4 - Becker's Hospital Review
advertisement

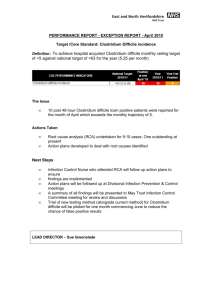
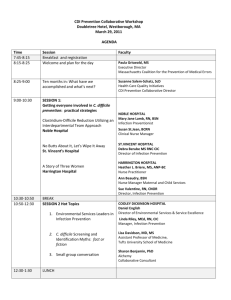
INFECTIOUS DISEASES STRATEGIES TO LIMIT HOSPITALIZATION,REDUCE RISK AND ADD VALUE Ronald G Nahass, MD, MHCM, FIDSA President – ID CARE Clinical Professor of Medicine-Rutgers University Robert Wood Johnson Medical School Disclosures Clinical Trial Support Gilead, Merck, Abbvie, BMS, Roche Advisory Board Janssen, Gilead Speaker Support Gilead, Merck, Vertex, Janssen Infection Prevention Contracts Somerset Medical Center, East Mountain Hospital, Bridgeway Care Center, University Radiology Objectives • Review the role of infection-related problems that lead to unnecessary admissions, readmissions, and avoidable complications • Discuss the cost from the fiscal and patient outcomes perspective • Illustrate the importance of the Infectious Diseases Physician – Hospital Partnership • Propose for consideration “The Infectious Diseases Service Line” Case Study: 72 Year Old Diabetic Woman Emergency Dept. Day 0 Presents with fever and painful, red foot Nursing Home Hospital Day 1 Day 2 Day 3 Day 4 Day 11 Day 12 Day 13 Day 14 After 12 days in hospital, patient discharged to Nursing Home Treated with broad-spectrum antibiotics Fever not better, Abx changed Develops diarrhea ID Called • Antibiotic treatment stopped as gout was diagnosed. • Clostridium difficile test ordered and treatment for this started. • Patient was isolated. • C difficile diagnosed. • ICU with dilated colon – operating room for colon resection. Case Analysis Emergency Dept. Day 0 Presents with fever and painful, red foot Potentially avoidable complication of antimicrobial therapy leading to lengthy stay Numerous antibiotics – most of which not needed Nursing Home Hospital Day 1 Day 2 Day 3 Day 4 Day 13 Day 14 After 12 days in hospital, patient discharged to Nursing Home Treated with broad-spectrum antibiotics Fever not better, Abx changed Develops diarrhea ID Called Late consultation with infectious disease Day 11 Day 12 • Antibiotic treatment stopped as gout was diagnosed. • Clostridium difficile test ordered and treatment for this started. • Patient was isolated. • C difficile diagnosed. • ICU with dilated colon – operating room for colon resection. Wrong initial diagnosis Prolonged recovery including sub-acute stay Key Take-Aways • Inappropriate diagnosis and treatment for infectious diseases is costly to the patient and system • Late consultation with ID specialist is costly Some Basic Statistics Keep 3 things in mind: 1. Infections can happen anywhere 2. Infections can be costly 3. Antibiotic resistance is a problem so Stewardship and Infection Control are critical Aggregate Costs Of Infectious Diseases • Clostridium difficile – nearly $9 Billion in annual costs Ref: Torio CM (AHRQ), Andrews RM (AHRQ). National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011. HCUP Statistical Brief #160. August 2013. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcupus.ahrq.gov/reports/statbriefs/sb160.pdf. Infection Related Health Care Admissions • Primary Diagnosis – – – – • Pneumonia Septicemia Complications of implant Skin and subcutaneous tissue infection Ranking* 1 4 7 9 What this could mean to you: – – 10% of your admissions may have an infectious disease diagnosis The number of admissions for ID related problems are almost 2x that of cardiovascular disease diagnoses * Ranking excludes pregnancy and psychiatry related diagnoses Ref: Pfuntner, A (Truven Health Analytics), Wier, LM (Truven Health Analytics), Stocks, C (AHRQ). Most Frequent Conditions in U.S. Hospitals, 2010. HCUP Statistical Brief #148. January 2013. Agency for Healthcare Research and Quality, Rockville, MD. Available at http://www.hcup-us.ahrq.gov/reports/statbriefs/sb148.pdf. Infection Related Health Care Re-Admissions • Primary Diagnosis – – – – – • Pneumonia Septicemia