imaging of dysembryoplastic neuroepithelial tumors. a study of 6 cases
advertisement
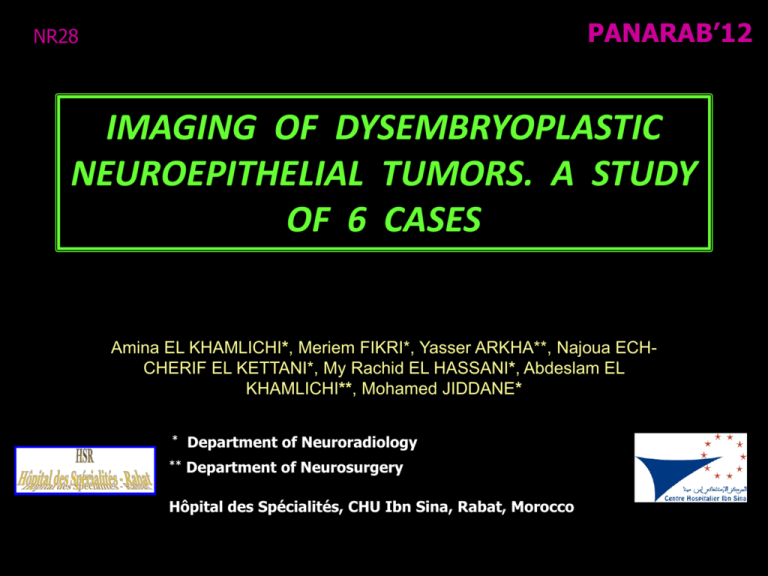
PANARAB’12 NR28 IMAGING OF DYSEMBRYOPLASTIC NEUROEPITHELIAL TUMORS. A STUDY OF 6 CASES Amina EL KHAMLICHI*, Meriem FIKRI*, Yasser ARKHA**, Najoua ECHCHERIF EL KETTANI*, My Rachid EL HASSANI*, Abdeslam EL KHAMLICHI**, Mohamed JIDDANE* * Department of Neuroradiology ** Department of Neurosurgery Hôpital des Spécialités, CHU Ibn Sina, Rabat, Morocco Introduction • Dysembryoplastic Neuroepithelial Tumors (DNTs) include a large morphological spectrum of tumors which histologically resemble gliomas but are carcinologically perfectly stable lesions. These tumors are seen in young patients with intractable partial epilepsy. • The purpose of this study is to evaluate CT and MRI features of dysembryoplastic neuroepithelial tumors . Materials and methods • Our study concerns 6 cases of dysembryoplastic neuroepithelial tumors histopathologically confirmed and diagnosed in patients who underwent corticectomies between 1998 and 2011. Table. Patient’s characteristics Characteristics No. of patients (n = 6) (%) 4 2 67 % 33 % 16 ± 15 6 – 26 2 4 33 % 67 % 5 0 1 83 % 0% 17 % Sex: Male Female Age: Mean (yr) Range (yr) Adults (> 16 yr) Children (< 16 yr) Histological forms : Complex form Simple form No specific form Materials and methods • Clinical symptoms : o Grand mal epilepsy (n = 2) o Pharmacoresistant partial seizures (n = 3) o Absence seizure (n = 1) o Symptoms beginning : * before age of 20 years : n = 4 * after age of 20 years : n = 2 o Symptoms of raised intracranial pressure (n = 1) o Neurological deficit (n = 0) Materials and methods • All patients underwent brain MRI and CT. • CT examination included axial and coronal sections before and after contrast administration. • MRI examination included T1 and T2 axial, sagittal and coronal sections both pre- and postcontrast. FLAIR were also utilised. Materials and methods • Studied parameters : Location and topography Signal on T1, T2 Contrast enhancement Calcifications and cystic component Size Limits Mass effect Peritumoral edema Results • In all cases a single focal supratentorial lesion on CT and MRI examinations • Location : * Temporal lobes (67%) : right (n = 3) and left (n = 1) * Right posterior parietal lobe (n = 1) * Left frontotemporal lobe (n = 1) Case 5 Case 6 Case 4 Case 3 Results • CT scan : * Hypodense lesion (n = 6) * ± Calcifications (n = 3) * Non-enhancing tumor or faint enhancement of solid portion. Case 2 Case 1 Case 4 Results • MRI : * Hypointense on T1-WI (n=6) * Hyperintense on T2-WI and Flair images (n=6) Case 2 Case 6 Results • Contrast enhancement : * Ring shaped (n = 3) * Nodular pattern (n = 2) * No enhancement (n = 1) Case 4 Case 5 Case 6 Results • Lesion pattern : * Pseudocystic, multilobulated (n=5) Case 6 Case 5 Case 4 Case 3 Results • Mass effect : Minimal (n = 2), absent (n = 4) • Peritumoral edema: Minimal (n = 1), absent (n = 5) Case 2 Case 3 Case 4 Discussion • 0.4 – 1.3 % of all brain tumors Histopathology : Specific glioneuronal element : columnar structure made up of bundles of axons lined by small tumoral oligodendrocytes. 