Physician_Documentation_Tips_03_09
advertisement

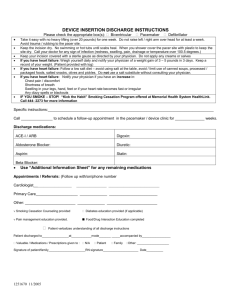
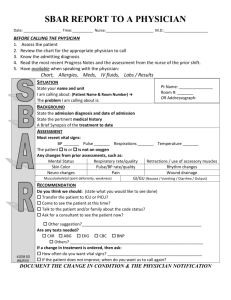
Physician Documentation Tips Lisa Bazemore, MBA, MS, CCC-SLP Documentation – Who needs it? Documentation • Why is documentation so important to medical necessity? This is a time of “defensive documentation” • Just like universal precautions – assume any and all charts will be audited. A reviewer of your medical record will only see the ink and paper you send. In some cases they are incentivised to deny your claims! Documentation • What is your perception of these statements from actual medical records? The patient has no previous history of suicides. The patient refused autopsy. Discharge status: alive but without my permission. She stated that she had been constipated most of her life until 1989 when she got a divorce. Rectal examination revealed a normal-size thyroid. On the second day the knee was better, and on the third day it had completely disappeared. The patient has been depressed since she began seeing me in 1993. Healthy appearing decrepit 69 year old male, mentally alert but forgetful. Documentation • When auditors review our charts, all they see is what we have documented. They don’t know the patient and don’t know our protocols for patient care. Physician Documentation Physician Documentation • Purpose: Establish medical necessity Clearly state why the patient needed to occupy an inpatient rehabilitation bed Indicate why the patient requires an intense level of rehabilitation services List problems and services that are needed Define why patient could not have their needs met in a skilled nursing facility AND Document information required to ensure continuity of high quality care Physician Documentation • Physician By-In for Medical Necessity Recognize most physicians do not think in terms of medical necessity documentation • “It is not that we don’t think about med necessity or med necessity documentation, it is just hard for us to realize what it is that someone expects to see to think that a patient needed a treatment (IRF). This is a new concept to us. We were not taught this in our training. And, it is so obvious to us that they need to be in IRF, we think it is obvious in the chart why they needed to be in IRF.” Physicians should be partnered with for the good of the patient and facility so that they: • Understand the importance of medical necessity and medical necessity documentation in rehab • Can identify how medical necessity can be assimilated into their current documentation style Physician Documentation • What’s so special about Physical Medicine and Rehabilitation? Combining into one Plan of Care • Medical treatments • Therapy treatments Three levels of documentation quality • Basic: Some documentation of therapy status and goals in the same document as medical status • Advanced: Documentation about therapy treatment status, plan and goals in the same document as the medical treatment plan • Exemplary: Links medical and therapy issues so it is clear how the two are interrelated Physician Documentation • What’s so special about Physician documentation? Auditors report if the proof of medical necessity can be easily identified in the H&P and discharge summary they spend less time reviewing the rest of the chart. Physician Documentation – H&P • Admission History & Physical Format Patient Name/History #; Room # Date of Admission: History of Present Illness: • Medical History (please include onset date, chief complaint and functional implications) Allergies: Medications: (Comment about medication reconciliation: home meds, MAR and discharge summary meds with discrepancies) Past Medical History: Social History: (home meds, assistance available) Family History: (do not use non-contributory) ROS: (end with “all other ROS negative except as noted above”) Physical Exam: Physician Documentation – H&P • Admission History and Physical Format (continued) Assessment/ Plan: • Impairment (Reason for admission) • Etiologic diagnosis (Pathophysiologic reason for reason for admission) • Medical Necessity – “The etiologic diagnosis and comorbidities listed below require the 24 hour availability and frequent intervention of a physician with specialized training in rehabilitation.” List of cormorbidities & interventions. Physician Documentation-H&P • Admission History and Physical Format (continued) • Rehab Necessity (Medical Impact on Function) – Treatment plan: Include nursing (“24 hr. rehab RN for bowel program, therapy carryover, pt edu., skin, . . .”) Include therapy (“Intensive therapy for 3 hours/day 5 days/week. Interventions: PT to address . . . OT to address . . . , etc” OR “Refer to