Behaviour Therapy & Cognitive Therapy
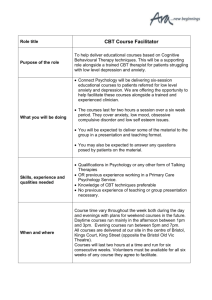
advertisement

Behaviour Therapy & Cognitive-Behaviour Therapy An Introduction for Psychiatric Registrars Frank McDonald Consultation-Liaison Psychologist www.fmcdonald.com The Townsville Hospital June 2002 Web V.02.6.22 Aims 1. 2. 3. 4. 5. Introduce theoretical premises of Behaviour Therapy & CognitiveBehaviour Therapy Describe behavioural case formulations - how they flow from a complete Behavioural Analysis & their value Describe a range of Behavioural & CBT treatments - ‘nuts & bolts’ of some psychological techniques Provide supplementary material a. b. c. therapist & pt written info material videos of strategies for mx of panic & depression (not on Web version) self-help & professional literature & Web references Check transfer of learning - discussion of medical practice case vignettes in which knowledge of strategies from learning theory based therapy may be helpful 2 BT & CBT Overview Click action button to advance to section 1. 2. 3. 4. 5. Paradigmatic bases of CBT & BT Distinguishing characteristics of CBT & BT Suitable disorders and problems Behavioural analysis – the etiological inquiry Survey of strategies for common conditions 3 BT & CBT Overview 6. Examples of specific behavioural strategies a. b. c. d. e. f. Exposure therapy for anxiety disorders Behavioural responses to panic symptoms Activity scheduling for depression Behavioural management of chronic pain Behavioural marital counselling Token economies for children 4 BT & CBT Overview 7. Examples of cognitive-behavioural strategies a. Anxiety b. Depression c. Pain 8. Your comment on how CBT & Behaviour Therapy may help with pt problems in some psychiatric practice scenarios 9. References & Resource materials 10. Credits 5 1. Theory And Paradigm Bases • Both therapies derived from Learning Theory and share some premises Pt’s problems are, at least in part, I. causally related to antecedent events, II. a result of reinforcing consequences, III. a result of dysfunctional thoughts or behavioural deficits. IV. And a pt’s condition is, at least in part, treatable by specific cognitive or behavioural techniques (Sperry et al., 1992) 6 1. Theory And Paradigm Bases • Both BT & CBT aim to modify or eliminate maladaptive • • thoughts, feelings and behaviours However their paths to this same goal differ (i.e. different therapeutic targets and rx strategies) Reflects differing paradigmatic bases 7 1. Theory And Paradigm Bases • Behaviourists say “change behaviour (&/or environment) • - changes in thoughts & feelings follow” Cognitivists say “change thoughts, images, etc (cognitions) - changes in feelings & behaviour follow” 8 1. Theory And Paradigm Bases 1. Conditioning paradigm – “experiences & action” Two subclasses Classical conditioning Operant conditioning 2. Cognitive-behavioural paradigm – “internal representation” For further discussion & examples see separate notes. Click here (Document links require a PDF reader.) 9 2. Characteristics of CBT & Behaviour Therapy What distinguishes Learning Theory based therapies? I. II. III. IV. V. Psycho-educational format Systematic measurement Individually-tailored, structured treatment ‘Home assignments’ Ultimate aim of self-management and self-control 10 3. Some conditions suitable for BT & CBT • Anxiety disorders • • • • • • • • • • (PD +/- A, OCD, GAD, PTSD, Social & Specific Phobias) Depression Chronic pain Social skills deficits Marital/relationship problems Sexual problems Children’s behaviour problems Eating disorders Habit disorders (e.g. sleep disturbances, smoking) Abnormal grief reactions Anger problems 11 4. Behavioural Analysis – The Etiological Inquiry • BT & CBT not just a bunch of routinely applied • procedures such as response prevention, exposure therapy, cognitive restructuring etc Good BT & CBT rests on thorough Behavioural Analysis of how problem began & why continues 12 4. Behavioural Analysis – The Etiological Inquiry • Behavioural Analysis – a search for all relevant • antecedents (recent & remote), concomitants & consequences – the ‘before, during & after’ contingencies More specifically, stimulus-response links – both personal (cognitions, autonomic & behavioural responses) & environmental – associated with problem. Guides therapy 13 4. Behavioural Analysis – The Etiological Inquiry • Analysis & therapy lie