Complications of implant Skin and subcutaneous tissue infection Urinary tract infections Ranking* 1 4 8 9 12 What this could mean to you: – – 21% of your septic patients are likely to be readmitted within 30 days 20% of your patients with an implantable device or graft are likely to be readmitted within 30 days * Ranking excludes pregnancy and psychiatry related diagnoses Ref: All-cause 30-day readmissions ranked by the most frequently treated conditions* in U.S. hospitals, 2010 - Elixhauser A (AHRQ), Steiner C (AHRQ). Readmissions to U.S. Hospitals by Diagnosis, 2010. HCUP Statistical Brief #153. April 2013. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb153.pdf. Special Pathogens – Clostridium difficile • Clostridium difficile – Healthcare associated diarrhea infection related to antibiotic use – Adds an estimated $26,000 marginal cost per case to each hospitalized patient – Admissions nearly doubled from 2001-2010 - from 4.5 to 8.2 cases / 1000 admissions. – In 2009, C. diff accounted for a total of 336,000 admissions or 1% of all admissions – Estimated to have excess attributable costs of $1.3 billion Lucado, J. (Social & Scientific Systems), Gould, C. (CDC), and Elixhauser, A. (AHRQ). Clostridium difficile Infections (CDI) in Hospital Stays, 2009. HCUP Statistical Brief #124. January 2012. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb124.pdf Lucado, J. (Social & Scientific Systems), Gould, C. (CDC), and Elixhauser, A. (AHRQ). Clostridium difficile Infections (CDI) in Hospital Stays, 2009. HCUP Statistical Brief #124. January 2012. Agency for Healthcare Research and Quality, Rockville, MD. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb124.pdf NATIONAL SUMMARY ATA Estimated minimum number of illnesses and deaths caused by antibiotic resistance*: 2,049,442 23,000 At least illnesses, deaths *bacteria and fungus included in this report Estimated minimum number of illnesses and death due to Clostridium difficile (C. difficile), a unique bacterial infection that, although not significantly resistant to the drugs used to treat it, is directly related to antibiotic use and resistance: At least W Ant mo to and 250,000 14,000 illnesses, deaths WHERE DO INFECTIONS HAPPEN? Antibiotic-resistant infections can happen anywhere. Data show that most happen in the general community; however, most deaths related to antibiotic resistance happen in healthcare settings, such as hospitals and nursing homes. The Infectious Diseases Service Line Is A Solution • • • • • • Antimicrobial Stewardship Clinical Care Infection Prevention Microbiology Laboratory Employee Health Resource Management Antibiotic Overuse Is Dangerous and Costly • Studies indicate that 30-50% of antibiotics prescribed in hospitals are unnecessary or inappropriate. 1. Ref: http://www.cdc.gov/getsmart/healthcare/ 2. Anderson DJ, Moehring RW, Sloane R, Schmader KE, Weber DJ, et al. (2014) Bloodstream Infections in Community Hospitals in the 21st Century: A Multicenter Cohort Study. PLoS ONE 9(3): e91713. doi:10.1371/journal.pone.0091713 Antibiotic Stewardship Is Needed And the ID Specialist will be your champion Ref: Combes J.R. and Arespacochaga E., Appropriate Use of Medical Resources. American Hospital Association’s Physician Leadership Forum, Chicago, IL. November 2013 Stewardship Creates Value ID Specialists Improve Outcomes and Reduce Cost – Clinical Care Early ID Clinician Engagement for clinical care is critical to achieve the best outcomes Ref: Schmitt et al. “ Infectious Diseases Specialty Intervention is Associated with Decreased Mortality and Costs.” Clin Infect Dis. (2014) 58 (1): 22-28. doi: 10.1093/cid/cit610 First published online: September 25, 2013 Improving Outcomes and Reducing Costs • Infection Prevention Intervention Clostridium difficile at Rhode Island Hospital Metric 2006 2012 Incidence/1000 discharges 12.2 3.6 Mortality (N) 52 