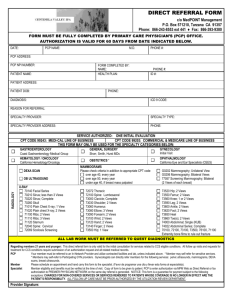
Document
advertisement

Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents Pneumocystis jiroveci Pneumonia Slide Set Prepared by the AETC National Resource Center based on recommendations from the CDC, National Institutes of Health, and HIV Medicine Association/Infectious Diseases Society of America About This Presentation These slides were developed using recommendations published in May 2013. The intended audience is clinicians involved in the care of patients with HIV. Users are cautioned that, owing to the rapidly changing field of HIV care, this information could become out of date quickly. Finally, it is intended that these slides be used as prepared, without changes in either content or attribution. Users are asked to honor this intent. -AETC National Resource Center http://www.aidsetc.org 2 May 2013 www.aidsetc.org Pneumocystis jiroveci Pneumonia: Epidemiology Caused by P jiroveci (formerly P carinii) Ubiquitous in the environment Initial infection usually occurs in early childhood PCP may result from reactivation or new exposure In immunosuppressed patients, possible airborne spread 3 May 2013 www.aidsetc.org PCP: Epidemiology (2) Before widespread use of PCP prophylaxis and effective ART, PCP seen in 70-80% of AIDS patients in the United States In advanced immunosuppression, treated PCP associated with 20-40% mortality Substantial decline in incidence in United States and Western Europe, owing to prophylaxis and ART Most cases occur in patients unaware of their HIV infection, in those who are not in care, and in those with advanced AIDS (CD4 count <100 cells/µL) 4 May 2013 www.aidsetc.org PCP: Epidemiology (3) Risk factors: CD4 count <200 cells/µL Recurrent bacterial pneumonia CD4 percentage <14% Unintentional weight loss Prior PCP High HIV RNA Oral thrush 5 May 2013 www.aidsetc.org PCP: Clinical Manifestations Progressive exertional dyspnea, fever, nonproductive cough, chest discomfort Subacute onset, worsens over days-weeks (fulminant pneumonia is uncommon) Chest exam may be normal, or diffuse dry rales, tachypnea, tachycardia (especially with exertion) Extrapulmonary disease seen rarely; occurs in any organ, associated with aerosolized pentamidine prophylaxis 6 May 2013 www.aidsetc.org PCP: Diagnosis Clinical presentation, blood tests, radiographs suggestive but not diagnostic Organism cannot be cultured Definitive diagnosis should be sought Hypoxemia: characteristic, may be mild or severe (PO2 <70 mmHg or A-a gradient >35 mmHg) LDH >500 mg/dL is common but nonspecific 1,3β-D-glycan may be elevated; uncertain sensitivity and specificity 7 May 2013 www.aidsetc.org PCP: Diagnosis (2) CXR: various presentations May be normal in early disease Typical: diffuse bilateral, symmetrical interstitial infiltrates May see atypical presentations, including nodules, asymmetric disease, blebs, cysts, pneumothorax Cavitation, intrathoracic adenopathy, and pleural effusion are uncommon (unless caused by a second concurrent process) 8 May 2013 www.aidsetc.org PCP: Diagnosis (3) Chest CT, thin-section Patchy ground-glass attenuation May be normal Gallium scan Pulmonary uptake 9 May 2013 www.aidsetc.org PCP: Diagnosis (Imaging) 10 Chest X ray: PCP with bilateral, diffuse granular opacities Chest X ray: PCP with bilateral perihilar opacities, interstitial prominence, hyperlucent cystic lesions Credit: L. Huang, MD; HIV InSite Credit: HIV Web Study, www.hivwebstudy. org, © 2006 University of Washington May 2013 www.aidsetc.org PCP: Diagnosis (Imaging) (2) High-resolution computed tomograph (HRCT) scan of the chest showing PCP. Bilateral patchy areas of ground-glass opacity are suggestive of PCP. Credit: L. Huang, MD; HIV InSite 11 May 2013 www.aidsetc.org PCP: Diagnosis Definitive diagnosis requires demonstrating organism: Induced sputum (sensitivity <50% to >90%) Spontaneously expectorated sputum: low sensitivity Bronchoscopy with