in the context of a supportive • relationship Despite apparent technical nature of BT & CBT, research says ‘warm’ therapists get significantly better results than ‘cold’ therapists. Even in more mechanical treatments like graded exposure therapy for phobias 14 4. Behavioural Analysis – The Etiological Inquiry • Irrespective of paradigm, behavioural analysis a sine qua non of learning theory based therapies • Hypotheses formulated about precise variables • controlling problem so as to suggest treatment. Reduces chances of ‘trial & error’ therapy Hypotheses tested by outcomes – reformulated if unsupported, loop-fashion, until success 15 4. Behavioural Analysis – The Etiological Inquiry • Treatment targets are specified in strict operational, • • measurable terms – not vague language like “less anxious” – a hallmark of behaviour therapies Treatment target options: change causes, change responses, change both or environment Changing environment often produces quickest, most efficient improvement in feelings 16 4. Behavioural Analysis – The Etiological Inquiry • Treatment is basically hypothesis testing of testable • constructs Click on links for ‘Behavioural Analysis’ notes for expansion and for example matrix to guide assessment 17 5. Survey of BT & CBT Techniques for Common Conditions • Anxiety – – – – – – – Breathing retraining Relaxation training Graded exposure therapy Flooding (rarely used) Response prevention (extinction) Cognitive restructuring strategies Structured problem solving 18 5. Survey of BT & CBT Techniques for Common Conditions • Anxiety (cont’d) • – Meditation – Assertiveness Training / Social Skills Training – Stimulus control – Eye Movement Desensitisation Reprocessing – Thought stopping To see how anxiety disorders are treated using psychological strategies on a disorder by disorder basis click here 19 5. Survey of BT & CBT Techniques for Common Conditions • Depression – Cognitive Therapy for ways of thinking common to depression (e.g. 3 P’s – ‘permanent, pervasive & personal’) – Activity scheduling – gradually increasing pleasurable and achievement events – Structured Problem Solving – Social skills training/Assertiveness training to increase social rewards – Consider involving family/partner in therapy 20 5. Survey of BT & CBT Techniques for Common Conditions • Habit Disorders/Addictive behaviours (e.g. Primary Insomnia, smoking) – – – – – – – Stimulus control Relaxation/ imagery/ autosuggestion Environmental changes Self-reward Self-monitoring Aversion therapy Saturation (extinction) 21 5. Survey of BT & CBT Techniques for Common Conditions • Social Skills Deficits – – – – – – – Behaviour modelling Covert modelling Behaviour rehearsal Role playing Assertiveness Training Social Skills Training (e.g. conversational skills) Communication Skills Training (e.g. listening, negotiation, conflict resolution) 22 5. Survey of BT & CBT Techniques for Common Conditions • Chronic Pain – – – – – – Goal setting Self-monitoring Pacing Graded physical conditioning Relaxation for any tension component Emotion defusing strategies (for frustration, anxiety etc) 23 5. Survey of BT & CBT Techniques for Common Conditions • Chronic Pain (cont’d) – – – – – Autosuggestion/self-hypnosis Structured problem solving Distraction (more suited to acute pain) Meditation Assertiveness Training (e.g. making/refusing requests given physical limitations) – Depression management strategies 24 5. Survey of BT & CBT Techniques for Common Conditions • Relationship Difficulties – Communication Skills training • Basic – Listening, validating, levelling • Intermediate – Assertiveness training • Advanced – Negotiation skills (win/win) Conflict resolution skills • Reciprocity counselling (quid pro quo agreements) • Miscellaneous – Token economies – Behavioural exchange contracts 25 6. Behavioural Strategies • A. Exposure therapy for Fear anxiety (used in OCD, PTSD, PD+A, Specific and Social Phobia) – Exposure to anxiety in graded fashion. Identify specific goals and break them into smaller, manageable steps Relax STOP Relax Relax Relax Relax STOP STOP STOP STOP Relax STOP The Principle of Exposure Therapy 26 6. Behavioural Strategies – Learn to master situations that cause mild, then gradually greater, anxiety. Teach & test a relaxation strategy before to reduce distress/panic during exposure – Aim is to achieve relative relaxation before