =Aggravating &/or alleviating factors What makes it better or worse? =Associated manifestations =Include significant negatives =Medications, Allergies, Immunizations UTD? Screening tests? can be included here or at the end of PMH =For a child, include variables from the Child Sick List here =For an older adult, include SPICES (sleep disorders, problems eating/feeding, incontinence, confusion, falls in past 3 months, skin breakdown) PMH Family HH Identify illnesses, accidents, & problems. For GYN Hx. include parity & any problems during pregnancy. Social HH Include the following categories: Current situation [occupation, schooling, marital status, # of children & dependents, housing]-- Relationship patterns [sexual hx with hx of HIV risk factors such as STDs, # of partners, IV drug use, use of condoms, sexual preference] -- Daily routine [food/fluid intake-elimination, sleep pattern, habits, nutrition, exercise]-Community activities/Interests/Leisure Activities -- Spirituality/Religious preference Differential Diagnoses: List potential differentials now—you will rule them out as you progress and after the physical exam. ROS—you may not need to include any additional systems, as you may have covered the pertinent ones above. However, if there are additional ROS items not included above, you would include them here. Objective: Vital Signs & for children [include Ht with growth%; Wt with growth%] -- for Adults [Ht., Wt., & BMI] Each system in order goes next –this will be focused based on the presenting problem, HPI, and ROS. Not every body system needs to be included. You will have to determine which ones are appropriate based on your client’s presentation. Present lab data [Results available during visit, i.e., Hematocrit, wet prep, throat swab] Assessment/Plan Assessment =These are actual problems. Number these, 1, 2, 3, 4 starting with Acute self-limited problems then Chronic health problems. For each diagnosis, put the dx. Code (ICD-9 or ICD-10 as indicated. Plan =For each 1, 2, 3, 4, DX above, develop a plan it is easy for someone following you to understand your critical reasoning. See example below: 1. Hypertension: 401.9: DASH, weight loss, 30 minutes of walking 3 days a week, Lisinopril 10 mg po daily, #30, 2 refills, CMP in 3 months …etc. Here is where you will support how you ruled out your differential diagnoses. *After items 1,2,3, etc., ALWAYS end with RTC prn even if there is a specific appt. time =Be sure each plan is relevant to the client/family=s cultural heritage & spirituality--clearly identify this in each plan E Evaluation/Education/Anticipatory Guidance = Identify Health Maintenance Behaviors/Activities for each Dx. above = Identify Individual and Family Health Promotion Behaviors/Activities: For individual, family, and geriatric, put specific items here, including developmental issues For child, ADD Anticipatory Guidance & developmental issues Document patient education you provide. If you would have managed the encounter with the patient differently than what your Preceptor ordered, explain this at the end of SOAP note Support all your interventions with evidence-based guidelines or scholarly evidence and cite your sources in correct APA format.