Quality in The Clinical Microbiology Laboratory
advertisement

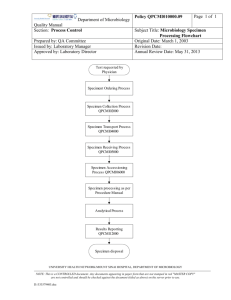
Antimicrobial disk susceptibility testing Quality in The Clinical Microbiology Laboratory Dr.S.Hekmat Reference Health Laboratory Total laboratory Quality Program quality management(QM) Continuous quality Improvement (CQI) or Performance improvement (PI) Quality Control (QC) Quality Assurance (QA) Test Cycle Preanalytical (sampling , labelling , transport , storage , specimen clinical information ↓ Analytical ( macroscopic evaluation , microscopy , culture , identification , interpretation , antibiogram , .. ) ↓ Post analytical ( Final report to physician ) Quality management ( QM ) QM is : A process of looking of what is done How it is done Identifying opportunities for improvement Making the appropriate changes Assessing the impact QC and QA are integral and essential components of QM . CQI and PI CQI and PI went a step further by seeking to improve patients care by placing the emphasis on not making mistake on first place; CQI and PI advocate continuous training to guard against having to correct deficiencies QUALITY ASSURANCE PROGRAMME QA • A quality assurance (QA) programme is concerned with sampling, specifications and testing as well as with organization, documentation and release procedures that ensure that the necessary and relevant steps have been taken to ensure satisfactory quality. • The bacteriology and immunology laboratory is responsible for providing accurate and relevant information that is of use for clinical diagnosis of a patient or in support of a public health activity. The accuracy and clinical value of the laboratory analysis of the clinical specimen and microbial isolates are dependent upon a QA programme that • assesses the quality of the specimen, • documents the validity of the test method, • monitors the performance of test procedures, reagents, media, instruments and personnel, • and reviews test results for errors and clinical relevance An effective QA programme is dependent on a continuous process of assessment and improvement. It has two broad components: • Quality assurance = Internal quality control + External quality assessment Continue…. QA is the sum of activities to ensure that test results are accurate , reproducible and timely However The speed , the cost , and the usefulness or clinical relevance of the test is important. It must be comprehensive , concentrate on the most critical steps , provide continuous monitoring of test procedures , able to detect and correct errors as they occur. Internal quality control • Internal quality control (IQC) is the set of procedures undertaken by the staff of a laboratory for continuously and concurrently assessing laboratory work and the emergent results, to decide whether they are reliable enough to be released. These results may be required for a wide variety of purposes; e.g. support of clinical decision making or epidemiological surveillance or research. Internal quality control procedures have an immediate effect on the laboratory’s activities and should actually control – as opposed to merely examining – the laboratory’s output. Internal Quality Control IQC Practical Realistic Economical QC program The laboratory director is primarily responsible for QC and QA programs. However all laboratory personnel must actively participate in both program Sources of error that effect the reliability and reproducibility Specimens: Sampling , transport,storage, processing Environmental factors: Inadequate space working : ventilation, temperature, excessive noise, unsafe :work conditions,.. Personnel: Education, training , experience, condition of employment Laboratory materials Quality or reagents, stains, chemicals, culture media , , Test method ; some methods are more reliable : Equipments Substandard or poorly maintained instruments Examination and reading :Hurried Reading of results , failure to examine sufficient number of microscopic fields,… Reporting Procedures Begins with proper laboratory operations based on SOPS for: • Collection of specimen Registeration of specimen Processing of specimen. Care of equipment Preparation and storage of culture media , stains , reagents and antisera Antibiotic susceptibility tests Stock cultures Safety precautions Personal hygiene Handling and disposal of infected material Parameter Guidelines Specimen collection and Provide instructions for collection and transport transportation Establish criteria for acceptable specimens Establish rejection criteria for unacceptable specimens Personnel Use sufficient qualified personnel depending upon volume and complexities of work Provide continuous technical education Provide written performance standards Evaluate annually QC records Record all QC results on prescribed forms Report all out-of-control observations to supervisor Note corrective actions on QC form Review QC records monthly Patient reports Report only to authorized personnel Notify test requester of important values immediately Provide normal ranges where appropriate Correct errors in