CBT in Palliative Care: Training & Techniques
advertisement

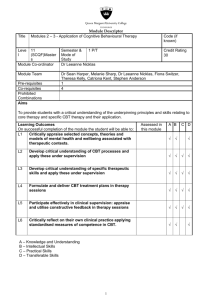
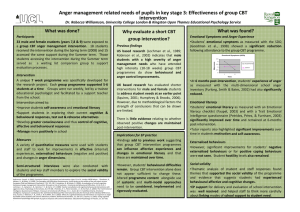
Training in Psychological Support: Using Cognitive Behavioural Approaches in Palliative Care Ms Clare Gadd Marie Curie Hospice Solihull Dr Iñigo Tolosa Pan Birmingham Cancer Network 1 Format • • • • A day a fortnight for Six Months Eight Hospice Staff (Ward & Community) Two or Three Trainers (Psychologists) Day Schedule: – Checking in: Progress and Obstacles – Teaching session – Joint Clinical Practice – Clinical Supervision • Follow up: 10 monthly refresher & SV sessions 2 Training on Cognitive-Behavioural Approaches in Palliative Care Teaching Session Relevant chapters Teaching Topics Session 1 Ch 1 & 2 Introductions; ‘norming, storming & forming’; Introduction to Cog Beh Theory; Relevance of CBT Session 2 Ch 4 Communication skills Session 3 Ch 5 & 6 CBT communication and Guided Discovery Session 4 Ch 7 Assessment; questions to ask; tools Session 5 Ch 8 Formulation Session 6 Ch 9-11 Intervention 3 From “CBT for Chronic Illness and Palliative Care: A Workbook and Toolkit”. Sage, Sowden, Chorlton & Edeleanu, 2008 Session 7 Ch 9-11 Goal setting; Step by step; Practicalities, problems Session 8 Ch 12 Bringing about change Session 9 Ch 13 Behaviour change; graded exposure; resistance, avoidance Session 10 Ch 14 & 15 Cognitive change; challenging unhelpful thinking Session 11 Ch 16 Managing emotions and unpleasant sensations Session 12 All Book Consolidation and Practice Session 13 All Book Preparing for Goodbye Session 14 All Book Endings & Saying Goodbye (Pros, Cons, Costs, Losses) 4 Cognitive Behavioural Approaches • Problem-oriented • Look at Emotions, Thoughts, Behaviours and Physiological Responses • Interpersonal • Related to cancer type • Psychoeducational – client taught cognitive model and shown how their thoughts contribute towards distress (homework) 5 6 Translating the Stages 1… • Assessment – what would you like to know? – How? – What questions do you need to ask to get the information? • Formulation – what is the problem/issue the patient wants help with – Why/when/how did it start? – Why is it a problem? – How is it maintained? 7 Translating the stages 2… • Tackling the problem: – Agreeing the goal/s or the desired change? – Setting the steps (SMART) • How /where/ what to bring about change – use the toolkit Which techniques? – Emotional focus – Cognitive focus – Or a mix? -- Behavioural focus -- Sensations focus • Constantly checking back – is this the right goal? How is it going? 8 9 10 11 • What might other useful questions be? 12 Cognitive Techniques for changing decision making • Breaking old cognitive habits • Distinguishing between intention and action • Commitment: – – – – Acceptance – of the problem Belief Pros and Cons Considering others’ views and reactions 13 Behavioural techniques • • • • • Relaxation training Activity scheduling Graded task assignment Planning for the future Behavioural experiments 14 Examples of clinical application A • Nature of Psychological Distress: • • Deterioration in Patient’s condition; and Feelings of loss of control over life. • HP’s Observations and Opinions of what was happening: • • Patient seemed to be in a vicious cycle of: thinking they were not in control → increased stress, anxiety, worry and hopelessness → sleeplessness → tiredness and loss of confidence → avoiding people and situations, becoming more withdrawn → feeling more out of control. • HP’s intervention: • Used Guided Discovery to explore what was causing most concern to the Patient. Worked together on plan for patient to regain more control with step by step approach. • HP’s Assessment of how the course helped this situation: • • Gave me the confidence to explore difficult issues with patients which I would not have done before. Helped me to think with patients about the thought patterns, behaviours and emotions, and perhaps to change them. 15 Examples of clinical application B • Nature of Psychological Distress: • • Patient felt she was letting her family down by being ill and imminently dying. Rift with one daughter, the other had disabilities and was in a residential home. • HP’s Observations and Opinions of what was happening: • Patient was tearful and expressed many regrets about her life and her desire to have changed things. Her anxiety brought on her pain. • HP’s intervention: • • Did a ‘hot cross bun’ with patient to explore links between thoughts, emotions, physiological sensations and behaviour. Patient was able to see the link between her anxiety and pain. Explored what patient wanted to do to change things with her estranged daughter. She expressed some thoughts and we made time to meet again. Unfortunately we were unable to revisit the issues because the patient’s condition deteriorated. • HP’s Assessment of how the course helped this situation: • • • Gave me confidence to explore painful issues. It felt okay that the patient was tearful. I was able to reflect that her feelings made her cry rather than me. I was able to use Guided Discovery and the downward spiral of unhelpful thinking. 16 Over to Clare... 17