Conception and Contraception
advertisement

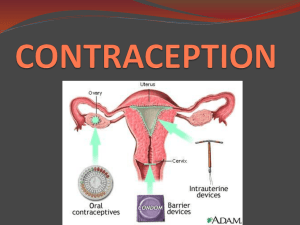
Methods of Birth Control Conception and Contraception Conception refers to the fertilization of an ovum by a sperm. It must involve: A viable egg A viable sperm Access to the egg by the sperm Contraception refers to methods of preventing conception. 2 methods of effectiveness include: Perfect failure rate: risk of pregnancy during the first year of use if the method is used w/o error Typical failure rate: risk of pregnancy during the first year of use w/ normal number of errors Reversible Methods of Birth Control Intrauterine Devices (IUDs) Hormonal methods Barrier methods Fertility awareness and abstinence Intrauterine Devices (IUDs) Copper T IUD—An IUD is a small device that is shaped in the form of a “T.” Your doctor places it inside the uterus to prevent pregnancy. It can stay in your uterus for up to 10 years. This IUD is more than 99% effective at preventing pregnancy. Hormonal Methods Hormonal methods introduce synthetic hormones into the women’s system that prevent ovulation, thicken cervical mucus or prevent a fertilized egg from implanting. Oral contraceptives combine synthetic estrogen and progesterone to prevent release of an ova from the ovary, preventing pregnancy. Progestin-only pills contain small doses of progesterone and are used when suffer from sideeffects related to estrogen or are nursing a baby – slightly less effective than combination pills. Hormonal methods Oral contraceptives—Also called “the pill,” it contains the hormones estrogen and progestin. It is prescribed by a doctor. A pill is taken at the same time each day. If you are older than 35 years and smoke, have a history of blood clots or breast cancer, your doctor may advise you not to take the pill. The pill is 92–99% effective at preventing pregnancy. Early Warning Signs of Medical Complications for Pill Users Figure 7.6 Hormonal methods Patch—This skin patch is worn on the lower abdomen, buttocks, or upper body (but not on the breasts). This method is prescribed by a doctor. It releases hormones progestin and estrogen into the bloodstream. You put on a new patch once a week for three weeks. During the fourth week, you do not wear a patch, so you can have a menstrual period. The patch is 92–99% effective at preventing pregnancy, but it appears to be less effective in women who weigh more than 198 pounds. Hormonal methods Hormonal vaginal contraceptive ring— The NuvaRing releases the hormones progestin and estrogen. You place the ring inside your vagina. You wear the ring for three weeks, take it out for the week you have your period, and then put in a new ring. It is 92–99% effective at preventing pregnancy. Hormonal methods Injection or "shot"— Women get shots of the hormone progestin in the buttocks or arm every three months from their doctor. It is 97–99% effective at preventing pregnancy. Hormonal methods Implant—The implant is a single, thin rod that is inserted under the skin of a women’s upper arm. The rod contains a progestin that is released into the body over 3 years. It is 99 percent effective at preventing pregnancy. Hormonal methods Emergency contraception—Emergency contraception is NOT a regular method of birth control. Emergency contraception can be used after no birth control was used during sex, or if the birth control method failed, such as if a condom broke. One type of emergency contraception requires you to take two doses of hormonal pills 12 hours apart or take both pills at one time. (This is now over the counter for those who are 18 years old and older. You have to take the pills starting within three days (72 hours) after having unprotected sex. They are sometimes referred to as “morning after” pills, even though they can be used up to three days later. The pills are at least 75% effective at preventing pregnancy. Plan B is available over-the-counter for women aged 18 years and older. Plan B is available by prescription for women aged 17 years and younger. (Plan B is the brand name of one product approved by the Food and Drug Administration for use as emergency contraception.) • • • • • Barrier methods: use of a physical or chemical block to prevent the egg and sperm from joining Male condom – latex sheath designed to fit over erect penis catching ejaculate. Foams, suppositories, jellies and creams contain chemical spermicides which kill sperms & some STIs Female condom is soft loose fitting polyurethane sheath that covers the external genitalia. Diaphragm w/ spermicide provides chemical and physical barrier to sperm Cervical cap – small latex cap that fits snugly over the cervix to keep sperm out of uterus Barrier Methods Male condom—Worn by the man, a male condom keeps sperm from getting into a woman’s body. Latex condoms, the most common type, help prevent pregnancy and HIV and other STDs as do the newer synthetic condoms. “Natural” or “lambskin” condoms also help prevent pregnancy, but may not provide protection against STDs, including HIV. Male condoms are 85–98% effective at preventing pregnancy. Condoms can only be used once, and are most effective when used consistently and correctly. You can buy condoms, KY jelly, or water-based lubricants at a drug store. Do not use oil-based lubricants such as massage oils, baby oil, lotions, or petroleum jelly with latex condoms. They will weaken the condom, causing it to tear or break. Barrier methods Male Condoms A male condom is a thin sheath made of latex or other materials Latex condoms protect against pregnancy & STDs Male Condoms 1700 1800 1993 Male Condoms Available in various shapes, colours, flavours, textures and sizes Latex and polyurethane condoms also provide limited protection against HPV that can cause genital warts HSV that can cause genital herpes Hepatitis-B virus Male Condoms How do they work? The man puts the condom on his erect penis The condom holds the semen After sex, the man carefully takes off the condom so that it does not leak. Each condom can be used only once. Male Condoms Male condom instructions Leave about one-half inch of empty space at the tip After intercourse, hold onto the condom at the base of the penis as you withdraw from the vagina Lubricating the condom – contraceptive cream or jelly For latex condom, do not use oil-based lubricants (such as petroleum jelly or vegetable oils) tear Male Condoms Benefits No medical side-effects inexpensive, easily accessed Protecting against