patient’s reports in timely fashion Retain records for at least two years Information should be filled Patient name Hospital or laboratory number Ordering physician Whether the patient receiving antimicrobial therapy Suspect agent or syndrome Written collection instruction Test selection criteria Patients selection criteria Timing of specimen collection (e.g., Before antimicrobial are administration) Optimal specimen collection site Approved specimen collection method Specimen transport medium Continue… Specimen transport time and temperature Specimen holding instructions if it cannot be transported immediately (e.g. hold at 4C for 24 hours) Availability of test (on –site or sent to reference laboratory ) Hours test performed (daily or batch) Turn-around time Result reporting procedures Criteria for unacceptable specimens Unlabeled or mislabeled specimens Use of improper transport medium Excessive transport time Improper temperature during transport or storage Improper collection site for test request Specimen leakage out of transport container Personnel It is laboratory director's responsibility to employ sufficient qualified personnel for the volume and complexity of the work performed. Document competency and training twice a year Continuing education program should be provided All documentation should maintained in personnel file External quality assessment • External quality assessment (EQA), which was earlier known as proficiency testing, refers to a system of objectively assessing the laboratory performance by an outside agency. The assessment is retrospective and periodic in clinical microbiology unlike industrial microbiology such as production of vaccines and immunobiologicals which, as per the laws of the land, require testing by an agency independent of the manufacturer before their release for use. The main objective of external quality assessment is to establish • inter-laboratory comparability. This will influence the reliability of future testing. In contrast, the main objective of internal quality control is to ensure day-to-day consistency. Hence, both internal quality control and external quality assessment are complementary in ensuring the reliability of procedures, their results and finally the quality of the product quality control of equipment Biological safety cabinets Autoclave Oven Incubator Refrigerator Water- bath Microscope Continue.. Maintenance records should be retained in the laboratory for the life of instrument. Specific guidelines regarding periodicity of testing for autoclaves, biological safety cabinets ,centrifuges ,incubators, microscope, refrigerators ,freezers, water bathes , heat blocks and other microbiology laboratory can be found in reference books Culture media Ordering and storage of dehydrated media Order quantities for 6 months or at most 1 year. The overall quantity should be packed in containers that will be used up in 1-2 months. Write date of receipt on each container Store in a dark , cool, well ventilated place When a container is opened , write the date of opening on it Discard all dehydrated media that are either caked or darkened Storage of prepared media• Distilled or demineralized water should be used for • preparation of media Protect against sunlight • Protect against heat. Media containing blood, antibiotics • ,… should be stored in refrigerator The shelf-life of prepared media when stored in cool , • dark place depend on the type of container used. Tybes with cotton – wool plygs 3 weks • Tubes with loose caps 2 weeks • containers with screw – caps 3 months • Petri dishes , sealed in plastic bags 4 weeks • Commercially Prepared Culture Media The NCCLS subcommittee on media quality control collected data over several` years regarding the incidence of QC failure of commonly used microbiology media Based on its finding the subcomm ittee published a list of media that did not require retesting in the user's laboratory if purchased from a manufactures who follow NCCLS guidelines pH testing Prepared media should not be checked routinely. If it is prepared in house from basic ingrediente it should be allowed to cool before the pH tested. Solid media with a surface electrode or after macetration in distilled water. If pH differs 0.2 units from the specification, adjust with acid or alkali or prepare a new batch. Sterility Check A representative sample of each media which blood or their components are added after autoclaving should be test for sterility; 3-5% of any batch is tested. Sterility is routinely checked by incubating the medium for 48 hours at the 35 C temperature . More than 2 colonies per plate if seen , discard the whole batch.. Performance testing When medium dose need to quality controlled because it was prepared “in house (in the laboratory) or because it is complex, several basic rules must be followed : All media must be tested before use Each medium must be tested with organisms expected to give positive reaction as well as with organism expected either not to grow or produce a negative reaction Continue.. Performance tests for different