PowerPoint with caring device - Scotland's Health on the Web
advertisement

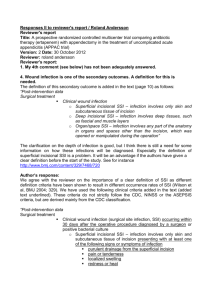
Scottish Surveillance of Healthcare Associated Infection Programme SURGICAL SITE INFECTION SURVEILLANCE Training to ensure valid and reliable surveillance data Why are we here? • National SSI surveillance in Scotland – Establishing the impact of HAI in Scotland – HDL (2001) 57 • All acute Divisions must do surveillance of 2 surgical procedures, 1 of which should be orthopaedic HDL (2006)38 • Hip arthroplasty surveillance mandatory from Jan 2007 if procedure performed within hospital • Readmission surveillance must be undertaken for this category until day 30 post op • Caesarean section surveillance mandatory from Jan 2007 • PDS must be undertaken to day 30 post all for all c section procedures Surveillance is: • Policing! • A survey – Research – Audit HPS’s Role Scottish Surveillance of Healthcare Associated Infection Programme • To co-ordinate, facilitate and support the implementation of SSI surveillance • To prepare Protocols • To prepare data collection tools • To support on-going data management and ensure quality data • To collate and report the national data set Today’s climate and demands! • Public awareness! • Quality is at the heart of everyone’s agenda – Clinical Governance – Clinical Standards – Accountability Reviews – Performance Assessment Framework HAI - Extent of the problem • 100, 000 patients affected per year • 5000 deaths per year The Cost of HAI AIM Scottish Surveillance of Healthcare Associated Infection Programme • To promote accurate completion of surgical site infection surveillance forms Learning Objectives Scottish Surveillance of Healthcare Associated Infection Programme • To recognise the benefits of surveillance in relation to surgical site infection (SSI) • To describe the background to SSI surveillance • To discuss the importance of data definitions • To evaluate the variety of processes that can be utilised to carry out SSI surveillance Introduction to Surveillance • Surveillance is the ongoing systematic collection, analysis, and interpretation of health data essential to the planning, implementation, and evaluation of public health practice, closely integrated with the timely dissemination of these data to those who need to know. The final link of the surveillance chain is the application of these data to prevention and control. (Centers for Disease Control and Prevention 1988) Introduction to Surveillance • The objectives of healthcare associated infection (HAI) surveillance are to: – Monitor the incidence of HAI, including SSI – Provide early warning and investigation of problems and subsequent planning and intervention to control – Monitor trends, including the detection of outbreaks – Examine and share the impact of interventions – Gain information on the quality of care – Prioritise the allocation of resources Introduction to Surveillance • Surveillance is a multidisciplinary activity and local ownership is crucial • National surveillance should be a byproduct of local surveillance • Local feedback is essential HAI Proportion of all HAI (%) Proportion of extra bed days(%) Proportion of extra cost (%) Proportion preventable? (%) UTI 45 11 13 38 SSI 29 57 42 35 Pneumonia 19 24 39 Sur 27; Med13 Bloodstream 2 4 3 35 Other 6 4 3 N/A Source: Haley 1995 and 1985 HAI SWI Cost (£pp) 3246 •in-patient only Source: Plowman et al. Socio-Economic Burden of HAI Nat Burden*(£M) 62.37 Background to SSI surveillance – What is the problem? • Specific operation categories known to have • Surveillance can result in a reduced infection rates but is unacceptably high infection unlikely to be the only factor: rates – ICTs • Many factors have been – Commitment of all staff recognised that influence – Education on risk the occurrence of SSI factors/evidence based – Pre operative practice – Intra operative – Adequate staffing, resources, equipment – Post operative – Is there a Hawthorne effect? Background to SSI Surveillance • SSI is therefore important as it continues to be a key complication of surgery, with high human and financial costs • The potential to improve infection rates through surveillance has been proven • A number of other programmes are already in place: – NNIS – SSISS – PAN CELTIC – Local projects • In Scotland: SSHAIP Scottish SSI Surveillance Programme – the way forward…… • SSI Surveillance Protocol and Resource Pack • HAI Surveillance newsletter to share good practice • Communications and visits with all divisions • Updates to National Steering Group • Training for those involved………… Operation Categories for SSI Surveillance • Orthopaedic: hip replacement, knee replacement, operations for fractured neck of femur • Cardiac: CABG, other cardiac surgery • General: breast, major vascular • Obs/Gyn: abdo hysterectomy, c.section • Cranial Surgery PATIENT PATHWAYS FOR SSI SURVEILLANCE TO POST OP DAY 30 Admission Death Operation Post Operative In-patient Discharge Transfer Death Re-operation In-patient to day 30 Post Discharge Surveillance Re-admission PDS to day 30 In-patient end of Surveillance End of Surveillance Decide on operation categories for surveillance Ensure key personnel are prepared and all systems are in place to commence the surveillance Pilot and launch the programme Identify multidisciplinary personnel to be involved in the local surveillance team Hold training sessions for key personnel to include SSI definitions and data management* Hold surveillance team meetings to discuss logistics of the programme. Discuss forms, definitions, dataset, start date etc.