H.1 Hormonal Control
advertisement

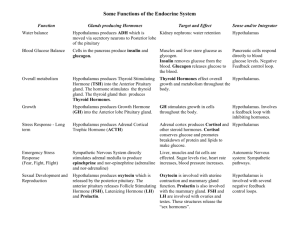
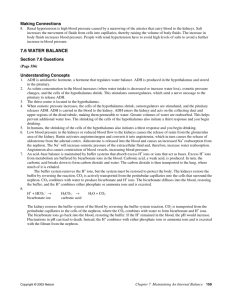
H.1 Hormonal Control IB Assessment Statement • H.1.1 State that hormones are chemical messengers secreted by endocrine glands into the blood and transported to specific target cells. Hormones are Chemical messengers • Produced in endocrine glands • Travel through blood • Affect the target tissues IB Assessment Statement • H.1.2 State that hormones can be steroids, proteins, and tyrosine derivatives with on example of each. Hormone Examples Steroid Hormones Animation Steroid Hormone in action. http://highered.mcgrawhill.com/olcweb/cgi/pluginpop.cgi?it=swf::535::535::/sites/dl/free/00724 37316/120109/bio46.swf::Mechanism%20of%20Steroid%20Hormone%20 Action Peptide Hormone Thyroxine Hormone Animation • http://highered.mcgrawhill.com/olcweb/cgi/pluginpop.cgi?it=swf::535 ::535::/sites/dl/free/0072437316/120109/bio 47.swf::Mechanism%20of%20Thyroxine%20Ac tion IB Assessment Statement • H.1.3 Distinguish between the mode of action of steroid hormones and protein hormones Steroid vs. Peptide Hormones • Steroid hormone: (a) Pass straight through the plasma membrane Directly affect the expression of genes. • Peptide hormone • (b) Attachment to plasma membrane receptor ( Glycoprotein) (c) Receptor-Hormone complex (d) Stimulation of secondary messenger in cytoplasm which alters the action of the cell. IB Assessment Statement • H.1.4 Outline the relationship between the hypothalamus and the pituitary gland Hypothalamus and Pituitary • The diagram shows the posterior division of the forebrain; where the hypothalamus connects the cerebral hemispheres with the middle portion of the brain. • The hypothalamus has many receptors for changes of internal conditions and serves as a link between the nervous system and the endocrine system (pituitary). • Below the hypothalamus is a double lobed structure called the pituitary that produces the endocrine secretions when stimulated by the hypothalamus. Hypothalamus and Pituitary The hypothalamus controls each lobe of the pituitary slightly differently. Control of Anterior Lobe • Hormones are sent from the hypothalamus to the anterior pituitary via a blood vessel called the portal vein. • The hypothalamus acts as the endocrine gland (a) • Hormone travel in blood through the blood vessel (portal vein)(b). • The target tissue is the anterior lobe of the pituitary(c). e.g. LH, TSH and FSH Hypothalamus and Pituitary Control of Posterior Lobe of the pituitary • (d) Neuro-hormones are synthesised in the hypothalamus neuron. They are transported and stored in vesicles in the axon ending located in the posterior pituitary. • (e) Nerve impulses travel down the axon into the posterior pituitary. This causes the release of the vesicles of hormones into the blood stream at the posterior pituitary. e.g. Oxytocin, ADH IB Assessment Statement • H.1.5 Explain the control of ADH secretion by negative feed back • H1.5 ADH and negative feedback control • This is an example of control of the posterior pituitary as outlines in steps (d) and (e) above. • This is an example of the how the hypothalamus and the posterior pituitary integrate to control the release of another hormone. • H1.5 ADH and negative feedback control • The homeostatic regulation of water (osmoregulation) is brought about by the action of the hormone Anti-diuretic hormone. • The hypothalamus is sensitive to changes in plasma concentrations. • Neurosecretory cells in the hypothalamus synthesis ADH and transport this along the axon of their nerves for storage in their synaptic knob endings in the posterior lobe of the hypothalamus. • .. • H1.5 ADH and negative feedback control • Osmoregulatory sensitive cells in the hypothalamus which are sensitive to plasma concentrations stimulate the neurosecretory cells to transmit impulses to their storage regions in the posterior lobe of the hypothalamus. • ADH is secreted and has its target tissue of the Distal Convoluted and Collecting tubules of the kidney. • The ADH causes the opening of the Aquaporin (pores) which increases water reabsorption from kidney filtrate Animation on how the kidney works • http://www.sumanasinc.com/webcontent/ani mations/content/kidney.html • https://www.youtube.com/watch?v=ajgbnOB4jM LE 44-14 Proximal tubule NaCl Nutrients HCO3– K+ H2O H+ NH3 Distal tubule H2O NaCl K+ HCO3– H+ CORTEX Descending limb of loop of Henle Filtrate H2O Salts (NaCl and others) HCO3– H+ Urea Glucose; amino acids Some drugs Thick segment of ascending limb NaCl H2O OUTER MEDULLA NaCl Thin segment of ascending limb Key Collecting duct Urea NaCl Active transport Passive transport INNER MEDULLA H2O The Kidney • The kidneys regulate the amount of water, salts and other substances in the blood. • The kidneys are fist-sized, bean shaped structures that remove nitrogenous