Management of Cancer Patients after Cancer Therapy
advertisement

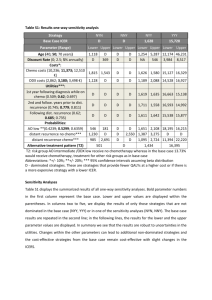
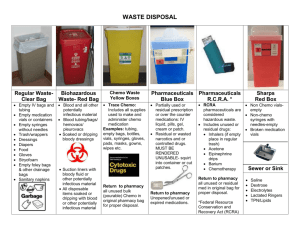
Management of Chemotherapy Complications Elshami M. Elamin, MD Medical Oncologist Central Care Cancer Center www.cccancer.com Wichita, KS - USA Introduction Chemotherapy: Affects the rapidly dividing cancer cells Also affects rapidly dividing normal cells Hair Mucous membranes Blood cells Effect of chemo on blood counts Because stem cells in BM do not reproduce rapidly they are less likely to be affects During hematopoiesis (differentiation) the blood cells are sensitive to chemo and most likely to be damaged After the mature cells (neutrophils, platelets) live out their life span, the blood count fall to THE NADIR What is the chemo nadir? Lowest blood counts following chemo The nadir time is usually about 10 days (7-14 days) after chemo It varies depending on the drugs Risk of infection and bleeding The next dose of chemotherapy is given only after: The nadir BM recovers (3-4 wks) Why chemo given in Cycles (q3-4 wks?) The nadir (7-14 days) BM recovery (3-4 wks) What if chemotherapy is given during BM recovering period (increasing stem cell production)? It may cause: Prolonged myelosuppression Permanent BM damage 10.0 W.B.C. 8.0 6.0 4.0 2.0 Day 0 (Chemo Starts) Day 7 Nadir Day 21 Chemotherapy Side Effects Immediate Delayed within days Within weeks Late Immediate Side Effects Allergic reactions: Infusion-related Rituximab Anaphylactic Burning sensation or pain at the site of infusion Irritant Vesicant Urine discoloration Doxorubicin Red Mitoxantrone Blue Immediate Side Effects Acute emesis (Nausea/Vomiting): Within few min – Hrs Peaks after 5-6 hrs Resolves within first 24 hrs Related to: Age Gender Place History of alcoholism (reduce it) History of motion sickness Chemo drugs Anti-emetic used Within days Delayed-onset emesis: > 24 hrs after chemo – 7 days Related to types of chemo drugs (Platinum, Cytoxan, Doxo) Fatigue Myelosuppression: During the nadir of chemo Mucositis Neuropenic fever +/- infection Diarrhea or Constipation Reduced appetite Metallic taste Within weeks Hair loss (Alopecia) Taxanes, Cisplatin, Doxo Peripheral neuropathy Pacltaxel, Oxalipatin, Cisplatin Dry skin or pigmentaion Nail changes Fluid retention Docetaxel Late Side effects Ototoxicity Cisplatin Memory difficulties (chemo brain) Sexual dysfunction Amenorrhea Sterility MDS, leukemia Alkyl agent (2-5yrs), cytoxan (MDS 8-10 yrs) Topoiso ll inhibitor: usually M4, M5ALL (1-2 yrs) 11q23, 21q22, inv 16, t(15:17), t(9:22), t(4:11), t(3:21), t(16:21), t(8:16) Mitoxantrone (2-3 yrs) Cardiotoxicity Anthracyclines Pulmonary fibrosis Bleomycin Delayed A.E. Immediate A.E (days) Delayed A.E. Chemo Starts ? (Wks) Late A.E. Management of a cancer patient who is undergoing chemotherapy What is the patient status? SOAP: Subjective: Fever, pain, S.O.B., cough, bleeding, diarrhea etc … Objective: A/O x 3 V.S.: BP, Pulse, Temp, RR, O2 Dehydration Mucositis Does the pt has a venous catheter Routine full system exam Assessment: Plan: TREATMENT OF SIDE EFFECTS AND COMPLICATIONS OF CANCER THERAPIES What do you need to know? When was the chemotherapy given? Are you dealing with chemo NADIR Any supportive therapy following the chemo was given? List of medication What kind of cancer? What kind of chemotherapy /regimen? EMESIS (Nausea/Vomiting) Causes of N/V in cancer patients Chemo RT Bowel obstruction Brain mets Electrolytes imbalance Hypercalcemia, Hyponatremia, Hyperglycemia Uremia Opiates Gastroparesis (Vincrestine) Psycophysiologic: Anxiety Anticipating N/V CINV • Acute • Onset: minutes-hrs • Resolves: first 24 hrs • Delayed It is easier to prevent N/V than to treat it • Platinum, Cytoxan, Doxo • Onset: >24 hrs • May last for 7 days • Anticipatory • Breakthrough/Refractory Always remember Dyspepsia may mimic nausea Which anti-emetic you should chose for your patient? Anti-emetic regimens should be chosen based on: Chemo drugs and their sequence in the regimen Acute and delayed emesis may overlap Goal of chemo: Palliative vs Adj/curative Patient specific risk factors Smoker Alcoholic: less N/V Gender, Age (more CINV in young female) Hx of N/V or motion sickness Prior experience with anti-emetics Categories of Emetogenic Chemotherapy High emetic risk Moderate emetic risk Low emetic risk Minimal emetic risk *Don’t undertreat *Don’t underestimate 5-HT3 Antagoist Dexa Aprepitant Lorazepam PPI/H2-blocker Dopamine antagonist Management of Delayed Emesis Dopamine antagonists Metoclopramide (Reglan) and Domperidone (Motilium) Sensitize tissues to acetylcholine Stimulate upper GIT motility Facilitate gastric emptying Increase esophageal peristalsis Increase LES pressure Antagonize central and peripheral dopamine receptors Block dopamine receptors in chemoreceptor trigger zone in CNS 2- Haloperidol Anxiolytics/Anti-psychotics Benzodiazepine (Lorazepam) May give the night before and after chemo Phenothiazine: Prochlorperazine (Compazine): Anti-dopaminergic effect Blocking dopamine receptors Blocking vagus nerve in GIT Watch for Dystonic reaction Prochlorperazine Metoclopramide Domperidone Steroids Dexamethasone Improve efficacy of 5-HT3 antagonists With Aloxi for moderate risk: 8 mg d1 enough No need on d 2-3 Do Not use if chemo include steroids e.g. ESHAP Contra-indicated with: IL-2 IFN *Acute emesis: PO/IV Prior to mod-highly emetogenic chemo *Delayed emesis: Days 2-3 Steroids Dexamethasone Always keep in mind its side effects *Hyerglycemia *HTN *Fluid retension *PU *Osteoporosis Serotonin (5-HT3) Antagonists 5-HT3 antagonists (except aloxi/palonosetron) are less effective for delayed emesis A meta-analysis of randomized controlled trials: Adding 5-HT3 antagonist to Dexa did NOT improve antiemetic effect of Dexa for delayed emesis Another study: 5-HT3 antagonists (except Aloxi, not studied) NOT more effective than prochlorperazine for delayed emesis A Canadian meta-analysis: Ondansteron alone did help for delayed emesis Not cost-effective to use 5-HT3 antagonists on d 2-4 Miscellaneous Antipsychotic : Olanzapine (zyprexa) Cannabinol: Dronabinol (marinol) 5-10 mg OR Nabilone 1-2 mg Anti-histamine: Promethazine (phenergan) H2-Blocher or PPI MANAGEMENT OF BREAKTHROUGH (REFRACTORY) EMESIS Breakthrough CINV The most difficult to treat Consider routine (around the clock) rather than PRN Rectal or IV rather than PO Multiple, alternating agents and perhaps routes Do not forget: Hydration Electrolytes Brain mets GI tumors Breakthrough Treatment for CIN/V First Step: Add one agent from a different drug class PRN Antipsychotic : Olanzapine (zyprexa) 2.5-5 mg po bid Caution: elderly, DM Benzodiazepine: Lorazepam 0.5-2 mg Cannabinol: Dronabinol 5-10 mg OR Nabilone 1-2 mg Dopamine antagonists: Metoclopromide , Domperidone, Haloperidol Phenothiazine: Prochlorperazine OR Promethazine Serotonin 5-HT3 antagonists Dexa Breakthrough Treatment for CIN/V Second Step: Continue agent on Schedule Not PRN Agents from different drug class PRN Consider change antiemetics to higher level for next cycle Re-eval, adjust dose and or new drug Anticipatory N/V Negative bad experience with chemo 18-57% of patients N>V Prevention: Optimal anti-emetic with each cycle Acupuncture Alprazolam 