* Produce local guidance and make forms, posters and flowcharts available in key areas *The SSHAIP team at HPS should be involved at these stages Project officer administrates the surveillance All forms are uniquely identified and originate in theatre Surgeon completes questions in theatre Anaesthetist completes questions in theatre Theatre nurses complete questions on the form Form is transferred to ward with patient Ward nurses complete questions IC Dept provides local feedback Project officer manages the data and transfers this to HPS ICN contacted when SSI present and completes questions Ward clerk returns forms to the project officer (Infection Control department) when the patient is discharged Pre Pre admit admit nurse nurse places stored places stored forms forms supplied by supplied bycocoordinator (ICSN ordinator (ICSN checks checks on on aa weekly weekly basis) basis) in in all all patient patient notes notes and and completes completes demographics demographics Ward Ward staff staff complete complete relevant details relevant details on on the form during inthe form during inpatient patient stay, stay, prompted prompted by by integrated integrated care care pathway pathway Surgical Surgical site site inspection carried inspection carried out out ifif infection infection suspected suspected NB NB Forms Forms are are pulled pulled from from store store ifif patient patient re re presents presents in in hospital hospital with with surgical site infection surgical site infection following following discharge discharge Form Form goes goes with with patient patient notes notes to to ward area ward area Ward Ward clerkess clerkess completes completes follow followup up date on form on date on form on patient patient discharge discharge and and sends sends for for ms ms to to arthoplasty arthoplastynurse nurse practitioner practitioner (ANS) (ANS) Data Data sent sent to to ICSN ICSN and quality checks, and quality checks, including including denominators, denominators, performed performed before before feedback feedback given given to to MDT monthly MDT monthly The The form form goes goes with the patient with the patient notes notes into into theatre theatre All All operative operative details details completed completed by anaesthetist, by anaesthetist, and and surgeon surgeon or or theatre theatre nurse nurse where where relevant relevant Forms Forms stored stored by by ANS and ANS and completed completed as as necessary necessaryat at follow up review follow up review Forms Forms sent sent to to Audit Dept for Audit Dept for scanning scanning and and collation collation Daily visits to all surgical wards to carry out wound checks Wounds are checked before discharge from hospital Data are graphed and fed back to the surgeons, nurses and infection control team on a monthly basis Wound surveillance nurse administrates the project Wound surveillance nurse identifies patients from theatre lists Operative details…completed by wound surveillance nurse on the ward post op Demographic details…completed by wound surveillance nurse on the ward pre-op Patients have a 24 hour answer service telephone number to call with wound problems. Primary care staff also liaise with wound surveillance nurse Data are managed and collated by the wound surveillance nurse Patients with identified wound problems are seen at wound surveillance clinics, or at home by the wound surveillance nurse for wound review Patients are seen at wound surveillance clinics, or at home by the wound surveillance nurse at day 30 post-op for wound review Data collection completed at site Data are sent to the local surveillance coordinator Data are quality checked and anonymised (Patient identifying details removed) Data are sent to local nominated data transfer coordinator (if required) Forms sent to HPS by post Data scanned at HPS and database with reporting facilities fedback to hospital within 3 months Electronic data transfer to HPS* Collated for national reporting of SSI surveillance National Report Results fed back to hospitals Pan Celtic Collaboration IPSE Essential Elements of a Successful HAI surveillance system • Defining what outcomes to measure • Ensuring everyone involved is aware of the outcomes • Reliably collecting the data in a standardised/defined manner • Analysing data for comparison • Using the data locally in a timely manner to improve quality of care Gaynes & Solomon. J Quality Improvement 1996;22:457- In Summary • Recognise the benefits of and the background to conducting SSI Surveillance • Understand and apply to your setting the various processes that can be utilised to conduct SSI Surveillance AIM Scottish Surveillance of Healthcare Associated Infection Programme • To promote accurate completion of surgical site infection surveillance forms Learning outcomes Scottish Surveillance of Healthcare Associated Infection Programme • To define the categories that are included in diagnosing SSIs • To describe and discuss the appearance of surgical sites, to include the aforementioned categories • To explain the surveillance form completion