Phase III Randomized Study of Adjuvant Conventional
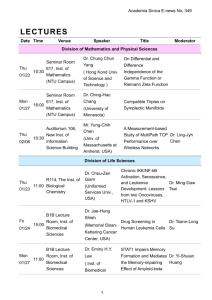
advertisement
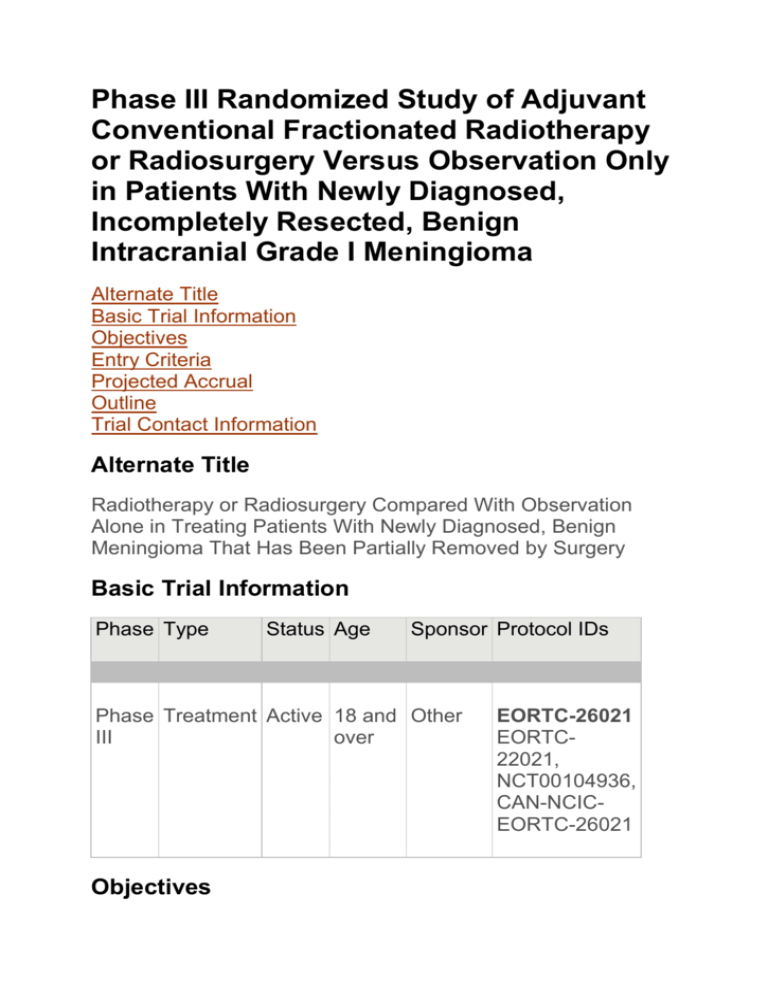
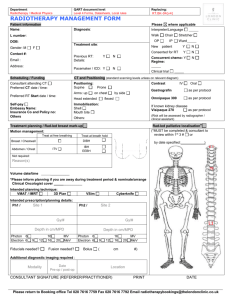
Phase III Randomized Study of Adjuvant Conventional Fractionated Radiotherapy or Radiosurgery Versus Observation Only in Patients With Newly Diagnosed, Incompletely Resected, Benign Intracranial Grade I Meningioma Alternate Title Basic Trial Information Objectives Entry Criteria Projected Accrual Outline Trial Contact Information Alternate Title Radiotherapy or Radiosurgery Compared With Observation Alone in Treating Patients With Newly Diagnosed, Benign Meningioma That Has Been Partially Removed by Surgery Basic Trial Information Phase Type Status Age Sponsor Protocol IDs Phase Treatment Active 18 and Other III over Objectives EORTC-26021 EORTC22021, NCT00104936, CAN-NCICEORTC-26021 Primary 1. Compare progression-free survival of patients with newly diagnosed, incompletely resected, benign intracranial grade I meningioma treated with adjuvant conventional fractionated radiotherapy or radiosurgery vs observation only. Secondary 1. Compare the quality of life of patients treated with these regimens. 2. Compare overall survival of patients treated with these regimens. 3. Compare the incidence of a second surgery in patients treated with these regimens. 4. Compare the incidence of acute and long-term neurotoxicity in patients treated with these regimens. Entry Criteria Disease Characteristics: Histologically confirmed newly diagnosed benign intracranial meningioma WHO grade I Any location except orbital meningioma Mitotic index < 4 (total counts per 10 high-power field) AND MIB-1 labeling index < 4% The following histologies are not allowed (i.e., WHO grade II or III): Atypical Clear cell Choroid Rhabdoid Papillary Anaplastic Must have undergone non-radical resection* within the past 7 months Post-operative MRI (performed 4 months after surgery) demonstrating stages 3, 4, or 5 [Note: *Biopsy only is considered non-radical resection and may be classified as stage 4 or 5 according to tumor volume] No brain invasion No hemangiopericytoma No fibrous dysplasia or intra-osseous meningioma No multiple meningiomas or meningiomatosis Not part of neurofibromatosis type II Prior/Concurrent Therapy: Biologic therapy Not specified Chemotherapy Not specified Endocrine therapy Not specified Radiotherapy No prior radiotherapy to the meninges or brain that would preclude study treatment Surgery See Disease Characteristics Other No prior randomization to this study Patient Characteristics: Age 18 and over Performance status WHO 0-2 Life expectancy Not specified Hematopoietic Not specified Hepatic Not specified Renal Not specified Cardiovascular No serious congestive heart failure Other