"SSI Prevention: Preparing for the future by going back to the basics"
advertisement

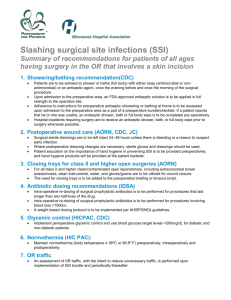
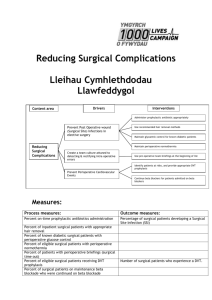
Presented by: Kathleen Kohut, RN, MS, CIC, CNOR System Director of Infection Prevention Cone Health, Greensboro, NC 3M AMN Healthcare The Compass Group BE Smith Consulting Johns Hopkins Hospital NCH Healthcare System APIC 1. 2. 3. 4. 5. Discuss the five basics of SSI prevention Describe the use of glycemic control, nasal decolonization, and normothermia initiatives for the reduction of SSIs. Name the 2 most common mechanisms for wound contamination Name 3 SCIP Measures Discuss two opportunities for practice improvement Current National SSI Initiatives include: The Joint Commission National Patient Safety Goal NPSG.07.05.01 included in 2009 CMS Public reporting requirements for SSIs 2012 - Colon Resections and Abd Hysterectomies ▪ Nationally 1. Antibiotic Prophylaxis ( Inf- 1,2,3) Drug, Timing, Dosing, Discontinuation 2. 3. 4. 5. Hair Removal (Inf- 6) Glycemic Control (Inf – 4) Foley Catheter removal POD1 or POD2 (Inf- 9) “Normothermia” (Inf 10) Expanded in June 2011 All surgical patients http://www.jointcommission.org/specifications_manual_for_national_hospital_in patient_quality_measures.aspx http://www.jointcommission.org/assets/1/6/Surgical%20Care%20Improvement% 20Project.pdf SSI is an unfortunate possibility (it says so right on the consent form) Challenge-change the culture of tolerance to one of intolerance to SSI The Business Case- maximization of OR volume to increase revenue Challenge- improve efficiencies without compromising infection prevention Tradition Challenge- re-examine practices from a fresh perspective to find new opportunities Lack of research Challenge- conduct research and publish to create a solid body of evidence Five Focus Areas: 1. 2. 3. 4. 5. Patient Preparation Aseptic Technique ABX Prophylaxis Hair Removal Skin Antisepsis Losing weight, quitting smoking Glucose Management Nasal Decolonization Normothermia – pre-warming The stress response induced by surgical procedures increases blood glucose levels Non-diabetics may also experience hyperglycemia during this critical perioperative period CDC(2011). http://www.cdc.gov/diabetes/pubs/factsheet11.htm; accessed on May 10, 2013. >25 million Americans diagnosed with diabetes > 7 million are undiagnosed 79 million considered pre-diabetic 30-35% of cardiac patients are diabetics http://www.cdc.gov/diabetes/pubs/factsheet11.htm SCIP INF 4: Cardiac surgery patients with controlled 6 a.m. postoperative serum glucose. All Patients should be managed with a target of <200 The first 24 hours is critical The OR cannot be a black hole Between 25-30% of all patients are colonized at any given time and another 60% carry it intermittently. Carriers are at higher risk S. aureus causes 25-35% of all HAIs 20% of all surgical pts acquire some type of HAI during their postoperative course Perl, TM, et al. Intranasal Mupirocin to Prevent Postoperative Staphylococcus Aureus Infections. N Engl J Med 2002; 346(24): 1871-7. 85% of S. aureus infections were endogenous in SSI study populations Van Rijen, et al. Intranasal Mupirocin for reduction of S. aureus in surgical patients with nasal carriage. J Anti Chemotherapy 2008; 61:254-261. MRSA SSI rates decreased from .23% to .09% (5,094 pts) with MRSA eradication program Pofahl, WE, et al. Active Surveillance Screening of MRSA and Eradication of the Carrier State Decreases SurgicalSite Infections Caused by MRSA. J Am Coll Surg 2009;208:981-988. SCIP Measure Inf-10 Includes all SCIP surgical patients (June 2011) ▪ Total Knee, Hip, Vascular, Cardiac, ABD Hyst, Colon Resect Requires one temperature > 96.8º F(36º C) 30 min. before or 15 min after anesthesia end time. Start with pre-warming Principles were developed to reduce the risk of wound contamination. Risk of SSI = Dose of Bacterial Contamination X Virulence Resistance of Host (patient) Berry & Kohn’s, Operating Room Technique, 11th ed., p. 254 Exogenous sources 1. Cleanliness of environment, lack of proper airflow, shedding by the Surgical Team Endogenous sources 2. Patient’s own skin/hair Infection at a remote site People = Shedding 4000-10,000 particles per minute (Berry & Kohn’s, Operating Room Technique, 11th ed., p. 252) Carried by wind currents to the sterile field which results in wound contamination. 1. 2. 3. 4. 5. 6. Patient Surgical Team Ancillary Personnel Sales Reps Students Passersby Requires the control of the amount of traffic and the traffic patterns themselves Essential personnel only One foot (min) perimeter around sterile field Sterile fields should be a destination, not a thoroughfare Limit students and observers ▪ The right of the student to learn vs. the right of the patient to receive safe patient care Utilize alternative methods of communication Sherertz, et al. “Cloud” HCWs. Emerging Infect Dis. 2001;7(2): 241-44. Edmiston, et al. Airborne Particulates in the OR Environment. AORN 1999; 69(6): 1169-1183. People + Wind + (-) Aseptic Technique > ABX + Skin Prep = Wound Contamination = SSI Patient Opportunities Pre-op showering program -At least 2 showers with CHG Hat and clean gown/linen for patient transport Hair removal only when necessary Clippers, not in the OR Association of periOperative Registered Nurses (AORN). Recommended Practices for Perioperative Patient Skin Antisepsis. Perioperative Standards and Recommended Practices 2013 ed., pp75-89. Chlebicki MP, et al. Preoperative chlorhexidine shower or bath for prevention of surgical site infection: A meta-analysis. Am J Infect Control 2013;41:167-73. Newsmanager.commpartners.com/shea/issues/2013-04-02/1.html. Accessed 4/3/13. Surgical Team Hand Hygiene Nocardia farcinica (Wenger, et al. J Infect Dis. Nov 1998) Proper aseptic technique Properly worn hats, masks, clean OR scrubs, jackets, minimal jewelry (AORN scrub attire) If it takes 17 years to adopt new technology, our time is up! Dineen, P, Drusin, L. Epidemics of Postoperative Wound Infections Associated with Hair Carriers. Lancet 1973; (Nov) 1157-59. Institute of Medicine (IOM). (2001). Crossing the quality chasm. Crossing the quality chasm: A newhealth system for the 21st century. Washington: National Academy Press. THE JACKSON LABORATORY BIOTECHNOLOGY COMPANY COSTCO Room Requirements • Ventilation System ▪ (min 15- recommended- 20-25/hr, 3 fresh) ▪ Positive pressure • Temperature (68-73° F) • Humidity (20-60%) Room Cleaning • Between cases • Terminal cleaning • Types of construction materials • Clutter AORN, Recommended Practices for Perioperative Nursing: Patient & Worker Safety. (2011 ed., p 219-221) SCIP Measures - INF 1,2,3 and NPSG.07.05.01 (#7) Goal >95% ▪ Challenge the organization to 100% Proper dosage for obese population (BMI>30) (Surg 1989;106:750) Redosing q 3 hours (Ann Surg 2009; 250:10) • RCA or Med Error if missed Bratzler, DW, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health-Syst. Pharm. 2013;70:195-283. 1. SCIP measure (Inf-10) 2. NPSG.07.05.01 (#8) Goal Minimize as much as possible Clippers only 3. Not addressed: Location of hair removal The attributes of an appropriate surgical skin antiseptic require: The ability to significantly reduce microorganisms (2 log-dry sites, 3 log-wet sites) Provide broad spectrum activity Be fast acting Have a persistent effect All products with FDA approval meet this criteria Association of periOperative Registered Nurses (AORN). Recommended Practices for Perioperative Patient Skin Antisepsis. Perioperative Standards and Recommended Practices 2013 ed., pp75-89. 1. Procedure (location and type of incision site) May challenge the prep area with the presence of blood, saline, friction from retractors, etc. 2. Patient Safety Consider not using alcohol based preps for head and neck surgeries due to the highest risk of fire. CDC SSI guideline states to “use an appropriate antiseptic” SHEA Compendium - “Optimal preparation and disinfection of the operative site” AORN compares products but does not provide specific product recommendations NQF 2011 recommendation: “use solutions that contain isopropyl alcohol as skin antiseptic preparation until other alternatives have been proven as safe and effective, and allow appropriate drying time per product guidelines.” National Quality Forum: http://www.qualityforum.org/News_And_Resources/Press_Releases/2011/NQF_Maintains_Endor sement_of_Safe_Practice_to_Prevent_Surgical_Site_Infection.aspx Limited research is available that compares commonly used skin antiseptic agents with SSI outcomes The majority of the literature compares microbial counts Much more work must be done to create a body of evidence to guide practice Saltzman, MD, et al. Efficacy of Surgical Preparation Solutions in Shoulder Surgery. J Bone Joint Surg AM 2009;91:1949053 Microbial culture study of 150 patients comparing 3 methods (Iodophor Scrub/Paint vs. ChloraPrep® vs. Duraprep™) Swenson, et al. Preoperative skin preparation on postoperative wound infection: a prospective study of three skin preparation protocols. Infect Control Hosp Epidemiol 2009; 30:964-971 ▪ SSI Outcome study of 3209 pts comparing 3 methods (Iodophor Scrub/ETOH/Paint vs. ChloraPrep® vs. DuraPrep™ Darouiche, RO, et al. Chlorhexidine-Alcohol versus Povidone-Iodine for Surgical-Site Antisepsis. N Engl J Med 2010; 362(1):18-26. Microbial culture study of 849 patients comparing 2 methods (Iodophor Scrub/Paint vs. Chlorhexidine-alcohol) Savage, JW et al. Efficacy of Surgical Preparation Solutions in Lumbar Spine Surgery. J Bone Joint Surg Am. 2012;94:490-4 Efficacy study comparing ChloraPrep® to DuraPrep™ preop, post prep, and post-op Mechanism of actions: Denatures (kills) proteins Bactericidal Fungicidal Virucidal Does not kill spores Has no persistent effect Association of periOperative Registered Nurses (AORN). Recommended Practices for Perioperative Patient Skin Antisepsis. Perioperative Standards and Recommended Practices 2013 ed., pp75-89. Follow manufacturer’s directions Read the labels! Utilize proper aseptic technique during application & gloves to contain shedding Create relationships between IP, OR, SPD, Pre-op, Surgeons (and their offices): Learn how they do their work Learn how you can help each other Choose process measures together Its about partnering not policing Provide process data on an ongoing basis Maintains focus ▪ IUS rates ▪ Compliance with surgical attire Review outcome data regularly SSI Rates SSIs are preventable and there is much work to be done The tools for success include SCIP measures, NPSG.07.05.01, process and outcome data and the operating room basics to: 1. Educate 2. Measure 3. Communicate