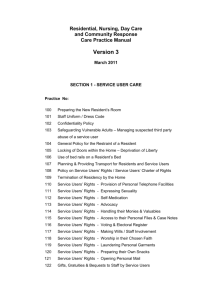
Resident and Family Groups
advertisement

Tammie Martin, MHA, CTRS Activities Director F249 (2) The activities program must be directed by a qualified professional who(i) Is a qualified therapeutic recreation specialist or activities professional who(A) Is licensed or registered, if applicable, by the State in which practicing; and (B) Is eligible for certification as a therapeutic recreation specialist or as an activities professional by a recognized accrediting body on or after Oct. 1, 1990; or (ii) Has 2 years of experience in a social or recreational program within the last 5 years, 1 of which was full time in a patient activities program in a healthcare setting; or (iii) Is a qualified occupational therapist or occupational therapy assistant; or (IV) Has completed an approved training course approved by the State. Activities F248 (f) Activities (1) The facility must provide for an ongoing program of activities designed to meet, in accordance with the comprehensive assessment, the interests and the physical, mental, and psychosocial well-being of each resident. 19CSR 30-85.032(93) The facility shall designate an employee to be responsible for the activity program. • The designated person shall be capable of identifying activity needs of residents, designing and implementing a program to maintain or increase, or both, the resident’s capability in activities of daily living. • Facilities shall provide activity programs on a regular basis. • Each resident shall have a planned activity program which includes individualized activities, group activities and activities outside the facility as appropriate to his/her needs and interests. (94) The facility shall provide and use adequate space and equipment within the facility for the identified activity needs of residents. (95) The facility shall establish and maintain a program for informing all residents in advance of available activities, activity location and time. 19 CSR 30-86.047(31)(A) The facility shall designate a staff member to be responsible for leisure activity coordination and for promoting the social model, multiple staff role directing all staff to provide routine care in a manner that emphasizes the opportunity for the resident and the staff member to enjoy a visit rather than simply perform a procedure. (B) The facility shall make available and implement self-care, productive and leisure activity programs which maximize and encourage the resident’s optimal functional ability for residents. The facility shall provide person-centered activities appropriate to the resident’s individual needs, preferences, background and culture. Individual or group activity programs may consist of the following: 1. 2. 3. 4. 5. Gross motor activities, such as exercise, dancing, gardening, cooking and other routine tasks; Self-care activities, such as dressing, grooming and personal hygiene. Social and leisure activities such as games, music and reminiscing. Sensory enhancement activities, such as auditory, olfactory, visual and tactile stimulation. Outdoor activities, such as walking and field trips. 7. Other social, leisure or therapeutic activities that encourage mental and physical stimulation or enhance the resident’s wellbeing. (C) Staff shall inform residents in advance of any organized group activity including the time and place of the activity. 19 CSR 30-86.043(57) Residents shall be encouraged to be active and to participate in activities. In a facility licensed for more than twelve (12) residents, a method for informing the residents in advance of what activities are available, where they will be held and at what times they will be held shall be developed, maintained and used. The changes to the interpretive guidance for F248/F249 reflects a shift in perspective to interpreting activities as they pertain to every facet of care that an individual who comes to skilled nursing care receives. The stated intent of F248 “facility is required to identify diverse interests of each resident and develop a program of care to meet those needs and interests. The mere development of a program is not sufficient for compliance.” The facility must promote care for residents in a manner and in an environment that maintains or enhances each resident’s dignity and respect in full recognition of his or her individuality. “Dignity” means that in their interactions with resident, staff carries out activities that assist the resident to maintain and enhance his/her self esteem and self-worth with grooming, dressing, and assisting residents to attend activities of their own choosing. Respecting private space and property (TV and Radio on to resident’s preference). Conversing with resident during cares. During group activities does the staff focus their attention on the group of residents or talk to other staff members instead? Are residents restricted from using common areas open to the public such as the lobby or common area restrooms? Do staff members respond to residents with a cognitive impairment in a dignified manner, such as not contradicting what residents are saying, and addressing what residents are trying to express (the agenda) behind their behavior. The resident has the right to— (1) Choose activities, schedules and health care consistent with his or her interests, assessments and plans of care; Both formal and self-directed activities Choice over their schedule—bedtime, bathing, therapy, attending activities, meals, etc…. Does the staff provide assistance as needed to the resident to be able to engage in their preferred activities on a routine basis? Does