next step Fear Relax STOP Relax Relax Relax Relax STOP STOP STOP STOP Relax STOP The Principle of Exposure Therapy 27 6. Behavioural Strategies • – Principle: best way to overcome fear is to face it, but in ways research says are more likely to succeed – Emphasise habituation to anxiety in each exposure session. Biggest trap is to flee a step at height of fear (re-forges association of situation & fear) – Confront fears regularly and frequently See ‘Exposure Therapy’ notes Click here for pt notes Click here for therapist notes 28 6. Behavioural Strategies • Example of graded exposure hierarchy for Agoraphobia or Social Phobia – Goal: To travel alone by bus to the city and back 1.Travelling 2.Travelling 3.Travelling 4.Travelling 5.Travelling 6.Travelling 7.Travelling one stop, quiet time of day (anxiety level 4/10) two stops, quiet time of day two stops, rush hour (anxiety level 6/10) five stops, quiet time of day five stops, rush hour (anxiety level 8/10) all the way, quiet time of day all the way, rush hour (anxiety level 10/10) 29 6. Behavioural Strategies • Some pts with Social Phobia may need assistance with • • developing social skills Click here for Conversational Skills material Click here for pt introduction to Assertiveness Training Click here for list of Assertiveness Techniques Click here for Conflict Resolution strategies Model & role play to aid generalisation (role play practice the core element of any social skill development) 30 6. Behavioural Strategies • B. Teaching behavioural responses to early symptoms of panic – After education about panic, pt’s breathing is retrained – Slow, steady breathing is central to controlling panic. Regular daily practice set up – Strategies applied at earliest symptom in selfmonitoring framework – Prof. Gavin Andrews on hyperventilation control. See References to purchase CD-ROM video via CRUfAD Web address – See pt guide ‘Panic Attacks!’ Click here 31 6. Behavioural Strategies • 1. 2. 3. 4. 5. • Videos below (Andrews & Hunt, 1998) on mx of panic in General Practice, demonstrate a learning theory framework & psychological research on the issue Patient presentation Assessing antecedents and consequences Psycho-educational phase Breathing retraining discussion & ‘homework’ assignment Behaviour rehearsal & real-world generalisation Videos not available on Web. See References for purchase details of complete clinical skills program on CD-ROM available via CRUfAD Web address in References 32 6. Behavioural Strategies • C. Behavioural management of depression Main psychological approaches – Cognitive Therapy (see CBT section) – Structured problem solving (see CBT section) – Activity Scheduling • Ask pt about recent frequency of activities that gave sense of pleasure or achievement – either or both often unusually low in depressed pts • Encourage achievable, gradual increases each day. • See list of suggested Pleasant Activities Click here 33 6. Behavioural Strategies • D. Behavioural management of Chronic Pain – Set specific adjustment goals. For suggestions on goal planning click here. Blank goal sheet - click here – Increase behaviours associated with adjustment to chronic pain. For guidelines click here and for more comprehensive guidelines on targets & rx’s click here – Baseline activity levels via pain diary. Raise or lower these according to principles of pacing. Click links for initial pain diary cover and follow-up diary cover and blanks for each day & evening of the baseline periods 34 6. Behavioural Strategies – Build stamina with appropriate exercise. Behaviourists start exercise below current capacities to avoid association with pain before habits established – Click links for movement guidelines & movement diary 35 6. Behavioural Strategies • E. Behavioural Marital Counselling – Reciprocity Counselling focuses on couples forming quid pro quo agreements about highly specific desirable changes by partner – Reciprocal agreements prevent either partner feeling any unfairness about change – Click links for guidelines & home monitoring sheets 36 6. Behavioural Strategies • F. Token Economy – Mainly for children & young adolescents – Makes a game of home discipline. Reduces emotionality of parents. Adds objectivity to task. Reciprocal control in that child can manage parent. Gets around imbalance of power problem in some behavioural programs – Fade to more natural