complete admission orders for interventions”) Include weekly team conferences to coordinate plan of care. Physician Documentation – H&P • Admission History and Physical Format (continued) This care could not be provided in a lower level of care because . . . . Rehabilitation Goals: Functional Prognosis: Estimated LOS: Planned Discharge Disposition: Physician Documentation – H&P • Assessment / Problem List Provides details of conditions that require care: • Medical conditions that require daily physician oversight • Functional deficits that require intensive, coordinated therapy • Complexity of conditions that require nursing assessment and carry over 24 hours a day Physician Documentation – H&P • We gather codes from physician documentation, so we need to be able to identify: • Actively treated conditions • Newly recognized conditions • Resolving/resolved conditions Physician Documentation – H&P • Assessment / Problem List should include: Rehabilitation diagnosis (primary functional limitation, primary impairment and cause) Complications and coexisting conditions Symptoms that will require treatment Chronic medical conditions Potential conditions that require preventive measures, restrictions and/or precautions Functional deficits to be treated by the program Physician Documentation – H&P • What is the plan?: The preliminary plan supports medical necessity by describing the “treatment for the condition” Indicates the decision to admit the patient Provides evidence of the complexity of the interdisciplinary program Lists the interventions to be provided by each team member Implies the skill level required to provide such services Physician Documentation – H&P • The plan supports medical necessity by exhibiting: Multidisciplinary treatment Individualized care. • It supports the problem list by including: Medical conditions that require daily physician oversight Functional deficits that require intensive, coordinated therapy Complexity of conditions that require nursing assessment and carry over 24 hours a day Physician Documentation – H&P • Things to avoid in the assessment and plan: Do not use the same statement for all patients admitted Less is not more Writing efficiently can help control length Limiting the list to medical conditions only Forgetting to document what nursing will do Forgetting to document what therapy will do Comments like: • “Medically stable” • “No medical issues” • “I don’t know why this guy is here” • “Uneventful course” Physician Documentation – H&P • What’s on your list of things to avoid? • What is your favorite canned statement? Physician Documentation – H&P • Evaluating medical necessity content in Physician History and Physicals: This evaluation system is a rough tool to help identify where to focus education efforts. • Recall, three levels of medical necessity content: Basic: Some documentation of therapy status in the same document as medical status, orders therapies Advanced: Documentation about therapy treatment status, goals and plan in the same document as the medical treatment plan Exemplary: Links medical and therapy issues so it is clear how the two are interrelated. Physician Documentation – H&P • Basic: Some documentation of therapy status in the same document as medical status, orders therapies Example: • H&P – lists medical problem list and includes functional status • Comorbidities: Hypertension Uncontrolled Diabetes Metastatic colorectal carcinoma Dependence with mobility and self care skills • Will initiate physical and occupational therapies, rehabilitative nursing, medical case management and physician oversight due to the medical problems noted above Physician Documentation – H&P • Advanced: Documentation about therapy treatment status, goals and plan in the same document as the medical treatment plan Example: • H&P – lists therapy goals and interventions as well as medical goals and interventions • We will initiate comprehensive rehabilitation program with physical therapy, occupational therapy, recreational therapy, 24 hour rehabilitation nursing and physicians. She will benefit from this comprehensive rehabilitation program to address ADLs and mobility status post surgery as she is currently requiring moderate assistance for ADLS and mobility • Hypertension – will monitor and adjust dosing of Norvasc and hydrochlorothiazide due to recent uncontrolled pressures • Postop anemia. Hemoglobin has been stable at 9, will continue to monitor and consider adding iron supplementation if this continues to be an issue. Will hold off for now as patient has constipation and iron can be constipating • Rehabilitation therapies. Goals to manage pain, increase ambulation and ADLs to goal of independent