the facility assess to determine resident’s preferences regarding routine? (1) A resident has the right to organize and participate in resident groups in the facility; (2) A resident’s family has the right to meet in the facility with the families of other residents in the facility; (3) The facility must provide a resident or family group, if one exists, with private space; (4) Staff or visitors may attend meetings at the group’s invitation; (5) The facility must provide a designated staff person responsible for providing assistance and responding to written requests that result from group meetings. When a resident or family group exists, the facility must listen to the views and act upon the grievances and recommendations of residents and families concerning proposed policy and operational decisions affecting resident care and life in the facility. A resident’s or family group is defined as a group that meets regularly to: Discuss and offer suggestions about facility policies and procedures affecting residents’ care, treatment and quality of life; Support each other; Plan resident and family activities Participate in educational activities; or For any other purpose. If no resident or family group exits, has the facility tried to impede the formation of such a group? A resident has the right to participate in social, religious, and community activities that do not interfere with the rights of other residents in the facility. (both inside and outside of the facility) A resident has a right to— Reside and receive services in the facility with reasonable accommodations of individual needs and preferences, except when the health or safety of the individual or other residents would be endangered. Reasonable accommodations means the facility’s effort to individualize the resident’s physical environment, including bedroom, bathroom and facility’s common living areas. (Furniture, fixtures, task lighting to allow for resident’s chosen activities, and electronics) Staff should interact with the resident in a way that takes into account the physical limitations of the resident, assures communication, and maintains respect. For example: Getting down to eye level with a resident who is sitting. Speaking so a resident with limited hearing who reads lips can see their mouth when they speak. Utilizing a hearing amplification device such as a pockettalker. Move resident from a noisy area so they can communicate. Residents who use glasses, hearing aids or similar devices should have them in use, clean, and functional. Call light within reach. Adaptive equipment to participate in resident-preferred activities. The facility must provide for an ongoing program of activities designed to meet, in accordance with the comprehensive assessment, the interests and the physical, mental, and psychosocial well-being of each resident. The intent of this requirement is that: The facility identifies each resident’s interests and needs; and The facility involves the resident in an ongoing program of activities that is designed to appeal to his or her interests and to enhance the resident’s highest practicable level of physical, mental and psychosocial well-being. “Activities” refer to any endeavor, other than routine ADL’s, in which a resident participates that is intended to enhance his/her sense of well-being and to promote or enhance physical, cognitive, and emotional health. These include, but are not limited to, activities that promote self-esteem, pleasure, comfort, education, creativity, success and independence. (ADL-related activities, such as manicures/pedicures, hair styling and makeovers may be considered part of the activities program.) “One-to-One Programming” refers to programming provided to residents who will not, or cannot, effectively plan their own activity pursuits, or residents needing specialized or extended programs to enhance their overall daily routine and activity pursuit needs. “Person Appropriate” refers to the idea that each resident has a personal identity and history that involves more than just their medical illnesses or functional impairments. Activities should be relevant to the specific needs, interests, culture, background, etc. of the individual for whom they are developed. “Program of Activities” includes a combination of large and small group, one-to-one, and selfdirected activities; and a system that supports the development, implementation, and evaluation of the activities provided to the resident’s in the facility. The ongoing activity program should be based upon the resident’s individual needs and enhance their self-esteem and dignity. The activity program should match the skills, abilities, needs and preferences of each resident with the demands of the activity. The resident’s characteristics should also match the characteristics of the physical, social and cultural environments of the activity program. Daily life and involvement in activities should be meaningful. Activities are meaningful when they reflect a person’s interests and lifestyle. Bring enjoyment to that person. Help the person to feel useful. Provide a sense of belonging. Activities are relevant and valuable to our resident’s quality of life. Quality of Life=Dignity Dignity = Independence and Positive SelfImage Choice of Activities Activities that amount to something a. Activities that produce or teach something b. Using skills from resident’s former work c. Religious activities d. Activities that contribute to the nursing home e. Activities that require thinking f. Gender specific g. Allow for socializing with visitors and participating in community