STDs ( Latex ) Condoms can help men maintain an erection for a longer period Lower risk for cervical dysplasia and cancer Condoms also prevent sperm allergy which some women suffer Male Condoms Can interrupt sexual activity Some individuals argue that condoms reduce sensitivity and pleasure during intercourse May sometimes tear or leak Can cause an allergic reaction Female Condom Worn by the woman, the female condom helps keeps sperm from getting into her body. It is packaged with a lubricant and is available at drug stores. It can be inserted up to eight hours before sexual intercourse. Female condoms are 79–95% effective at preventing pregnancy when used consistently and correctly, and may also help prevent STDs. Has two flexible rings The inner ring at the closed end of the condom eases insertion into the vagina, covering the cervix and holding the condom in place The outer ring , The larger, open ring stays outside the vagina, covering part of the perineum and labia during intercourse. Spermicides These products work by killing sperm and come in several forms—foam, gel, cream, film, suppository, or tablet. They are placed in the vagina no more than one hour before intercourse. You leave them in place at least six to eight hours after intercourse. You can use a spermicide in addition to a male condom, diaphragm, or cervical cap. Spermicides alone are about 71–82% effective at preventing pregnancy. They can be purchased in drug stores. barrier method Spermicides Spermicides are chemical compounds act to inactivate sperms in the vagina before it can move into the upper genital tract Spermicides , CHEMICAL NATURE TWO BASIC COMPONENTS : 1-ACTIVE SPERMICIDAL AGENTS : Surface acting (surfactants) Nonoxynol-9 Octoxynol-9 Menfegol Recently with antiviral activity : CHLORHEXIDINE,CHOLIC ACID & GRAMICIDINE. 2- THE BASE ( CARRIER ) AGENT foams, jellies, creams, foaming tablets, melting suppositories ,aerosols soluble films or vaginal suppositories. Spermicides How do I use spermicides? *Every time of sexual intercourse. *Insert the recommended dose deep into vagina to cover the cervix well just before sexual intercourse *Insert tablets or suppositories or films 10 minutes ( 5-30 min) before sexual intercourse Spermicides *Use a second dose of spermicides If more than one hour passes before you have sexual intercourse *An additional application of the spermicides is needed for each additional act of intercourse *Douching should not be allowed for at least 6 hours after intercourse Spermicides Characteristics of spermicides? Does not require a prescription May be discontinued at any time Safe May cause irritation in the vagina or on the penis Can cause an allergic reaction May interrupt sexual activity Not recommended for preventing STIs Diaphragm or cervical cap Each of these barrier methods are placed inside the vagina to cover the cervix to block sperm. The diaphragm is shaped like a shallow cup. The cervical cap is a thimbleshaped cup. Before sexual intercourse, you insert them with spermicide to block or kill sperm. The diaphragm is 84–94% effective at preventing pregnancy. Visit your doctor for a proper fitting because diaphragms and cervical caps come in different sizes. The Diaphragm TYPES Coil Spring Arching Spring Flat Spring barrier methods Cervical Cap A cervical cap is a soft, deep rubber cup (like a thimble) with a firm, round rim that fits snugly over the cervix. Cervical Cap Different sizes With Spermicide TYPES Fertility awareness and abstinence Continuous abstinence—This method means not having vaginal intercourse at any time. It is the only 100% effective way to prevent pregnancy. Natural family planning or fertility awareness— Understanding your monthly fertility pattern can help you plan to get pregnant or avoid getting pregnant. Your fertility pattern is the number of days in the month when you are fertile (able to get pregnant), days when you are infertile, and days when fertility is unlikely, but possible. If you have a regular menstrual cycle, you have about nine or more fertile days each month. If you do not want to get pregnant, you do not have sex on the days you are fertile, or you use a form of birth control on those days. These methods are 75–99% effective at preventing pregnancy. Withdrawal Withdrawal is a method in which the man takes his penis out of the woman's vagina just before he ejaculates Permanent Methods of Birth Control These methods are meant for people who want a permanent method of birth control. In other words, they never want to have a child, or they do not want more children. The methods listed here are more than 99% effective at preventing pregnancy. Female Sterilization—Tubal ligation or “tying tubes.”— A woman can have her fallopian tubes tied (or closed) so that sperm and eggs cannot meet for fertilization. The procedure can be done in a hospital or in an outpatient surgical center. You can go home the same day of the surgery and resume your normal activities within a few days. This method is effective immediately. Transcervical Sterilization— A thin tube is used to thread a tiny device into each fallopian tube. It irritates the fallopian tubes and causes scar tissue to grow and permanently plug the tubes. It can take about three months for the scar tissue to grow, so use another form of birth control during this time. Return to your doctor for a test to see if scar tissue has fully blocked your fallopian tubes. Male Sterilization–Vasectomy—This operation is done to keep a man’s sperm from going to his penis, so his ejaculate never has any sperm in it that can fertilize an egg. This operation is simpler than tying a woman’s tubes. The procedure is done at an outpatient surgical center. The man can go home the same day. Recovery time is less than one week. After the operation, a man visits his doctor for tests to count his sperm and to make sure the sperm count has dropped to zero; this takes about 12 weeks. Another form of birth control should be used until the man’s sperm count has dropped to zero. Surgical Methods Sterilization Female Tubal ligation is a method where surgery ties or cuts and cauterizes the uterine tubes. This blocks the sperm’s access to released eggs. Hysterectomy is the surgical removal of the uterus. It’s usually done only when there is disease or damage to the uterus. Male Vasectomy is a procedure where both ductus deferens are surgically cut and tied shut. Sterilization Figure 7.7