0.5-2 mg po tid beginning night before Or Lorazepam 0.5-2 mg po night before and am It is not always medication to do it … It is not always doctors and nurses to do it … It is most of the time the patient to do it … It could be simple and easy …. Non-Medical measures •Eating small frequent meals •Choice of food • Easy on stomach •Eating food at room temperature Dietary consult Behavioral therapy Relaxation/systematic desensitization Hypnosis with guided imagery Music therapy Spiritual Radiation-Induced N/V R.T. - upper abdomin: Pretreatment daily: Granisetron 2 mg qd OR Ondansetron 8 mg bid TBI: +/- Dexa 4 mg qd Pretreatment: Granisetron 2 mg qd OR Ondansetron 8 mg bid-tid +/- Dexa 4 mg qd ChemoRT: CIN/V protocol CANCER-RELATED INFECTIONS PREVENTION TREATMENT PREVENTION 1. Neutropenic precaution 2. Prophylactic antimicrobials 3. G-CSF Neutropenic precaution Hand wash Gloves, Gowns, etc Accessing central venous lines: Written policy Training of medical staff Isolation Prophylactic antimicrobials RISK CATOGERIES Overall infection risk Disease/Therapy Fever/ Neutropenia Antimicrobial prophylaxix Low Standard chemo for solid tumor *Neutropenia < 7 d Low None *Viral if prior HSV Intermediate ASCT Lymphoma MM Purine analog *Neutropenia 7-10 d High *Intermediate if single agent Purine analog *Consider fluoroquinolone (bactrim) *Consider fluconazole during neutropenia, mucositis *Antiviral during neutropenia and at least 30 days after SCT High Allo SCT Acute leukemia Alemtuzumab GVHD on HD steroids *Neutropenia >10 d High *Consider fluoroquinolone (Bactrim) *Anti-fungal: I.D. consult: or consider fluconazole, Ampho-B, Voriconazole, Posaconazole, Micafungin, Itraconazole, *Antiviral during neutropenia and at least 30 days after SCT *Consider PCN and TMP/SMX (GVHD) Fungal prophylaxis Pts with hematologic malignancies and SCT not on antifungal prophylaxis: Severe mucositis is a risk factor for candidemia Consider for all GVHD patients on immunosuppressants Acute leukemia receiving induction or re-induction When selecting drugs: Take into account local susceptibility pattern Remember: Itraconazole, voriconazole, posaconazole are potent inhibitors of cytochrome P450 3A4 isoenzymes than floconazole May decrease clearance of some chemo drugs A lipid formulation is preferred based on less toxicity Anti-viral Prophylaxis For low risk pts: None Prior HSV: during neutropenia Intermediate risk pts: During neutropenia + 30 days after SCT High risk: Acute leukemia: During neutropenia Alemtuzumab: During and minimum 2 m after Alemtuzumab and until CD4 > 200 ASCT: During neutropenia + 30 days after SCT Allo SCT: for the first yr CMV Prevention High risk groups and surveillance period : 1-6 m after SCT GVHD Minimum of 2 m after Alemtuzumzb Surveillance done wkly by PCR or Ag testing Pre-emptive therapy: Ganciclovir, Foscarnet, Valganciclovir (PO) At least 2 wks and until CMV not detected PCP Prophylaxis (Pneumocystis Jirovecii) Recommended Allo SC For 6 m and while on immunosuppressants ALL Throughout anti-leukemic Alemtuzumab For minimum of 2 m after it Considered Fludara, T-cell depleting agents Until CD4 > 200 Prolonged steroids (e.g. Pred > 20mg qd x > 4 wks0 Temodar + RT ASCT For 3-6 m after it PCP Prophylaxis (Pneumocystis Jirovecii) Drugs of choice: TMP/SMX Preferred If allergic or intolerant: Desensitization or Dapsone, aerosolized Pentamidine, Atovaquone G-CSF 10.0 W.B.C. 8.0 6.0 4.0 2.0 Day 0 (Chemo Starts) Day 7 Nadir Day 21 TREATMENT Neutropenic Fever Temp > 38⁰ C Neutropenia ANC < 500 OR Predicted decline to < 500 Look for source of infection: *Catheter sites *Skin *Lungs/Sinus *GIT *GUT