events. h. Physically active activities Complete an Activity Assessment to identify the resident’s interests, preferences and abilities. Use resident and family interviews to obtain information. Include the resident’s lifelong interest, spirituality, life roles, goals, strengths, needs, activity pursuit patterns and preferences. Identify any issues, concerns, problems or needs affecting the resident’s involvement/engagement in activities. What adaptations do they need? Activity Goals should be measurable objectives that focus on desired outcomes. For example: a. Engagement in an activity that matches the resident’s ability. b. Maintain attention to the activity for a specified period of time. c. Express satisfaction with the activity verbally or non-verbally d. Not merely a goal of attending a certain number of activities per week. The Care plan should also identify who is going to carry out the approaches. Examples: a. Notify resident of preferred activities. b. Transport residents who need assistance to and from activities. c. Provide needed functional assistance (such as toileting and eating assistance) d. Provide needed supplies or adaptations, such as obtaining and returning audio books, setting up adaptive equipment, etc. A continuation of life roles, consistent with resident preferences and functional capacity (e.g., to continue work or hobbies such as cooking, table setting, repairing small appliances) Encouraging and supporting the development of new interests, hobbies, and skills (e.g. training on using the internet) Connecting with the community, such as places of worship, veteran’s groups, volunteer groups, support groups, wellness groups, athletic or educational connections. Activities can occur at any time. Are not limited to formal activities being provided by the Activity staff. Includes activities provided by other facility staff, volunteers, visitors, residents and family members. All relevant departments should collaborate to develop and implement an individualized activities program for each resident. The facility may need to consider accommodations in schedules, supplies and timing in order to optimize a resident’s ability to participate in an activity of choice. Examples: a. Alter a therapy or shower schedule to make it possible for a resident to attend a desired activity. b. Assist residents to be ready to attend an activity (dressing, toileting, transportation) c. Provide supplies (e.g., books/magazines, music, crafts, sorting materials) for activities and assistance when needed, for residents’ use (e.g., during weekends, nights, holidays, evenings, or when the activities staff are unavailable) Time the administration of medications to avoid interfering with the resident’s ability to participate or to remain at a scheduled activity. (diuretics, incontinence, pain) Modify the administration time of pain medication to allow the medication to take effect prior to an activity the resident enjoys. Adapt for visual impairments: a. Provide higher levels of lighting without glare. b. Provide magnifying glasses c. Light-filtering lenses d. Telescopic glasses e. Use of “clock method” to describe where items are located. f. Describe sizes, shapes, colors. g. Provide large print items including playing cards, newsprint, books h. Audio books Adapt for hearing impairments a. Involve in small group activities b. Placement of resident near speaker/activity leader c. Use amplifiers or headphones. d. Decrease background noise e. Use written instructions f. Use of gestures or sign language to enhance verbal communication. g. Adapted TV (closed captioning, magnified screen, earphones) Adapt for physical limitations a. Use adaptive equipment b. Ensure proper seating and positioning c. Adjust placement of supplies and materials to enhance 1. visual interaction and to compensate for loss of visual field. 2. upper extremity function and range of motion (reach) 3. Hand dexterity (e.g., adapt size of items such as larger handles for cooking and woodworking equipment, built-up paintbrush handles, large needles for crocheting) 4. The ability to manipulate an item based upon the item’s weight, such as lighter weight for residents with muscle weakness. d. For the resident who has the use of only one hand: holders for kitchen items, magazines/books, playing cards; items (e.g., art work, bingo card, nail file) taped to the table; c-clamp or suction vise to hold wood for sanding. Task segmentation and simplification Programs using retained long-term memory, rather than short term memory. Length of activities based on attention span. Settings that recreate past experiences or increase/decrease stimulation Smaller groups without interruption One-to-one activities The length, duration and content of specific one-to-one activities are determined by the specific needs of the individual resident. Sensory Stimulation or Cognitive Stimulation a. Stimulation of the five senses (vision, hearing, touch, taste and smell) b. Reminiscing c. Validation Therapy-validate the feeling, not challenge the facts. Reminisce from that point. d. Special stimulus rooms like a Snoozylyn Room or sensory stimulation equipment e. Music f. Aromatherapy g. Stimulate the sense of touch with varying textures. Social engagement a. Directed conversation with staff or volunteer b. Initiate a resident to resident conversation c. Coffee and chat d. Pleasure walk Spiritual support and nurturing a. Daily devotion b. Bible reading c. Prayer with or for resident per religious requests/desires. Creative or Task Oriented Activities a. Music b. Pet visits c. Letter writing d. Word Puzzles