level and to work on range of motion with CPM machine. Assess for equipment needs and home safety Physician Documentation – H&P • Exemplary: Links medical and therapy issues so it is clear how the two are interrelated. Example • H&P – lists how medical impairments will impact therapy progress • A 72-year old female, previously modified independent, following cerebellar infarct – decreased balance, coordination, unable to return to prior level of function. Needs inpatient rehab, physical/occupational therapies for function as well as decreased cognition, in need of speech therapies. Rehab physician care management for therapy plan of care, management of pain control with non-narcotic use, management of chest pain and monitoring for complications following stroke. Rehab nursing care to work on bowel and bladder training, transfers, education. • Physical therapy to work towards improvement of bed mobility, transfer training, balance/coordination with gait to a modified independent level • Rehab nursing to support therapy goals, return to modified independent with bowel/bladder, educate on prevention of stroke • Occupational therapy . . . • Speech therapy . . . Physician Documentation – Progress Notes • Proving medical necessity during the stay: Close medical supervision means patient requires medical care daily Evidenced through physician visits and progress notes • Do each of these visits demonstrate active intervention by the physicians on the medical and rehabilitation needs of the patient? • Are there changes in orders for the rehabilitation intervention? Physician Documentation – Progress Note • The Daily Progress Note: SUBJECTIVE: OBJECTIVE: Vitals: BP , T , P , R , Pulse ox LUNGS: clear to auscultation bilaterally __, rhonchi __, rales __, wheezes __, crackles __ CV: regular rate and rhythm __ murmurs __, rubs __, gallops __ Abd: soft __, non-tender __, normal active bowel sounds __, obese __ Ext: cyanosis __, clubbing __, edema __, calf tenderness __ (Right __ Left __) Neuro: Labs: PLAN: 1. 2. 3. 4. 5. Justification for continued stay Medical issues being followed closely Issues that 24 hours rehabilitation nursing is following Rehab progress since last note – Continue current care and rehab or adjustment to POC - Physician Documentation – Progress Note • Saying it: Document Document Document Document consulting progress with rehabilitation programs changes in plan of care barriers to attaining goals collaborative efforts of team and other physicians Physician Documentation – Progress Note • Remember to include: Medication changes – document why changed Lab results – document decisions made based on lab results Ordering additional tests/labs – document reason why ordered, discuss risks, advantages, hasten rehab participation and discharge Document interaction with other professionals Document patient’s functional gains as discussed with patient Physician Documentation – Progress Note • Evaluating progress of medical necessity in Physician Progress Notes: • Basic: Some documentation of therapy status in the same document as medical status, orders therapies Example • Progress note – Some documentation about therapy such as functional status or missed therapy time. • Patient reports he is ambulating with the assist of only one therapist and a rolling walker. Yesterday he required the assistance of two therapists • Missed 1 hour of therapy due to nausea and vomiting yesterday Physician Documentation – Progress Note • Advanced: Documentation about therapy treatment status, goals and plan in the same document as the medical treatment plan Example Progress Note – Documentation about changes to the treatment plan due to barriers or progress Therapy progress is delayed due to new onset cognitive issues, I will order a speech therapy consult Pain is limiting progress in all disciplines so we will increase the patient’s pain medications to include . . . Missed 1 hour of therapy due to nausea and vomiting, will add Phenergan PRN for reoccurrence Physician Documentation – Progress Note • Exemplary: Links medical and therapy issues so it is clear how the two are interrelated Example Progress Note – medical comorbidities impact on therapy is considered Hypertension remains uncontrolled despite adjustment in Norvasc. This has resulted in fatigue and discomfort that have caused the patient progress slowly with PT and OT. Will consult cardiology to assist with control of hypertension and remove this barrier to intensive therapy participation. Missed 1 hour of therapy due to nausea and vomiting per PT, will add Phenergan PRN for reoccurrence and monitor participation in intensive rehab via conversations with therapy. Physician Documentation – Discharge Summary • Components of the Discharge Summary: Medical Issues that required an acute level of care: Patient is a 63 year old male with a history of… While on the unit we managed these complicated issues… Brief History of Rehab Stay: Functional Independent Measures Scores (in Functional Independence Measure language) Ambulation - The patient was () on admission with gait at () feet with/without assistive device. The patient was () at discharge with gait at () feet with/without assistive device. Admission Eating Grooming Bathing UE Dressing LE Dressing Toileting Discharge Physician Documentation – Discharge Summary Discharge Diagnosis: Discharge Co-morbidities: Discharge Follow-up: Discharge Diet: regular __, ADA __, AHA __, low salt __ Discharge Condition: stable __, fair __, guarded __ DISCHARGE MEDICATIONS: DISCHARGE LABS: DISCHARGE RADIOLOGY REPORTS: PLAN: 1. Discharge medications written 2. Discharge follow-up with 3. Discharge therapy with outpatient/home health care/no therapy needed Physician Documentation – Discharge Summary • Evaluating progress of medical necessity in Physician Discharge Summaries: • Basic: Some documentation of therapy status in the same document as medical status, orders therapies • Example • Discharge Summary – lists therapy status admit to discharge • Patient was minimal assistance for grooming, upper body dressing, toilet transfers, toileting and ambulation for 50 feet with a rolling walker at admission. Also required moderate assist for bed to wheelchair transfers and bathing. • At discharge the patient was modified independent for all functional independence measure items. • Medically the patient was admitted with uncontrolled hypertension and severe anemia which were treated during her stay with two adjustments to her Norvasc dose and 2 units of PRBC respectively. At the time of discharge both are controlled and will be followed by her primary care physician upon discharge. Follow up with PCP in 1 week. Physician Documentation – Discharge Summary • Advanced: Documentation about therapy treatment status, goals and plan in the same document as the medical treatment plan Example Discharge Summary – Lists therapy status at admission, interventions and goal achievement as well as medical status, intervention and outcome At admission the patient was moderate assistance for essentially all ADLs and was not able to ambulate. Physical and Occupational therapy intervened with gait and mobility training with the outcome of the patient progressing to meet the goal of modified independent with use of a rolling walker to ambulate at discharge. Medically the patient was admitted with intractable pain, sepsis and acute vs. chronic atrial fibrillation which was treated with consultation to internal medicine, IV antibiotics, frequent monitoring by rehab nursing and myself. He developed dehydration and an electrolyte hypokalemia during this admission which was treated with IV fluids and potassium supplementation with good results. At discharge the dehydration and hypokalemia have resolved. The a-fib is considered chronic and will be followed by his cardiologist. The infection is being treated with p.o. antibiotics and will be followed by internal medicine at discharge. Pain is ongoing – patient to continue Percocet and follow up with me in 1 week. Physician Documentation – Discharge Summary • Exemplary: Links medical and therapy issues so it is clear how the two are interrelated Example • Discharge Summary – Medical and therapy progress are described together • Course of Inpatient Rehabilitation: At admission the patient presented with hemiparesis, hypertension, and renal insufficiency all which contributed to her being dependent for all ADLs and mobility. Additionally she had a dysphagia with resultant aspiration pneumonia. • Hemiparesis: was a major focus of physical and occupational therapy. She was identified as dependent at admission for all ADLs and mobility. Through application of skilled therapy and rehabilitation nursing interventions the patient progressed to moderate assistance and her son and husband were trained to safely care for her at home. • Hypertension: Blood pressure was high at admission and is thought to be the precipitating factor in her MCA infarct stroke. It remained high at admission and was treated with close monitoring and adjustments to her dose of Lopressor. The hypertension and medication adjustments induced fatigue which resulted in her missing some scheduled therapy. Once her dose was stabilized hypertension was no longer a barrier to her participation in intensive therapy. • Renal insufficiency: . . • Pneumonia: . . . Questions? Lbazemore@erehabdata.com (202) 588-1766