19 Results of a 5 step program focused on reducing the incidence of Clostridium difficile • C difficile infection control plan • Monitor morbidity and mortality of C. difficile • Improve test sensitivity • Enhance environmental cleaning • Standardize the treatment plan • Other interventions as necessary Mermel, LA et al, Reducing Clostridium difficile Incidence, Colectomies, and Mortality in the Hospital Setting: A Successful Multidisciplinary Approach. The Joint Com J 2013;39:298. ID Clinicians Offer A Unique System and Population Orientation • Long-term focus of risk reduction and safety through systemwide infection prevention and control efforts • One of the few specialties that focuses on efficient resource management, across various sites-of-service • Effective managers of patient care transitions – Employing Outpatient Parenteral Antimicrobial Therapy (OPAT) – Extensivist activity in LTC • Strong competency towards promoting team communication across all specialties and within the continuum of care The Infectious Diseases Service Line Is the Solution Clinical Care ID Specialist-led Interventions Efficient Resource Utilization Early ID consults Infection Control & Prevention Judicious use of radiology services, micro/lab services Rescue ID Antimicrobial Stewardship Hazardous waste (“red bag”) management Case Study – ID Rescue • 64 year old man has a total knee replacement. – • • Hospital has established TKR bundled payment agreement with payer 2 weeks later the patient has fever and drainage from the knee incision. A diagnosis of infected joint is made. Multiple treatment decision points, each with different cost implications Hospital Bundled Payment Total Knee Replacement Payer Option 1 – prolonged IV treatment and hope for the best $$ Option 2 – short course IV then long course oral treatment $$$ Option 3 – remove joint, IV treatment, replace joint $$$$$ There is a Better Way to Mitigate Risk Hospital Bundled Payment Total Knee Replacement Co-Management Agreement or Gain-sharing agreement with your ID Clinicians ID Services ID Specialist-led Interventions Efficient Resource Utilization Early ID consults Infection Control & Prevention Judicious use of Imaging/ Labs Rescue ID Antimicrobial Stewardship Hazardous waste management Clinical Care Payer Link payment to Quality: • Metrics for acute care – Antibiotic utilization – Resistant organism prevalence – C. difficile rates – CLASBI, CAUTI, SSI • Metrics for population management – Readmissions – Vaccination rates Strategies to Limit Hospitalization and Cost Without Sacrificing Outcomes • Acute infection diagnosis – Acute infection medical service • Out patient – Alternate site care • Early ID Consultation • Rescue care • Readmission – Focused programs on septicemia, pneumonia, UTI and surgical wound disruptions at LTC Case Study – Alternate Site Care • • 54 yo man with fever for 2 weeks had blood cultures performed by his doctor. He was seen by ID doctor because of long duration of fever. – – • • • Blood cultures positive for Streptococcus bacteremia. IV antibiotic treatment started as outpatient. Workup and treatment for endocarditis complicated as outpatient Total savings = $10,000 (Based on Millman and hospital per diem) Patient Satisfaction = High Risks = marked reduction for HAI ED/Hosp Option 1 – Send patient to ED $$$$$ Option 2 – OPAT and care management under ID $$ PCP Outpatient ID The Infectious Diseases Service Line • Is a solution for – Quality – Cost – Outcomes VALUE Final Key Messages Aligning incentives through gain sharing and co-management for the ID Service line provides a mechanism to achieve greater value Final Key Messages • If you are not engaged with your ID consultants you are missing opportunities to reduce risk and add value • If your ID consultants are not engaged with you then you have the wrong consultants THANK YOU! QUESTIONS or COMMENTS?