Support of self-directed activity. a. Providing supplies such as reading material, craft supplies, setting up talking books, etc. Language Barriers Provide translation tools or a translator. Offer publications and/or audio video materials in the resident’s language. Offer spiritual support Relaxation programs Music Massage Aromatherapy Pet Visits Appropriate Touch For residents who are unable to leave their room or prefer to remain in their room: a. Provide in-room visits by staff or volunteers with similar interests/hobbies b. Sensory Stimulation activities such as appropriate touch, massage or aromatherapy c. Ensure access to art/craft materials d. Offer cards, games, reading materials e. Provide access to technology of interest (computer, DVD, hand held video games) f. Assist with preferred radio programs/stations g. Offer audio books h. Offer visits from spiritual counselors Ensure activities are available during awake time. a. Nursing staff reads with resident b. Dietary makes finger foods/snacks available c. CNA completes an activity with resident like working a puzzle, etc. d. Maintenance staff takes resident on night rounds. e. Individual or self-directed activity supplies are available and accessible. Develop ways to make your new residents feel welcome and are orientated to facility and routine. a. Welcome Committee b. Welcome packet c. Gift bag d. Who to contact in the facility for needs/questions. Short-stay residents may choose to not engage in the facility activities program. Offer “a la carte activities” that can be used when the resident desires. Examples may include books, magazines, cards, word puzzles, newspapers, CDs, movies, and handheld games. Offer engagement in small group activities such as dominoes, bridge, poker, movies, travelogues. Offer individual activities designed to match the goals of therapy, such as enhancing fine motor skills or cognition. Offer age-appropriate activities. a. Individual and group music offerings that fit the resident’s taste and era. b. Magazines, books and movies that fit the resident’s interests. c. Computer and internet access d. Contemporary group activities such as video games, playing musical instruments, card and board games and sports. e. Outings Accommodate and celebrate your resident’s diverse ethnic or cultural backgrounds. Plan special events that include meals, decorations, celebrations, or music from their culture. Arrange for visits from spiritual leaders and other individuals of the same ethnic background. Printed materials (newspaper and magazines) about the resident’s culture. Provide opportunities for the resident and family to share information about their culture with other residents, families and staff. Emphasis is on Person Centered Care, especially for residents with dementia. If a resident has dementia, the facility must: ~ Do everything possible to manage behaviors without medications. ~ Continual monitoring and documentation of the resident’s behaviors, medical conditions, and social situations. ~ Document all of the non-medication interventions tried and how they worked. ~ Document /describe how the behavior seriously impairs the resident’s quality of life. --Cynthia Hadfield, Pharm.D. Director of Pharmacy, Retail /Employee / LTC Pharmacies Lead Clinical Pharmacist, CMH Foundation The facility staff need to provide activitiesrelated interventions to try to minimize distressed behaviors. Care Plan these intervention. Document resident’s response to the interventions. Provide a space for the resident to walk safely. Provide environmental cues that encourage physical exercise, decrease exit behavior and reduces extraneous stimulation. For example: Provide seating areas spaced along a walking path or garden. Have an area that a resident may manipulate items such as a rummaging dresser or activity box filled with items to touch, fold, sort, stack, put on, etc. Provide a room with a calming atmosphere with music, lights, rocking chair, etc. A Snoezelen Room is a therapeutic environment created for the express purpose of delivering high levels of stimuli to patients with dementia. A room that displays optical illusions with combined lighting effects, aromas, colors, textures and sounds to stimulate a person’s olfactory, auditory and gustatory systems. Sensory therapy has proven effective in calming aggressive behavior and improving mood. https://www.youtube.com/watch?v=ZbiVadI7VGk The use of concentrated plant extracts for curative purposes, provides soothing sensory stimulation that may relieve agitation and boredom in elderly adults with dementia. Aromatherapy with lavender, rosemary, chamomile and other essential oils may temporarily relieve anxiety and emotional disturbances in elderly adults with dementia. Symptoms such as wandering, aggression and sleep loss increase the risk of injury in frail older adults who suffer from Alzheimer's disease or other neurological conditions that affect memory and cognition. Restoring a sense of calm may increase safety, improve quality of life and reduce stress on caregivers. More research is required to confirm the benefits of aromatherapy for elderly adults. As part of a comprehensive approach to medical treatment, aromatic essential oils may be inhaled or massaged into the skin to ease agitation and improve cognitive function in seniors. If you're planning care for an elderly person with dementia, consult a medical professional about the potential benefits and side effects of aromatherapy. Clinical evidence has not confirmed that aromatherapy is an effective treatment for dementia. Validate the resident’s feelings and