Work-up: *CBC with diff *Renal and liver function *UA +/- C/S *C-x-ray *Blood C/S x2 *ABC *Vitals Signs *Venous Access *IVF *O2 *Antibiotics Choice of Initial Antibiotic Should be based on: Infection risk assessment: High risk (inpt, co-morbid, prolonged neutropenia, pneumonia) Low risk (outpt ) Potential VRE and ESBL (Extended Spectrum Beta-Lactamase) MRSA status Local susceptability Organ dysfunction Drug allergy Previous antibiotics Anti-pseudomonous Bactericidal Choice of Initial Empiric Antibiotic IV monotherapy: *Primaxin *Meropenem *Zosyn *Cefepime *Ceftazidime IV combination: *Aminoglycoside + Anti-pseudom *Cipro + Antipseudom Oral for low risk pts *Cipro+ Augmentin or Clinda Vanco, Linezolid, daptomycin , synercid should not be used routinely RESPONDING: •Continue same antibiotic until ANC > 500 and rising •FUO: •DC antibiotic •Documented infection +/bactremia: •Duration of therapy varies *Daily F/U *Eval response in 3-5 d NOT-RESPONDING: •FUO: •Stable: •Cont. same antibiotic •Consider antifungal (high risk pts) •Unstable: •Cover anaerobes, gram neg/positive, Candida •Consider G-CSF •ID consult •Documented infection: •Antibiotic/pathogen susceptibility •Consider G-CSF •Consider Granulocyte transfusion Duration of therapy Bacterial Infection Skin/Soft tissue 7-14 d Simple bacteremia (no tissue site) Gram-negative: 10-14 d Gram-positive: 7-14 d S. aureus: 2 wks after 1st negative blood culture & neg TEE Sinusitis: 10-21 d Bacterial pneumonia: 10-21 d Duration of therapy Fungal & Viral Infection Fungal: Candida: minimum 2 wks after 1st negative blood cultue Mold (e.g. Aspergillus): minimum of 12 wks Bloodstream Yeast: > 2 wks after 1st negative blood cultue Viral: Localized HSV/VZV: 7-10 d (acyclovir, valacyclovir, famciclovir) Influenza: Tamiflu X 10 d and until symptoms resolution ?? Catheter Removal ?? Considered: Recommended: •Septic phlebitis •Tunnel infection •Port pocket infection •Bloodstream infection with: •Candida •S. aureus •P. aeruginosa •Corynbacterium jeikeium •Acinetobacter •Bacillus •Atypical mycobacteria •Yeasts or molds •VRE •Stenotrophomonas maltophilia When to use Vancomycin as initial therapy? Serious infection associated with: Clinically apparent, serious, catheter-related infection Blood culture Gram positive (pending identification/susceptability) Known colonization with PCN/Cephalosporin-resistant pneumococci or MRSA Unstable pt (Hypotensive, septic shock) *DC Soft tissue infection Vanco in 2-3 Pt at risk for Strep viridans bacteremia: days if a resistant Gram Severe mucositis positive not Quinolone or Bactrim prophylaxis identified Recent studies: Vanco unnecessary if beta-lactam agent is used Other agents for resistant Gram-positives *VRE *Vano not an option Linezolid (Zyvox) Quinupristin/Dalfopristin (Synercid) Daptomycin (Cubicin) Outpatient Therapy (Low Risk Neutropenic Fever) Who is a low risk? Fever at home No comorbidities Anticipated short neutropenia (<7d) Good P.S. Creatinine <2 LFTs < 3 X N Assessment: Careful exam Lab: No critical values Criteria for home therapy: Consent for home care 24hr care giver Home phone Access to ER within 1 hr Assess for PO antibiotics: No N/V PO tolerance Not on fluoroquinolone prophylaxi Plan: 2-12 hrs observation Give 1st dose and monitor Discharge planning Pt education Telephone F/U within 1224hrs Outpatient Therapy (Low Risk Neutropenic Fever) Drugs of choice: • Outpt IV longacting antibiotic • PO: Cipro 500mg q8h + Augmentin or Clinda • Daily monitoring at least for the first 3 days • Return to clinic if: • Positive culture • New symptoms/signs • Persistent/recurrent fever • Oral intolerance THANKS