bronchoalveolar lavage (sensitivity 90-99%) Transbronchial biopsy (sensitivity 95-100%) Open-lung biopsy (sensitivity 95-100%) PCR: high sensitivity for BAL sample; may not distinguish disease from colonization 12 May 2013 www.aidsetc.org PCP: Diagnosis (Histopathology) Lung biopsy using silver stain to demonstrate P jiroveci organisms in tissue Credit: A. Ammann, MD; UCSF Center for HIV Information Image Library 13 May 2013 www.aidsetc.org PCP: Diagnosis Treatment may be initiated before definitive diagnosis is established Organism persists for days/weeks after start of treatment 14 May 2013 www.aidsetc.org PCP: Preventing Exposure Insufficient data to support isolation as a standard practice, but data suggest highrisk patients may benefit from isolation from persons with known PCP 15 May 2013 www.aidsetc.org PCP: Primary Prophylaxis Initiate: CD4 <200 cells/µL or history of oropharyngeal candidiasis Consider for: CD4% <14% or history of AIDS-defining illness CD4 200-250 cells/µL if Q 3-month CD4 monitoring is not possible Discontinue: On ART with CD4 >200 cells/µL for >3 months Reinitiate: CD4 decreases to <200 cells/µL 16 May 2013 www.aidsetc.org PCP: Primary Prophylaxis (2) Preferred: Trimethoprim-sulfamethoxazole (TMP-SMX) DS 1 tablet PO QD* TMP-SMX SS 1 tablet PO QD For patients who experience non lifethreatening adverse events, consider desensitization or dosage reduction * Effective as toxoplasmosis prophylaxis (for CD4 count <100 cells/µL + positive serology) 17 May 2013 www.aidsetc.org PCP: Primary Prophylaxis (3) Alternative: TMP-SMX DS 1 tablet PO 3 times Q week Dapsone 100 mg PO QD or 50 mg BID Dapsone 50 mg QD + pyrimethamine 50 mg Q week + leucovorin 25 mg Q week* Dapsone 200 mg + pyrimethamine 75 mg + leucovorin 25 mg, all Q week* Aerosolized pentamidine 300 mg Q month via Respirgard II nebulizer (other devices not recommended) Atovaquone 1,500 mg PO QD* * Effective as toxoplasmosis prophylaxis (for CD4 count <100 cells/µL + positive serology) 18 May 2013 www.aidsetc.org PCP: Treatment Duration: 21 days for all treatment regimens Preferred: TMP-SMX is treatment of choice Moderate-severe PCP TMP-SMX: 15-20 mg/kg/day TMP and 75-100 mg/kg/day SMX IV or PO in divided doses Q6-8H Mild-moderate PCP As above, or TMP-SMX DS 2 tablets TID Adjust dosage for renal insufficiency 19 May 2013 www.aidsetc.org PCP: Treatment (2) Alternatives Moderate-severe PCP Pentamidine 4 mg/kg IV QD Recommended for patients who cannot tolerate TMPSMX or experience clinical failure with TMP-SMX; do not combine use Primaquine 30 mg (base) PO QD + clindamycin 600 mg IV Q6H or 900 mg IV Q8H or 300 mg PO Q6H or 450 mg PO Q8H More effective than pentamidine, less toxicity 20 May 2013 www.aidsetc.org PCP: Treatment (3) Alternatives Mild-moderate PCP Dapsone 100 mg PO QD + TMP 15 mg/kg/day PO in divided doses TID Similar efficacy, fewer side effects than TMP-SMX, but more pills Primaquine 30 mg (base) PO QD + clindamycin 300 mg PO Q6H or 450 mg PO Q8H Atovaquone 750 mg PO BID Less effective than TMP-SMX, but fewer side effects 21 May 2013 www.aidsetc.org PCP: Treatment (4) Adjunctive: Corticosteroids For moderate-to-severe disease (room air PO2 <70 mmHg or A-a gradient >35 mmHg) Give as early as possible (within 72 hours) Prednisone 40 mg BID days 1-5, 40 mg QD days 6-10, 20 mg QD days 11-21, or methylprednisolone at 75% of respective prednisone dosage 22 May 2013 www.aidsetc.org PCP: ART Initiation For patients not on ART, start ART within 2 weeks of PCP diagnosis, if possible In one study, lower rates of AIDS progression or death with early ART initiation (no data on patients with respiratory failure requiring intubation) IRIS has been reported; follow for recurrence of symptoms 23 May 2013 www.aidsetc.org PCP: Monitoring and Adverse Events Monitor closely for response to treatment, and for adverse effects of treatment 24 May 2013 www.aidsetc.org PCP: Monitoring and Adverse Events (2) TMP-SMX: rash, Stevens-Johnson syndrome, fever, leukopenia, thrombocytopenia, azotemia, hepatitis, hyperkalemia Atovaquone: headache, nausea, diarrhea, rash, fever, transaminase elevations Dapsone: methemoglobinemia and hemolysis, rash, fever Pentamidine: pancreatitis, hypo- or hyperglycemia, leukopenia, fever, electrolyte abnormalities, cardiac dysrhythmia Primaquine and clindamycin: methemoglobinemia and hemolysis, anemia, rash, fever, diarrhea 25 May 2013 www.aidsetc.org PCP: Treatment Failure Lack of clinical improvement or worsening of respiratory function after at least 4-8 days of treatment If patient not on corticosteroid therapy, early deterioration (day 3-5) may be caused by inflammatory response to lysis of P jiroveci organisms Rule out concomitant infection 26 May 2013 www.aidsetc.org PCP: Treatment Failure (2) Treatment failure resulting from drug toxicities in up to 1/3 of patients Treat adverse reactions or switch regimen Treatment failure caused by lack of drug efficacy in 10% of patients No data to guide treatment decisions For TMP-SMX failure in moderate-to-severe PCP, consider IV pentamidine or primaquine + IV clindamycin For mild disease, may consider atovaquone 27 May 2013 www.aidsetc.org PCP: Preventing Recurrence Secondary prophylaxis (chronic maintenance therapy) for life unless immune reconstitution on ART Preferred: TMP-SMX 1 DS PO QD, or 1 SS PO QD Alternatives: TMP-SMX DS 1 tablet PO 3 times Q week Dapsone 100 mg PO QD or 50 mg BID Dapsone 50 mg QD + pyrimethamine 50 mg Q week + leucovorin 25 mg Q week Dapsone 200 mg + pyrimethamine 75 mg + leucovorin 25 mg, all Q week* Aerosolized pentamidine 300 mg Q month via Respirgard II nebulizer (other devices not recommended) Atovaquone 1,500 mg PO QD Atovaquone 1,500 mg PO QD + pyrimethamine 25 mg QD + leucovorin 10 mg PO QD 28 May 2013 www.aidsetc.org PCP: Preventing Recurrence (2) Discontinue secondary prophylaxis for patients on ART with sustained increase in CD4 count from <200 cells/µL to >200 cells/µL for ≥3 months If PCP occurred at CD4 count >200 cells/µL, prudent to continue prophylaxis for life (regardless of CD4 count) Restart maintenance therapy if CD4 count decreases to <200 cells/µL or if PCP recurs at CD4 count >200 cells/µL 29 May 2013 www.aidsetc.org PCP: Considerations in Pregnancy Diagnosis and indications for treatment: as in nonpregnant women Preferred treatment: TMP-SMX Limited data suggest small increased risk of birth defects after 1st trimester TMP exposure, but pregnant women with PCP should be treated with TMP-SMX Consider increased doses of folic acid (>0.4 mg/day) in 1st trimester: may decrease risk of congenital anomaly but may increase risk of therapeutic failure Pentamidine embryotoxic in animals 30 May 2013 www.aidsetc.org PCP: Considerations in Pregnancy (2) Dapsone: risk of mild maternal hemolysis with long-term therapy; risk of hemolytic anemia in fetuses with G6PD deficiency Pentamidine embryotoxic in animals Primaquine: not generally used in pregnancy, risk of hemolysis; risk of hemolytic anemia in fetuses with G6PD deficiency Clindamycin, atovaquone: appear safe in pregnancy 31 May 2013 www.aidsetc.org PCP: Considerations in Pregnancy (3) Corticosteroid indications as in nonpregnant women; monitor for hyperglycemia Increased risk of preterm labor and delivery; monitor if pneumonia occurs after 20 weeks of gestation Prophylaxis as in nonpregnant adults Consider aerosolized pentamidine or atovaquone during 1st trimester, if risk of teratogenicity caused by systemic agents is a concern 32 May 2013 www.aidsetc.org Websites to Access the Guidelines http://www.aidsetc.org http://aidsinfo.nih.gov 33 May 2013 www.aidsetc.org About This Slide Set This presentation was prepared by Susa Coffey, MD, for the AETC National Resource Center in May 2013 See the AETC NRC website for the most current version of this presentation: http://www.aidsetc.org 34 May 2013 www.aidsetc.org