Review of Frozen Section Results and correlation with microbiology
advertisement
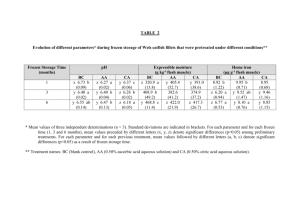
Review of Frozen Section Results and correlation with microbiology for revision joint replacement surgery Dr R Hadden BSc MBBS SpR Histopathology Derriford Hosptial Revision Surgery • Currently Frozen Section is considered by Orthopaedic surgeons as a vital tool in assessment of periprosthetic joint infections. • Main Indications – aseptic or septic loosening • Intraoperative decision on type of procedure – One stage – Two stage Problems • No agreed Gold Standard single test for diagnosing periprosthetic joint infections (PJI). • International Consensus Meeting on PJI. PJI Is Present When One of the Major Criteria Exists or Three Out of Five Minor Criteria Exist Major Criteria Two positive periprosthetic cultures with phenotypically identical organisms, OR A sinus communicating with the joint, OR 1) Elevated serum C-reactive protein (CRP) AND erythrocyte sedimentation rate (ESR) Minor Criteria 2) Elevated synovial fluid white blood cell (WBC) count OR ++change on leukocyte esterase test strip 3) Elevated synovial fluid polymorphonuclear neutrophil percentage (PMN%) 4) Positive histological analysis of periprosthetic tissue 5) A single positive culture Criterion Acute PJI (< 90 days) Chronic PJI (> 90 days) Erythrocyte Sedimentation Rate (mm/hr) Not helpful. No threshold was determined 30 C-Reactive Protein (mg/L) 100 10 Synovia White Blood Cell Count (cells/μl) 10,000 3,000 Synovial Polymorphonuclear (%) 90 80 Leukocyte Esterase + Or ++ + Or ++ Histological Analysis of Tissue > 5 neutrophils per high power field in 5 high power fields (× 400) Same as acute Local guidelines • No universally agreed gold standard (even within local team) • Based on the number of polymorphs per high powered field in at least five separate fields – <5 - indicates no active infection and one stage advised – 5-10 - possible infection, surgeon preference along with clinical picture to dictate surgical management – >10 - indicative of active infection, requiring two stage surgical management Recent Series Of 15 Patients • If “clear operative field” and <20neuts/hpf – an infection free outcome is possible after single stage re-implantation • If “poor surgical field appearances”, associated with >20neuts/hpf. 2 stage procedure done. • Confirms our anecdotal evidence that positive frozen sections are macroscopically abnormal (colour/texture/odour). Conflicting evidence • Cut off 10 or 20 neuts/hpf? • Do surgeons actually comply with local guidelines? Results • Reports on 50 sequential samples were reviewed • The microbiology results were reviewed • Correlation between the two was assessed Frozen results • 8 positive (>10 neuts/hpf) • 36 Negative • 6 Equivocal (5-9 neuts/hpf) Positive FS • Of the 8 positive Frozen sections: – All confirmed on paraffin – 4 grew organisms • 1 on initial culture • 3 on “enrichment” Negative FS • 34/36 confirmed on paraffin • 2/36 cases 0 neuts on frozen, “small numbers” on later paraffin sections – Likely negative • 24/36 grew organisms – 1 on culture – 23 on enrichment culture Equivocal / Borderline • 6 cases 5-9 neuts/hpf – 4 with growth on enrichment culture – 2 with no growth – All had no growth on initial culture Results Negative frozen section Equivocal frozen section Positive frozen section Single stage operation 110 4 Two stage operation 28 5 2 Other 0 0 1 0 Summary • Negative result: 25% go on to have 2-stage procedure! • Equivocal result: 50/50 split – presumably based on clinical/other test results • Positive result: Good compliance (n) Results Negative frozen section Equivocal frozen section Positive frozen section Negative Cultures 101 4 1 Positive Cultures 36 5 2 Results Negative frozen section Equivocal frozen section Positive frozen section Required Revision 17 2 0 No Further Revision 121 7 2 • 12% with negative FS required revision • 22% with equivocal FS required revision • 0% with positive FS required revision Discussion • Why do surgeons ignore negative result in 25% of cases? What is the point of FS in these cases? • In equivocal FS cases, what determines the procedural outcome? Does FS really make a difference? • 2011-2012 approximate costs of £15,000. Histology concerns: • Anecdotally, positive FS correlates with macro findings. – In the Korean series, high numbers of neuts correlated with macroscopic impression. • The 0-5, 5-10, 10+ criteria are arbitrary and based only on one study. • Recent criteria use histology (not necessarily FS histology!) as only a minor criteria for PJI. Microbiology concerns: • Correlation with microbiology results is difficult. – Confounding factors (pre/intraop abx). – Most growth is on “enrichment culture”, we do not know the significance of these results. Learning points / Questions • Negative predictive value is published as the most important factor in intraoperative testing • Why did many –ve FSs have +ve micro? ?sampling or FS poor sensitivity • 25% of negative frozen sections still had a 2-stage procedure • Is there another test or clinical parameter that “trumps” frozen section? • Targeted or limited use should be advised (JK agrees this – reaudit needed to confirm)