words. Validation is a method of communicating with and helping disoriented very old people. It is a practical way of working that helps reduce stress, enhance dignity and increase happiness. Validation is built on an empathetic attitude and a holistic view of individuals. When one can "step into the shoes" of another human being and "see through their eyes," one can step into the world of disoriented very old people and understand the meaning of their sometimes bizarre behavior. Validation theory explains that many very old disoriented people, who are often diagnosed as having Alzheimer type dementia, are in the final stage of life, trying to resolve unfinished issues in order to die in peace. Their final struggle is important and we, as caregivers, can help them. Using Validation techniques we offer disoriented elderly an opportunity to express what they wish to express whether it is verbal or non-verbal communication. Validation practitioners are caring, non-judgmental and open to the feelings that are expressed. When disoriented elderly can express the things that have often been suppressed for many years, the intensity of the feelings lessen, people communicate more and are less likely to withdraw into further stages of disorientation. Validation is a theory that very old people struggle to resolve unfinished life issues before death. Their behavior is age-specific. Their movements reflect human needs. Validation is a way of classifying their behaviors into four progressive stages: ◦ Malorientation- Expressing past conflicts in disguised forms. ◦ Time confusion- No longer holding onto reality; retreating inward. ◦ Repetitive motion- Movements replace words and are used to work through unresolved conflicts. ◦ Vegetation- Shuts out world completely and gives up trying to resolve living . https://www.youtube.com/watch?v=ESqfW_kyZq8 Provide one-to-one visits with the resident. Look at photo albums or familiar pictures. Read to the resident. For the resident who engages in name-calling, hitting, kicking, yelling, biting, sexual behavior or compulsive behavior: Provide a calm, non-rushed environment. Provide a structured routine with familiar activities such as folding, sorting or matching. Use one-to-one or small group activities that provide comfort, such as music, walking quietly with someone, eating a favorite snack, looking at familiar pictures. Engage in exercise and movement activities. Redirect/exchange self-stimulatory activity for a more socially-appropriate activity that uses the hands, if in a public space. Residents who disrupt group activities with behaviors such as talking loudly and being demanding, or the resident who has catastrophic reactions such as uncontrolled crying or anger, or the resident who is sensitive to too much stimulation: Offer activities that help the resident feel successful. Break down activities into simple steps. Involve in small groups or one-to-one activities that are short and repetitive. Stop the activity if the resident becomes overwhelmed. Reduce excessive noise such as from the TV. Involve in familiar occupation-related activities. (Sorting supplies, helping deliver resident mail, snacks or juice, etc.) Involve in physical activities such as walking, exercise or dance. Play games or engage in projects that require strategy, planning and concentration such as model building. Engage in creative programming such as music, art or dance. Offer physically resistive activities such as kneading clay, sanding, scrubbing, stretch bands, or lifting weights. Offer slow exercises such as slow tapping, clapping or drumming; rocking or swinging motions. Don’t forget to try a rocking chair. Use normalizing activities such as stacking canned food onto shelves, folding laundry; offering sorting activities (sorting socks, ties, buttons, etc.) Involve in organizing tasks such as putting activity supplies away. Provide rummage areas in plain sight, such as a dresser or cart. Use non-entry cues, such as “Do not disturb” signs or removable sashes at the doors of residents’ rooms. Provide locks to secure other resident’s belongings if requested. Provide activities just before or after meal time in the dining room (so they are out of their room) Provide in-room volunteer visits, music or videos of choice. Encourage volunteer-type work that could begin in the room and needs to be completed outside of the room. Ask the resident to host a small group activity in their room. Engage in failure-free activities such as a simple craft or an activity with a friend. Invite to special events with a friend or family. Encourage resident to play a helping roll and assist another resident. Engage in activities that give the resident a sense of value such as intergenerational activities. Invite resident to participate on facility committees. Invite the resident outdoors. Involve in gross motor exercises to increase energy and uplift mood, such as aerobics or light weight training. Offer opportunities for leadership Involve in social programs Small group activities Service projects For the resident who lacks awareness of personal safety, such as putting foreign objects in his/her mouth or who is self-destructive and tries to harm self by cutting or hitting self, head banging, or causing other injuries to self: Observe closely during activities. Take precautions with materials. Involve in smaller group or one-to-one activities that use the hands such as folding, putting together PVC tubing) Engage in activities that are emotionally soothing, such as listening to music or talking about personal strengths and skills, followed by