commonly used media are Performed by different microorganisms ( stock culture ) Blood agar Performance test *( hemolysis and growth ): s.Pyogenes s.Pneumoniae Bacitracin disc positive Negative Medium s. pyogenes (zone) E.faecalis blood agar User-Prepared and Noncommercially prepared Media QC forms for user-prepared media should contain: The amount of prepared The source of each ingredient The lot number The preparation date The expiration date (Usually 1 month for agar plate and 6 month for tube media) Sterlization methods: All user prepared colures media also should checked for : Continue. Proper color Depth Smoothness Clarity Hemolysis Excessive bubbles Contamination Stain and Reagents Containers of stains and reagents should be labeled as to contents, concentration ,storage requirements, date prepared (or received) date placed in service ,expiration date, source (commercial manufacture or user prepared) and lot number .All stains and reagents should be stored according manufacture's recommendations and tested with positive and negative controls before use. Antisera The lot number, date received, condition received ,and expiration date must be recorded for all shipments of antisera.In addition ,the antisera should be dated when opened .New lots must be tested concurrently with previous lots, and testing must include positive and negative controls. Use of Stock Cultures To operate a quality control program, stock culture must be maintained by all laboratories .They are available from many sources. Commercial sources Clinical specimens Proficiency testing Reference laboratories Official Culture Collection (ATCC) Preservation Long –term Lyophilization Storage at -70C TSB with 15 % Glycerol CTA for Neisseria and streptococci Cooked-meat medium for anaerobes Short-term TSA slants Store in refrigerator Transfer every 2 weeks. Stock strains for quality control suggusted by CLSI Escherichia coli ATCC 25922 Pseudomonas aeruginosa ATCC 27853 Staphylococcus aureus ATCC 25923 Streptococcus pneumoniae ATCC 49619 Enterococcus faecalis ATCC 29212 Haemophilus influenzae ATCC 49247 Klebsiella Pneumoniae ATCC 70063 Antimicrobial Susceptibility Testing ( AST ) METHODS OF AST Diffusion Kirby – Bauer method Dilution MIC 2) Agar dilution Diffusion & Dilution Test method Eٍٍٍ 1) Broth dilution Reagents for the Disk Diffusion Test 1-Selection of Antimicrobial Disks (source of infection and the isolated pathogen ) 2- Mueller- Hinton Agar medium -prepared from commercially dehydrated powder -4mm depth ( 25-30 ml for plates with100mm diameter ) -Store in 2-8 C within 7days 3-StandardTurbidity )0.5 McFarland ) from isolated colony Mueller Hinton Agar Medium Preparation of Mueller Hinton Agar Moisture PH Effects of Thymidine or Thymine Effects of Variation in Divalent Cations Testing Strains That Fail to Grow Satisfactorily Turbidity Standard 0.5 McFarland standard ( 0.5 ml of 0.048 mol/ml BaCl2 added to 99.5 ml of 0.18 mol/L H2SO4(1% v/v) density in 625 nm = 0.08 - 0.1 Keep in 4-6 ml aliquots in screw cap tubes in dark , room temperature Replace or verify density month 3/14/2016 AST 42 3/14/2016 AST 43 Common sources of error Inhibitory substance thymine and thymidine: Enterococcus faecalis ATCC 29212 or 33186 tested by SXT disc . An inhibition . zone ≥ 20 mm and free of colony. Control zones too small may be due to : Discs with low potency for bad storage or expired discs. Too dense inoculum. Too thick culture media. small zones for tetracyclines and beta- lactams indicate pH is too high. zones for aminoglycosides which are too small indicate pH is too low Salmonella and Shigella Fecal isolates : Ampicilin , a quinolone , SXT Extraintestinal isolates of Salmonella; In addition chloramphenicol and a third generation cephalosporin should be tested and reported. Vibrio cholerae MIC is the best method : Broth or agar dilution method Antibiotic agents : Ampicillin Tetracycline SXT Chloramphenicol Antibiotic susceptibility of Neisseria gonorrhoeae Medium : GC agar Inoculum ; Direct colony suspension Incubation ; 35 C , 5% CO2 , 20-24h Disk diffusion tests with ampicillin , penicillin , rifampin are unreliable for Nisseria meningitidis , MIC is necessary. Positive β - lactamase test predicts resistance to ampicillin , penicillin ,amoxicillin. Gonococci with 10-unit penicillin disk zone ≤ 19 mm are likely to be β - lactamase producing strains. β - lactamase test remains preferable to other susceptibility methods for rapid , accurate penicillin resistance Patient Report The laboratory should established a system for supervisory of all laboratory reports. This review should involve checking the specimens workup to verify that the correct conclusion were drawn and no clerical errors were made in reporting results. Reports should be given only given only authorized by law to receive them. Continue.. Clinician should be notified about ‘’panic values’’ immediately. Panic values are potential-threatening results, for example positive Gram stain for CSF or a positive blood culture. All patients records should be maintained for least 2 years.