HIV negative No other malignancy except basal cell skin cancer or carcinoma in situ of the cervix No other disease that would preclude 5-year follow up after study completion No psychological, familial, sociological, or geographical condition that would preclude study compliance or study follow up Projected Accrual A total of 478 patients (239 per treatment arm) will be accrued for this study within 3-4 years. Outline This is a randomized, multicenter study. Patients are stratified according to post-surgery MRI staging (3 vs 4 vs 5), skull base location (yes vs no), age (< 60 vs ≥ 60), and participating center. Patients are randomized to 1 of 2 treatment arms. Arm I: Patients undergo observation only. Arm II: Within 4-7 months after surgery, patients undergo conventional fractionated radiotherapy once daily, 5 days a week for 6 weeks OR a single treatment of high-dose radiosurgery in the absence of unacceptable toxicity. Quality of life is assessed at baseline, at 6 months after randomization, and then annually thereafter. After completion of study treatment, patients are followed at 3 and 6 months after randomization and then annually thereafter. Disclaimer The purpose of most clinical trials listed in this database is to test new cancer treatments, or new methods of diagnosing, screening, or preventing cancer. Because all potentially harmful side effects are not known before a trial is conducted, dose and schedule modifications may be required for participants if they develop side effects from the treatment or test. The therapy or test described in this clinical trial is intended for use by clinical oncologists in carefully structured settings, and may not prove to be more effective than standard treatment. A responsible investigator associated with this clinical trial should be consulted before using this protocol. Trial Contact Information Trial Lead Organizations European Organization for Research and Treatment of Cancer John Wolbers, MD, PhD, Ph: 31-10-463-2776 Protocol chair Email: j.wolbers@erasmusme.nl Raymond Miralbell, MD, Protocol co-chair Ph: 41-22-382-7098 Email: raymond.miralbell@hcuge.ch NCIC-Clinical Trials Group Rolando Del Maestro, MD, Protocol chair Ph: 514-398-5791 Email: rolando.delmaestro@mcgill.ca Luis Souhami, MD, Protocol co-chair Ph: 514-934-8040 ext. 43163 Email: luis.souhami@muhc.mcgill.ca Trial Sites and Contacts HOPITAL UNIVERSITAIRE ERASME (BRUSSELS, Belgium) - Inst. 131 CENTRE ANTOINE LACASSAGNE (NICE, France) - Inst. 218 CHU PITIE-SALPETRIERE (PARIS, France) - Inst. 233 ISTITUTO REGINA ELENA (ROMA, Italy) - Inst. 742 INSTITUT CATALA D'ONCOLOGIA (L'HOSPITALET BARCELONA, Spain) - Inst. 6225 MEDISCH CENTRUM HAAGLANDEN - WESTEINDE (DEN HAAG, The Netherlands) - Inst. 311 ERASMUS MC (ROTTERDAM, The Netherlands) - Inst. 336