participation in related activities. Focus attention on physical activities such as exercise. When delusional and hallucinatory behavior is stressful to the resident: Focus the resident on activities that decrease stress and increase awareness of actual surroundings such as familiar activities and physical activities. Offer verbal reassurance, especially in terms of keeping the resident safe. Acknowledge that the resident’s experience is real to him/her. The outcome for the resident, the decrease or elimination of the behavior, either validates the activity intervention or suggest the need for a new approach. A friend is someone who knows the song of your heart and can sing it back you when you have forgotten the words. Moments of Joy are those little things that anyone can do to spark a memory, create a moment that makes you smile, leaving you with a happy feeling. What is that person’s greatness? What has brought that person great joy throughout their lives? Use these key topics to bring joy. All staff members can help make a resident’s day special, happy and comfortable. Feelings linger on……what was said was really not the point. A person with Alzheimer’s will lose their shortterm memory. Our goal is help them grasp memories from their long-term memory and create moments of joy. When you chat with them, don’t ask about what they had to eat for breakfast. Target the longterm memory and ask what they like to eat for breakfast….pancakes, biscuits and gravy? Instead of asking if their son came to visit, say something about their son….like “Your son is a wonderful kid, he looks a lot like you.” Spark that memory for them, leave them with a happy feeling. Because of their short-term memory loss they will repeat themselves over and over. Key in on the topics that elicit a happy memory for them and let them tell that story 100 times. When they are feeling sad, bring up that topic to help redirect them to that happy memory. There is no reasoning with a person who has Alzheimer’s and you will not be able to make them live your reality. Provide reassurance to their fears, their reality. This is the only disease where you can make mistakes as a caregiver all day long, because in five minutes they come around the corner and ask the same question. Keep changing your answer until you find the one that works. Once you find the answer, tell everybody, so moments of joy can be created all day long. Stop correcting them. Use distraction and redirection. “I’ve been looking for you! Let’s go get some coffee or cookies.” Before you correct them, ask yourself 3 questions. 1. Does it physically hurt you (the staff member) in any way for this behavior to occur. 2. Does it physically hurt any of the other people living here? 3. Does it physically hurt the person with dementia? If no one is getting hurt, let them do what they want to do. If you do need to take something away, replace it with something else. Leaving the person with nothing leaves a feeling of emptiness and loss. Find out from family members what the dementia person’s favorites are. Get specific information so you can focus on these things to create moments of joy. Favorite: snack, drink, nickname, temperature, chair, color, hair style, sweater, outfit, outings, music, stories, hobbies, best friends, travels, etc…. Find at least 20 things. Share the favorites list with staff and visitors. As Alzheimer’s disease progresses, the resident gets younger in their mind. Ask them how old they are to help you determine the best way to relate to them. Or observe what they are talking about to help you figure out their age. For example, if they are looking for their children but do not recognize them, they are probably in their younger adult years. If they are looking for their parents, they are probably in adolescence. Once you know what age, figure out what was significant in their life at that time and use those details to create moments of joy. “Everything is in the process of being forgotten. But who we are—who we have been in mood, in personality, in character—persists much longer.” --David Dodson Gray In the middle stages of Alzheimer’s, their developmental level is 8 years old and regresses to 5 years old. In the late stages of Alzheimer’s, their developmental level is age 3 or younger. As the disease progresses, their development regresses. An adult with dementia also loses inhibitions and say exactly what they are thinking. Their filter is gone. “No” becomes a common word for them as their developmental level regresses. A person with dementia needs structure and routine. Don’t forget to have a time for rest. A person with Dementia may not recognize their family members, but they have not forgotten them. Help reassure the family they have not been forgotten. Use pictures of the family during their younger years to help spark a memory for the resident. A dementia person will recognize a tone of voice far into the disease, but you have to get out of their sight in order for this to happen. Be the sunshine in the room. Your mood affects their mood. Radiate warmth, patience, smile. Be like a duck……relaxed, floating on the pond in the sun. Care free. But underneath we are busy paddling non-stop trying to get all of our tasks completed. Don’t let them see the busy paddling. Talk about everyday things…..spark a memory. Tell a joke. Help the resident engage in something of interest to them. Use touch and a calm tone of voice to reassure. Keep changing the way we respond to them until we find a way to create a moment of joy for them. Each day is a new day, we can keep trying to find what will touch them. Talk to them on eye level. Make eye contact. Compliment them. Say something to try to elicit a memory from them. Help them to relive one of their own simple pleasures. Don’t ask “How are you today?” Say something like, “I love your ___________ today. Simplify the task/activity until they can do it. Gives them a sense of purpose to do as much for themselves as possible. 