contingencies as habits established – See example – Can be adapted to closed institutional settings i.e. where access to privileges outside closed system difficult See example 37 7. Cognitive-Behavioural Strategies • A. Cognitive Therapy for Anxiety – Explain cognitive restructuring to pts who potentially can ‘think about their thinking’ - role of specific thoughts, thinking styles & core beliefs. Supplement with info sheets / recommended reading Click here for samples – Teach strategies • Diary disputation / self-challenge of troublesome cognitions. Better than therapist persuasion, direct argument. Variation on role reversal strategy espoused by social psychologists for modifying attitudes. Model examples first using ‘thinking out loud’ 38 7. Cognitive-Behavioural Strategies • Click here for disputing tips, example & blank ‘Daily Stress & Tension Log’. • Cards with anti-worry statements / self-directions referred to regularly (principle of overlearning). Click here for example - ‘Coping with Worrying Thoughts’ and other ‘Managing Worry’ strategies • Reframing (alternative perspective taking). Examples: – “How would a reasonable person view same situation?” – Relate emotional reaction to point on a ‘Catastrophe Scale.’ Click here for pt info sheet 39 7. Cognitive-Behavioural Strategies • Thought stopping. Click here for description. Use with other ‘Managing Worry’ strategies • Powerful, brief coping self-statements pt believes to be true. Rapid, abbreviated form of earlier, more complex disputation e.g. “Feelings are not facts!” “Shit happens!” “Shouldhood is shithood!” “I’m musterbating again!” “I am a fallible human being who can therefore make mistakes, & some of them, big ones!” Click here for pt info sheet 40 7. Cognitive-Behavioural Strategies • Meditation (conditions switching off “what if?” thinking in GAD, “futurising” type problems) – Start with a one minute meditation exercise. Model out loud own multisensory awarenesses, moment to moment, free from any positive or negative judgments / adjectival speech – Pt tries same for similar period out loud initially & gradually increases time during repeated home assignments e.g. eventually long enough for hypnogogic phase of sleep to start 41 7. Cognitive-Behavioural Strategies • Guided Imagery. Used for relaxation, enhancing performance or imaginal confronting of avoided stimuli, obsessional cues, trauma recollections often in graded exposure fashion e.g. sees self extending travel radii from home – Can be intensified in hypnotic state or with associated cues e.g. vehicle crashes or aircraft sound effects recordings. Search Web for these 42 7. Cognitive-Behavioural Strategies – In confrontive applications, cognitive & somatic counter-conditioning imperative before pt leaves session. Otherwise in vitro exposure resensitises rather than desensitises – See Sleeping Better pt notes for example of relaxing Guided Imagery technique (‘Counting Down to Sleep’) 43 7. Cognitive-Behavioural Strategies • Distraction (GAD, acute pain etc not when extinction needed e.g. specific phobias, P.D.+A., PTSD) • Rational emotive imagery. Maultsby’s technique pts simply instructed to “push” themselves to feel better over a minute or so then articulate how they did it. (Usually with more rational thinking that provides starting point for further practice) 44 7. Cognitive-Behavioural Strategies • Structured problem solving (common skill deficit in worriers). Applied common sense. New variation on old “Think, judge, act” rule of conduct. Again see ‘Managing Worry’ pt info sheets pp. 5-6 • See Video examples (Andrews & Hunt, 1998) of structured problem solving with anxious pts on CDROM available via CRUfAD Web address in References 45 7. Cognitive-Behavioural Strategies • B. Cognitive Therapy for Depression – As for CBT for anxiety, explain cognitive restructuring for depression to pt. Role of specific thoughts, thinking styles & core beliefs. – Perhaps start with examples of common thinking styles seen in those more prone to depression e.g. Seligman’s 3P’s of adversity “permanent, personal & pervasive” as they apply to the cognitive triad of depression – future, self & the world 46 7. Cognitive-Behavioural Strategies – Supplement with info sheets / recommended reading. Click here for pt. info sheet on Ellis’s ABC model. Probably easiest of cognitive therapies for pts to understand. Info