3 histological forms : * simple : a unique specific glioneuronal element * complexe : - a specific glioneuronal element - a multinodular architecture - foci of cortical dysplasia * non specific : no specific glioneuronal element or multinodular architecture Discussion Imaging Three radiological features of DNT, not sensitive and not specific, are helpful for the diagnosis : • cortical topography • no « digit like » peritumoral edema • no mass effect CT scan: o Well-circumscribed hypodense lesion, which usually appears as non enhancing mass ± Focal enhancement in 21 % of cases ± Calcifications in 36 % of cases ± Pseudocystic aspect in 50 % of cases ± « Scalloping » o Brain CT was reported as normal in 10 % of cases (isodense small lesion) Discussion MRI +++: o T2 Weighted Images +++ o Tumor topography : cortex and/or subcortical white matter involvement o Hypersignal on T2 WI: 100 % o Polymorphic aspect : « nodular » (77%) or « megagyri » configuration (23%) o Tumor size : 8 – 60 mm o Microcystic pattern is common : « soap bubbles » appearance o True cyst is rare (7%) [size less to 1 cm] Discussion Imaging features according to the histologically forms : Simple form pseudo-cystic, well delineated, homogenous appearance with no calcifications or any enhancement after contrast examination Complexe form ring-like contrast enhancement, calcifications Non specific form nodular enhancement, « megagyri » pattern, calcifications Discussion Positive diagnosis : The diagnosis of DNT must be considered when the following criteria are associated : o MRI : intracortical lesion with no mass effect and no peritumoral edema o Histological feature resemble gliomas but without lymphocytic infiltrates o Partial seizures with or without secondary generalization o Symptoms beginning before 20 years of age o No neurological deficit or stable congenital deficit Differential diagnosis : * Ganglioglioma * Low grade oligodendroglioma Discussion Follow-up : * DNTs are carcinologically stable lesions * Absence of recurrences after total resection In our study, the mean follow-up was 21 months. One patient developed tumor recurrence appeared 2 years after incomplete primary resection Conclusion • DNTs is a recently defined category of tumors in young patients. These tumors histologically resemble gliomas but behave as stable lesions. MR imaging allows a better knowledge of their characteristic imaging features. • Three radiological features of DNT are helpful for the diagnosis: cortical location, absence of mass effect and no peritumoral edema. References 1. Stanescu Cosson R, Varlet P, Beuvon F, Daumas Duport C, Devaux B, Chassoux F, Frédy D, Meder JF. Dysembryoplastic neuroepithelial tumors: CT, MR findings and imaging follow-up: a study of 53 cases. J. Neuroradiol., 2011;28 : 230-240 2. Daumas-Duport C, Varlet P, Bacha S, Beuvon F, Cervera-Pierot P, Chodkiewicz JP. Dysembryoplastic neuroepithelial tumors: nonspecific histological forms – A study of 40 cases. Journal of Neuro-Oncology, 1999; 41 : 267-280 3. Daumas-Duport C, Scheithauer BW, Chodkiewicz JP, Laws ER,Vedrenne C. (1988). Dysembryoplasic neuroepithelial tumor: a surgically curable tumor of young patients with intractable partial seizure. Report of thirty-nine cases. Neurosurgery, 23: 545-556 4. El Kettani N, Sqalli-Houssaïni N, Sbihi S et al. Tumeur neuroépithéliale dysembryoplasique. Feuillets de Radiologie 2007;47(1):46-51 5. Litrico S, Desjardins T, Dran G et al. Localisation sous-tentorielle d’une tumeur dysembryoplasique neuroépithéliale. Neurochirurgie 2004;50(1):47-52 6. Rodrigo S, Chassoux F, Oppenheim C, Devaux B, Méder JF. Nouvelle approche sémiologique en IRM des tumeurs dysembryoplasiques neuroépithéliales. Journal de Radiologie, 2006; 87(10), Page 131 7. Ben Yaacoub I, Sebai R, Hammami N, Belghith L, Bellakhal J, Nagi S, Ben Hammouda M. Apport de l’imagerie dans le diagnostic des tumeurs dysembryoplasiques neuroépithéliales: à propos de 11 cas. Journal de Radiologie, 2007; 88(10), Page 1554