process Definitions of SSI Superficial SSI (Incisional) • A superficial SSI must meet the following criterion: 1. Infection occurs within 30 days after the operative procedure 2. And involves only skin and subcutaneous tissue of the incision 3. And patient has at least one of the following: • Purulent discharge from the superficial incision • Organisms isolated from an aseptically obtained culture of fluid or tissue from the superficial incision • At least one of the following signs or symptoms of infection: pain or tenderness, localised swelling, redness, or heat and superficial incision is deliberately opened by surgeon unless incision is culture negative • Diagnosis of superficial incisional SSI by surgeon or trained healthcare worker* (* Trained healthcare worker is defined as a qualified doctor or nurse who has been trained in the national definitions of SSIs.) Definitions of SSI Superficial SSI (Incisional) • The following are not reported as superficial incisional SSI: – Stitch abscess (minimal inflammation and discharge confined to the points of suture penetration) – Infected burn wound e.g. diathermy – Incisional SSI that extends into the fascial and muscle layers (deep incisional SSI) Definitions of SSI Deep SSI (Incisional) • A deep incisional SSI must meet the following criterion: 1. Infection occurs within 30 days after the operative procedure if no implant is left in place or within one year if implant is in place and the infection appears to be related to the operative procedure 2. And involves deep soft tissues (e.g. fascial and muscle layers) of the incision Definitions of SSI Deep SSI (Incisional) 3. And patient has at least one of the following: • Purulent discharge from the deep incision but not from the organ/space component of a surgical site • A deep incision spontaneously dehisces or is deliberately opened by a surgeon when the patient has at least one of the following signs or symptoms: fever (>38oC) or localised pain or tenderness, unless incision is culture negative • An abscess or other evidence of infection involving the deep incision is found on direct examination, during re-operation, or by histopathological or radiological examination • Diagnosis of a deep incisional SSI by surgeon or trained healthcare worker Definitions of SSI Organ/Space SSI • An organ/space SSI involves any part of the body, excluding the skin incision, fascia, or muscle layers that is opened or manipulated during the operative procedure. Specific sites are assigned to organ/space SSI to further identify the location of the infection. An example is an appendicectomy with subsequent diaphragmatic abscess, which would be reported as an organ/ space SSI at the intra-abdominal specific site. Definitions of SSI Organ/Space SSI • An organ/space SSI must meet the following criterion: 1. Infection occurs within 30 days after the operative procedure if no implant is left in place or within one year if implant is in place and the infection appears to be related to the operative procedure 2. And infection involves any part of the body, excluding the skin incision, fascia, or muscle layers that is opened or manipulated during the operative procedure Definitions of SSI Organ/Space SSI 3. And at least one of the following: • Purulent discharge from a drain that is placed through a stab wound into the organ/space • Organisms isolated from an aseptically obtained culture of fluid or tissue in the organ/space • An abscess or other evidence of infection involving the organ/space that is found on direct examination, during re operation, or be histopathological or radiological examination • Diagnosis of an organ/space SSI by surgeon or trained healthcare worker Organ/Space SSI • Vascular: – Arterial or venous • Breast: – Breast abscess – Mastitis • Orthopaedic: – Joint or bursa – Osteomylitis • Abdominal Hysterectomy: – Intraabdominal – Endometritis – Vaginal Cuff – Ovaries, uterus, pelvic cavity • C. Section: – Endometritis – Ovaries, uterus, pelvic cavity Criteria Used to Determine SSI – Surveillance Form (generic) • Purulent drainage • Organisms isolated from an aseptically obtained culture of fluid or tissue • Abscess/other evidence found on direct examination, during a re-operation or radiology/histopathology • Incision spontaneously dehisces • Incision is deliberately opened by surgeon • Fever (temperature 38 degrees or more) • Localised pain or tenderness • Localised swelling • Redness • Heat • Diagnosis by surgeon or trained healthcare worker Extra criteria for organ/ space infection • Vascular: – Organisms not isolated from blood/ blood culture not done • Abdominal Hysterectomy/ • Orthopaedic: C.Section: – Limitation of motion – Nausea – Evidence of effusion – Dysuria – Organisms and WBC seen on gram stain – Vomiting of joint fluid – Organisms seen – Positive antigen test on blood, urine or on gram stain joint fluid – Cellular profile and chemistries of joint fluid compatible with infection NB: No extra criteria for breast Various extra criteria for cardiac/ CABG (See SSI protocol) Other definitions of wound infections • • • • • • • • Cellulitis Delayed healing Discolouration Friable granulation tissue, which bleeds easily Pocketing at the base of the wound Bridging within the wound Odour 105 colony forming units per gram of tissue Surgical site microbiology • Common