sheet focus: understanding & modifying specific thoughts associated with depression – Visit Albert Ellis Institute for more on Ellis’s Rational Emotive Behaviour Therapy – Work thru structured program material with pt. Keep demands low at first because of problems with concentration, lethargy etc. 47 7. Cognitive-Behavioural Strategies – Pt material on raising activity levels & modifying depressive cognitions from Oxford University Psychology Dept click here (Melanie Fennell in Hawton et al., 1989) • Structured problem solving for depression – Click here for single sheet description of technique. Present sheet to pt in session to aid application 48 7. Cognitive-Behavioural Strategies • C. Cognitive Therapy for Chronic Pain – Click here to see list of common thoughts & associated feelings that can worsen pain – Click here to see some suggested disputations of thoughts that can worsen pain 49 7. Cognitive-Behavioural Strategies – Cognitive therapy for self-defeating thoughts relies on usual strategies such as ‘diarying’ & disputation – Hypnotherapy (perhaps the oldest cognitive therapy) seen by many pts as useful. A daily ½ hour selfhypnosis session can provide a welcome break from constancy of pain Click here for list that includes other cognitive (& behavioural) pain mx strategies Click here for more details on cognitive treatment, targets, strategies & their rationales (go to page 6 for cognitive treatments etc) 50 8. Psychiatric Practice Scenarios: How Can Behaviour Therapy & CBT Help? • 1. As a psychiatric registrar you see many patients whose primary complaint is that they are "unable to sleep." Discuss the most common reasons for this presentation. How would you evaluate such a problem and how might you treat it using learning theory principles? (exclude ‘therapist modelling’ as per pic) 51 8. How Can Behaviour Therapy & CBT Help? • 2. Ms A is a 45 year old woman who presents at mid- morning to Emergency Dept. complaining of nausea and anxiety. She had been unable to sleep the previous night because she had run out of her usual sleeping tablets (Temazepam). She has been taking up to 4 tablets (10mg) nightly for several months as her insomnia had worsened. She had increased the dose herself as her doctor had refused to do so and she had resorted to visiting more than one doctor. She admits to being somewhat anxious and depressed in mood at times and to having difficulty concentrating on her work. She denies taking any other drugs. 52 8. How Can Behaviour Therapy & CBT Help? • 3. Describe and discuss the various treatments that are currently used in the treatment of Panic Disorder with Agoraphobia. 53 8. How Can Behaviour Therapy & CBT Help? • 4. You are treating a 45 year old man with chronic low back pain. He is requiring increasingly frequent pethidine injections and appears depressed and tearful. He says he can no longer cope with the pain. How do you approach this problem? 54 8. How Can Behaviour Therapy & CBT Help? • 5. A rather shy and introverted Engineering Student attends your outpatient clinic and tells you that he can't present his assignments in front of his seminar group. How can you as his psychiatric registrar help him? 55 9. Reference Material • Andrews, G. and Hunt, C. (1998) Counselling and Management Skills in Clinical Practice. (CD-ROM) Clinical Unit for Research of Anxiety Disorders (Web link next page for purchase), UNSW Psychiatry – St. Vincent’s Hospital, Sydney, NSW, Australia • Hawton, K., Salkovskis,P. et al.(1989) Cognitive Behaviour Therapy for Psychiatric Problems: A Practical Guide. Oxford University Press. • Sperry, L. et al. (1992) Chapter 4 ‘Behavioral Formulations’ in Psychiatric Case Formulations. American Psychiatric Press, Washington • Treatment Protocol Project (1997) Management of Mental Disorders. WHO Collaborating Centre for Mental Health and Substance Abuse, Darlinghurst, NSW, Australia 2010 56 9. Reference Material • Clinical Research Unit for Anxiety Disorders (CRUfAD) Website A UNSW site with excellent anxiety resources for pts and professionals. Free treatment manuals, CBT teaching resources, assessment protocols, self-test, CD-ROM, videos, links etc http://www.crufad.com/homepage.htm • MoodGym Excellent self-paced web program for behavioural & CBT of depression (mainly) and anxiety. Downloadable relaxation instructions and music http://moodgym.anu.edu.au/ 57