90% of what a dementia person understands is body language, not the words that come out of your mouth. Be aware of your body language and send a positive message. Try a calm, gentle, matter-of fact approach. Reduce background noise. Position yourself directly in front of him, at his eye level, and make sure you have his attention before you start to speak. Touching a person on the shoulder or holding her hand may help her focus on what you are trying to communicate. Show a person what you are wanting him to do by demonstrating. Praise non-verbally through hugs, a caring smile, or a pat on the back. Walk away and try again later with a different approach. o o o o o o o o o o o o o Speak slowly in a low-pitched voice Enunciate your words Begin your conversation socially Use short, familiar words and simple sentences Talk in a warm, easy-going, pleasant manner Ask simple questions that require a choice of a yes/no answer. Listen carefully Give positive instructions and avoid “don’t…can’t” or negative commands. Avoid questions that require short-term memory e.g. :Did your daughter come to see you today?” Communicate using the person’s long-term memory: “I hear you have a wonderful daughter.” Give simple instructions for one task at a time (The simple task of brushing teeth contains 11 steps.) Keep talking to the person with dementia, even if he cannot talk back. The person with dementia may not understand your words, or be able to articulate their thoughts into words, but they do know how they feel right now. Respond to their emotion not their words. Listen actively and carefully Focus on a word or phrase that makes sense Respond to the emotional tone of the statement, not the words Stay calm and be patient Ask family members about possible meanings for words, names, or phrases Respond as though you understand Try a hug and change the subject Simply say Wow! Don’t argue with the person Don’t order the person around Don’t tell the person what he or she can’t do Don’t be condescending Don’t talk about people in front of them. People with dementia can hear, think, and feel emotions! Do not talk over, through, or about them as if they are not there. Avoid whispering because it arouses suspicion. Yelling into a person’s ear who cannot hear very well will only upset or frighten them. Get their attention before you start speaking to them. Compliment, Compliment, Compliment! Remind them who they are and give them their memories back. For example: Close your eyes ….and go back…..way back: Hide and seek at dusk. Sitting on the porch. Hot bread and butter. Penny candy in a brown bag. Hopscotch, kickball and Annie over! Cowboys and Indians. When around the corner seemed far away. And going downtown seemed like going somewhere. Being tickled to death. Playing slingshot and Red Rover. Climbing trees. Building forts. Running till you’re out of breath. Laughing so hard it hurts. Licking the beaters when your mom made a cake. Being tired of playing I will be here all day if you need anything. Don’t worry. I’ll take care of it. You are pretty important around here. If you need anything, just let me know. I do silly things like that, too. Between the two of us, we will be OK. You are a pretty special person. Wow, you are so smart! Thank you, I couldn’t have done it without you! That’s a good idea, I will have to try that! You always look out for me. Dementia resident may repeat, repeat, repeat themselves. Caregivers need to be patient, patient , patient. Distract rather than react. Use short, simple responses: “That’s interesting. You’re right. OK. I don’t know. Listen without judgment to give dignity. Affirm their conversation whether you agree or even understand what they are saying. www.enhancedmoments.com https://www.youtube.com/watch?v=NKDXuC E7LeQ Resident activities are everyone’s responsibility. Help your staff understand the significance in meeting the resident’s social and emotional needs, in addition to their physical and healthcare needs. Engaged residents are happier, less needy and are more fun to take care of and interact with. CNAs provide assistance to help the resident participate in desired group and individual activities by: Ensuring the resident is out of bed, dressed and ready to participate in chosen group activities and in providing transportation if needed. Provide any needed ADL assistance to the resident while he/she is participating in group activities. Help the resident to participate in individual activities such as set up equipment/supplies, positioning assistance, provide enough lighting and space for the activity. Help provide care planned activities for the resident at times when activities staff are not available. Ensure that the CNAs assist the resident in participating in activities of choice. Coordinate schedules for ADLs, medications and therapies to maximize the resident’s ability to participate. Make nursing staff available to assist with activities in and out of the facility. Try to identify and address the reason a resident is refusing to participate in activities. Coordinate the resident’s activities participation when activities staff are not available to provide care planned activities. Help facilitate resident participation in desired activities. Address