wastes (urine) and excess salts from the blood • Because the kidney regulates both salt and water concentration in the blood it is the central organ that controls osmoregulation. The urinary system: The pathway of Urine to the outside the body. • The ureters are tubes that carry urine from the pelvis of the kidneys to the urinary bladder. • The urinary bladder temporarily stores urine until it is released from the body. • The urethra is the tube that carries urine from the urinary bladder to the outside of the body. • The outer end of the urethra is controlled by a circular muscle called a sphincter. • These parts work together and are part of the urinary system. Blood vessels of the mammalian kidney Each kidney is supplied with blood by a renal artery and drained by a renal vein Animation: Nephron Introduction The Kidney The kidney structure Each kidney is composed of three sections: 1. The cortex is where the blood is filtered. 2. The medulla contains the collecting ducts which carry filtrate (filtered substances) to the pelvis. 3. The pelvis is a hollow cavity where urine accumulates and drains into the ureter. The Kidneys Cortex Medulla Renal artery Renal vein Ureter To the bladder Five Steps in the Formation of Urine 1. Ultrafiltration in the renal capsule 2. Selective reabsorption in the proximal convoluted tubules 3. Water conservation in the loop of henle 4. Blood pH and ion concentration regulation in the distal convoluted tubule 5. Water reabsorption in the collecting ducts. Step 1: Ultrafiltration in the renul capsule. • Filtration occurs as blood pressure forces fluid from the blood in the glomerulus into the lumen of Bowman’s capsule • This process is called Ultrafiltration because it is powered by pressure of the blood. • The entire content of the blood is not forced out. • The basement membrane of the of the capsule does not allow blood cells and proteins to enter the filtrate. Step 2 : Selective reabsorption in the proximal convoluted tubules • The convoluted proximal tubules is the longest section of the nephron. • The walls are one cell thick and they are packed with mitochondria. • The cell membrane in contact with the filtrate is packed with microvilli to increase surface area for absorption. Step 2 : Selective reabsorption in the proximal convoluted • The proximal convoluted tubules absorb filtrate through the following mechanisms: – Movement of water via osmosis – Active transport of glucose and amino acids across membranes – Movement of some minerals and ions via a combination of active transport, facilitated diffusion and some gas exchange of ions – Diffusion of urea – Movement of protein via pinocytosis (endocytosis) Step 3 Water conservation in the loop of henle figure 12.23 page 374 • The descending limb is permeable so salt diffuses into the loop of Henle and water diffuses out into the medulla tissue. • At the hairpin zone (base of the loop) water and salt diffuse into the medulla tissue. • In the ascending limb of the loop of Henle, salt diffuses from the permeable loop tubule into the interstitial fluid of the medulla, but water is retained Step 4: Blood pH and ion concentration regulation in the distal convoluted tubule • The distal tubule cells are the same as in the proximal tubule (one cell thick, microvilli and lots of Mitochondria) • The role of the distal tubule cells is to adjust the composition of the blood, in particular pH. • Blood pH is initially buffered by blood proteins, but if it deviates from a pH of 7.4 the concentrations of Hydrogen ion (H+) and hydroxide (OH-) are adjusted • Blood pH does not vary outside the range of pH 7.35 to 7.45, but urine pH ranges from 4.5 to 8.2. Step 5: Water reabsorption in the collecting ducts • The collecting ducts are where the water content is regulated. • When the water content of the blood is low the antidiuretic hormone (ADH) is secreted from the posterior pituitary gland. • When the water is the blood is high, NO ADH is released. . Step 5: Water reabsorption in the collecting ducts. • The permeability of the walls of the collecting ducts are variable. • If ADH is present the walls of the collecting tubules become fully permeable. • This allows water to be withdrawn from the filtrate of the tubule in the medulla. • The water will be taken up and redistributed throughout the body. • ADH is remove from the body by the kidney • When no ADH is present the walls of the collecting duct become less permeable. LE 44-16a Osmoreceptors in hypothalamus Thirst Hypothalamus Drinking reduces blood osmolarity to set point ADH Increased permeability Pituitary gland Distal tubule STIMULUS The release of ADH is triggered when osmoreceptor cells in the hypothalamus detect an increase in the osmolarity of the blood H2O reabsorption helps prevent further osmolarity increase Collecting duct Homeostasis: Blood osmolarity