organisms found to cause SSIs: – Staphylococcus aureus – Coagulase-negative staphylococci – Gram negative bacilli – Anaerobes – group B streptococci • These can be endogenous flora • Exogenous flora are also common and avoidable • Surgical site culturing – Why are you sampling? – When are you sampling? – What are you sampling? – How are you sampling? – Labelling and lab form completion – Interpreting results from the lab Risk Index for SSI Surveillance • SSI rates, by surgical procedure/category, which will be stratified by risk index. • The NNIS risk index will be used for this. • This index scores each procedure according to the presence or absence of three risk factors at the time of surgery and scores range from 0 (none of the factors present) to 3 (all of the factors present). The risk factors are: – ASA score>=3 – Wound classified as contaminated or dirty – Duration of operation Background to SSI Surveillance – Wound Classes • Surgical wounds can be classified according to the likelihood and degree of wound contamination at the time of operation. • The wound classification used for this surveillance is based on that developed be the National Research Council in the USA. Wound Classes • Clean • Clean contaminated • Contaminated • Dirty or infected Wound Classes • A minimum wound class is only indicative and may vary according to certain pre operative and intra operative events. • The final classification of wound contamination must be confirmed in consultation with the surgeon, or by checking the patient’s records. Wound Classes • Clean wounds: An uninfected operative wound in which no inflammation is encountered and the respiratory, alimentary, genital or uninfected urinary tracts are not entered. In addition clean wounds are primarily closed and if necessary drained with closed drainage. Operative incisional wounds that follow non-penetrating (blunt) trauma should be included in this category if they meet the criteria. Wound Classes • Clean contaminated wounds: Operative wounds in which the respiratory, alimentary, genital or urinary tracts are entered under controlled conditions and without unusual contamination. Specifically, operations involving the biliary tract, appendix, vagina and oropharynx are included in this category, provided no evidence of infection or major break in sterile technique is encountered. Wound Classes • Contaminated wounds: Open, fresh, accidental wounds. In addition, operations with major breaks in sterile technique (e.g. open cardiac massage) or gross spillage from the gastrointestinal tract and incisions in which acute, non-purulent inflammation is encountered are included in this category. Wound Classes • Dirty or infected wounds: Old traumatic wounds with retained devitalised tissue and those that involve existing clinical infection or perforated viscera. This definition suggests that the organisms causing postoperative infection were present in the field before the operation. ASA Classification • 1. Normal healthy patient • 2. Patient with mild systemic disease • 3. Patient with severe systemic disease that is not incapacitating • 4. Patient with an incapacitating systemic disease that is a constant threat to life • 5. Moribund patient who is not expected to survive for 24 hours with or without operation In Summary • What am I looking for? – Has an SSI occurred, are there defined signs and symptoms of infection? – The onset date (signs and symptoms of infection present should be completed on the form when first noticed) • Complete the form – With pre, peri and post operative details (see form completion instructions) Form completion – general points X • Place a cross in the appropriate box • Use a dark pen or biro • Correct errors by completely filling the box where the incorrect response is • Write clearly within the boxes when completing free text and do not write on the line of the boxes 2 • An empty box does not imply anything! Form completion – general points • DO NOT: – Use light pens – Use a tick – Leave gaps – Staple or tape through/over the four black cornerstone boxes – Write or draw on the black unique identifier box in the bottom corner of the forms – Photocopy forms (you may for your own use however HPS require all originals) Form completion – general points • Complete the form: – – – – – On discharge On death On transfer On re-operation (at the same surgical site) At day 30 (if patient is still an in-patient or PDS in being carried out) • Even if there is an implant complete the form at this time. • In some instances forms will continue to be completed during the post discharge surveillance period. Procedures should be in place locally for managing this. • Remember to ensure that the box for ‘no infection present’ is completed when surveillance ends. Conclusion • Standardised methodologies for SSI surveillance are essential to allow valid, reliable and comparable data. This includes the use of a common set of understood definitions. • The local multi-disciplinary team play an essential role in the success of SSI surveillance. • SSI rates are key quality indicators for surgery In Summary…. • Understanding the definitions of SSIs and their clinical appearances are essential • Accurate completion of surveillance forms is key • Visit our updated SSHAIP Website: www.show.scot.nhs.uk/scieh/ - select HAI& Infection Control.