the resident’s psychosocial needs that impact on the resident’s ability to participate in desired activities. Helps obtain equipment and/or supplies that the resident needs in order to participate in desired activities. Helps the resident access his/her funds in order to participate in desired activities that require money. Be aware of scheduled activities and talk it up! Encourage residents to attend activities. Offer to assist them to the activity. Engage in conversation, singing or story telling while you are in there completing your tasks. In their room, leave them with something to do. Would you like to watch TV, listen to the radio or talking books, look out the window, sit in the day area, work on an individual activity, hold their stuffed animal or doll, look at a magazine, work on a puzzle, get on the computer, etc…. Compliment the resident. Create a moment of joy! Schedule activities that involve your staff. These are easy to coordinate with National Nursing Home Week, holidays, special events. Staff are encouraged to participate, dress up, be a part of the fun! A little competition can be lots of fun and helps with team building. Seeing the staff get involved also helps motivate your residents to get more involved. Gives everyone a chance to connect on another level, laugh and have fun! Compliment staff for participation and engagement. Easter Parade and Easter Egg Hunt Pet Parade Trick-or-Treaters/Costume Contest Pumpkin Decorating Contest Golden Age Games Door Decorating Contest Theme Days/Dress up days Scavenger Hunt Celebrate National _____________Days Craft fair What are your employee’s talents? Would they be willing to share their talent? What groups, church, clubs, teams are your employees in or their family in? Would they be willing to come to the facility? What can you do to reward your staff for going the “extra mile” for your residents? Offer a treat to the staff who assist a resident to the activity. Coordinate an employee appreciation from the residents. ( Thank you card, treat bags, hearts and hugs, etc.) HEROES reward. When employees receive thank you notes from residents, families, visitors, peers they can earn points. When they reach 25 points, they receive a $25 check. We all need to feel like we make a difference. Rich Bluni says, "Engagement is actually a critical work skill wearing a fluffy disguise. It is the sense of feeling tuned into, a part of, a contributor to our calling and our mission." Acknowledge your staff’s important role at your facility. Make them feel like each person is a key player and appreciated. Recognition focuses primarily on performance or the achievement of certain goals. Appreciation focuses on the value of the individual. Take time to do both! Thank you notes from supervisor, peers, administration. Supervisors and Administration can mail thank you notes to their home, so their family can see their accomplishments too. Recognize Employee Birthdays. Recognize their anniversary with your facility. Team Build with Pot Luck luncheons. Coordinate Employee Secret Santas/Secret Pals. Recognize Departments during National Appreciation Days/Weeks. Employee Appreciation during the Holidays with a meal or party. Resident Welcoming Committee for new employees. Incorporate Personal Praise & Recognition Written Praise & Recognition Electronic Praise & Recognition Public Praise & Recognition Match the Reward to the Person Match the Reward to the Achievement Be timely and Specific When your employee’s groups come to the facility, try to get a picture in the paper or at least your newsletter and Facebook page. Recognize certifications, graduations, conference completions, etc….in your newsletters, on your bulletin boards, on Facebook, in the newspaper. Recognize your employee’s children, with permission, whenever you can. Also shows community support. The magic ratio of 5 positive interactions for every 1 negative interaction has been proven to improve productivity and satisfaction in the work place. --How Full Is Your Bucket? By Tom Rath and Donald Clifton, Ph.D. Everyone has an invisible bucket. We are at our best when our buckets are overflowing— and at our worst when they are empty. Everyone also has an invisible dipper. In each interaction, we can use our dipper either to fill or to dip from other’s buckets. Whenever we choose to fill other’s buckets, we in turn fill our own. 1. 2. 3. 4. 5. 6. 7. By what name do you like to be called? What are your “hot buttons”—hobbies or interests you like to talk about a lot? What increases your positive emotion or “fills your bucket” the most? From whom do you like to receive recognition and praise? What type of recognition or praise do you like best? Do you like public, private, written, verbal, or other kids of recognition? What form of recognition motivates you the most? Do you like gift certificates, a title for winning a competition, a meaningful note or e-mail, or something else? What is the greatest recognition you have ever received? Increases their individual productivity Increases engagement among their colleagues More likely to stay with their organization Receives higher loyalty and satisfaction scores from customers Better safety records and fewer accidents on the job How Full Is Your Bucket? Positive Strategies for Work and Life by Tom Rath and Donald Clifton, Ph.D. The spirit we have, not the work we do, is what makes us important to people around us. --Sister Joan Chisttister The Long Term Care Survey Manual Guidance to Surveyors Section V www.pioneernetwork.net www.culturechangenow.com www.quailitypartnersri.or www.edenalt.com