Neuroradiology Neuropatholgy Conference, Dec 2010
advertisement

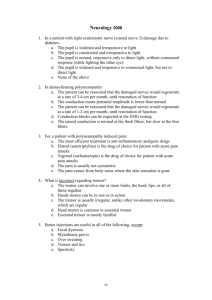
December 2010 Clinical Neuroradiology– Neuropathology Conference Patrick Farley, MD (Neuroradiology Fellow) and Thomas Bouldin, MD (Neuropathologist) Case #1 CLINICAL HISTORY: 59-year-old man with history of altered mental status and hearing loss. Differential diagnosis Infectious Meningitis Neoplastic Meningitis Breast, lung most common extracranial sources Most common primary brain tumors are GBM, medulloblastoma, pineal tumors, and choroid plexus tumors Neurosarcoidosis Lacy leptomeningeal enhancement May have ventricular or dural-based enhancing masses Brain biopsy revealed a poorly differentiated neoplasm within the leptomeninges and around several intracortical blood vessels. The immunophenotype of the neoplastic cells was consistent with a melanoma. The histologic features do not permit distinction between metastatic melanoma (common) and primary leptomeningeal melanoma (rare). Case #2 CLINICAL HISTORY: 21-year-old postpartum woman with a sellar mass. Differential Diagnosis Adenoma Pituitary hyperplasia 25–50% of females 18–35 years old have upwardly convex pituitary Usually < 10 mm unless pregnant, lactating Aneurysm Usually eccentric, not directly suprasellar Pituitary gland visible and identified as separate from mass Flow-related artifacts on MRI are common Meningioma Pituitary gland may be visible and identified as SEPARATE from mass Differential Diagnosis (continued) Metastasis Lymphocytic hypophysitis Can mimic adenoma clinically and on imaging studies May show zones of very low T2 signal peripherally Most common in peripartum female Craniopharyngioma Ca++, cysts more common, Children > adults Rim/nodular > solid enhancement May be indistinguishable from Rathke cleft cyst Biopsy revealed a dense lymphoplasmacytic infiltrate within the anterior pituitary. The gland also showed interstitial fibrosis and a loss of secretory cells. The remaining secretory cells form the clusters of larger, more eosinophilic cells in the photomicrograph. Lymphocytic hypophysitis Females > males, with a ratio of approximately 5:1 Often during last months of pregnancy or first few months postpartum Often have family history of autoimmune disease Sometimes associated with Hashimoto’s thyroiditis or Graves’ disease No adverse effect on fetus Presents as hypopituitarism and/or mass effect—headache or visual field cuts If unrecognized, may cause death from panhypopituitarism Treatment includes hormonal replacement and surgery to reduce mass effect. Lymphocytic hypophysitis Diagnostic signs: Thick non-tapered stalk, with or without pituitary mass Supra, intrasellar mass Areas of low T2 signal peripherally or/and in cavernous sinuses Usually < 10 mm but may be up to 2-3 cm Rounded pituitary gland with infundibulum that appears thickened, nontapering, or bulbous CASE #3 CLINICAL HISTORY: 73-year-old female with acute headache and right-sided weakness. Differential Diagnosis Hypertensive hemorrhage Deep structures (basal ganglia, thalami, cerebellum) but may also occur in cortex and subcortical white matter Hemorrhagic infarct Hemorrhagic metastases Cerebral amyloid angiopathy Beta Amyloid IHC Postmortem examination of the brain in this case revealed numerous cortical and leptomeningeal vessels infiltrated by amorphous, eosinophilic amyloid. Inset shows the immunohistochemical staining of the amorphous material for beta amyloid. Cerebral amyloid angiopathy (CAA) Deposition of beta amyloid in cortical and leptomeningeal vessels Common in older patients Often associated with Alzheimer’s disease Complications of CAA include intracerebral lobar hemorrhage, microbleeds, subarachnoid hemorrhage, cerebral infarcts, inflammatory CAA, and whitematter abnormalities. CAA Imaging Look for: Lobar hemorrhage(s) of different ages Multifocal areas of susceptibility artifacts corresponding to chronic microbleeds, particularly in cortex Hemorrhage may extend to subarachnoid space or into ventricles Acute lobar hemorrhage tends to be large Protocol advice: Recommend T2*-weighted sequence in all patients > 60 years of age Case #4 CLINICAL HISTORY: 65-year-old man with history of renal cell carcinoma first diagnosed in 1994. He has since had numerous surgeries for metastases to the brain. He also had stereotactic radiosurgery for an olfactory groove-based lesion, which was presumed to be a meningioma. Case #4 CLINICAL HISTORY (continued): A few months later the presumed meningioma developed surrounding edema, became larger, and demonstrated areas of different enhancement intensity and T2 signal. Biopsy of the olfactory-groove lesion revealed a meningioma (right half of photomicrograph). Also present within the meningioma was a focus of metastatic renal cell carcinoma (left half of photomicrograph). Tumor-to-tumor metastasis Metastasis of a systemic cancer to an intracranial tumor is rare. Most often, the CNS tumor is a meningioma. Other reported types of intracranial tumors harboring a metastasis include 8th-nerve schwannoma, glioma, hemangioblastoma, and pituitary adenoma. Breast and lung are the most common primary sites, with breast being the most common site. Renal cell carcinoma metastatic to a meningioma has been reported only rarely. Renal cell carcinoma may also metastasize to a hemangioblastoma in the context of the von Hippel-Lindau syndrome. Lanotte M, et al. Systemic cancer metastasis in a meningioma: Report of two cases and review of the literature. Clinical Neurology and Neurosurgery 111 (2009) 87–93. Case #5 CLINICAL HISTORY: 2-year-old AfricanAmerican girl with left eye strabismus for 9 months. Differential Diagnosis Retinoblastoma Calcifications, enhancement, mass of low T2 signal intensity Persistent hyperplastic primary vitreous Coat’s disease Retinal astrocytoma Rare; isolated or in association with tuberous sclerosis (TSC) Ocular toxocariasis PHPV Congenital Imaging Due to incomplete regression of embryonic ocular blood supply Best diagnostic clue: Hyperdense or hyperintense small globe, retrolental soft tissue, no Ca++ Retinal detachment common Central linear structure: Cloquet’s canal Layering blood or debris may be present PHPV is the most common intraocular abnormality to be confused with retinoblastoma The intraocular lesion is a small blue cell tumor with neuroblastic (Homer Wright) rosettes (arrows). The histological features of the tumor are typical of a retinoblastoma. Retinoblastoma CT: Calcified intraocular mass Unilateral in 70-75% MR: T2 Hypointense relative to vitreous Moderate to marked heterogeneous enhancement Best for assessing extraocular and intracranial disease