Quality Management Staff - Minnesota Department of Health
advertisement

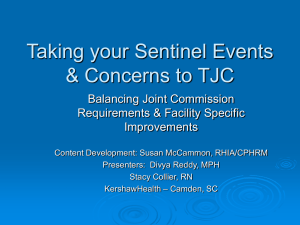
Focused Review of a Sentinel Event Root Cause Analysis Determination the Need for Focused Review • When something goes wrong, the appropriate clinical experts are in consultation – – – – – Administration Physician leadership Nursing leadership Risk Management Quality Management Determination of Need for Focused Review continued • It is determined that the event meets the definition for sentinel events – NQF 27 Adverse Event Criteria – JCAHO Minimum Criteria • The event is a near miss (good catch) – the event has resulted or could have resulted in patient harm • Problems keep repeating NQF Adverse Events • Surgical Events • Product or Device Events • Patient Protection Events • Care Management Events • Environmental Events • Criminal Events JCAHO Minimum Events • Events resulting in an unanticipated death or major permanent loss of function, not related to the natural course of the patient’s illness or underlying condition JCAHO Minimum Events • Event is one of the following (even if the outcome was not death or major permanent loss of function unrelated to the natural course of the patient’s illness or underlying condition) – Suicide of any individual receiving care, treatment or services in a staffed around-the-clock care setting or within 72 hours of discharge – Unanticipated death of a full-term infant – Abduction of any individual receiving care, treatment or services – Discharge of an infant to the wrong family – Rape – Hemolytic transfusion reaction involving administration of blood or blood products having major blood group incompatibilities – Surgery on the wrong individual or wrong body part – Unintended retention of a foreign object in an individual after surgery or other procedure JCAHO Minimum Events • Unanticipated death or major permanent loss of function associated with a health careacquired infection • Severe neonatal hyperbilirubinemia (bilirubin >30 milligrams/deciliter) • Prolonged fluoroscopy with cumulative dose >1500 rads to a single field, or any delivery of radiotherapy to the wrong body region or >25% above the planned radiotherapy dose Other events where RCA could be considered • Near Misses • Repeated problems • Events which have resulted in patient harm, or could have resulted in patient harm – “Risk thereof” Safety Assessment Code • Assists to prioritize safety related problems • Applies resources (time) where they have the greatest opportunity to improve safety • A tool intended to prioritize safety events yet not take the place of judgment • Based on 2 dimensions Safety Assessment Code Severity: • Based on actual and potential risk – “worst case” • Needs to have consistent definition • Should be determined first Safety Assessment Code • Catastrophic – Death or major permanent loss of function not related to natural course of illness or underlying condition • Major – Permanent lessening of bodily function not related to natural course of illness or underlying condition • Moderate – Increased length of stay or level of care • Minor – No injury, no increased length of stay or level of care Safety Assessment Code Probability: • More subjective, greater chance of variation • Should be reflective of the facility • Categories – – – – Frequent Occasional Uncommon Remote Safety Assessment Matrix Frequency SEVERITY Catastrophic Major Moderate Minor Frequent 3 3 2 1 Occasional 3 2 1 1 Uncommon 3 2 1 1 Remote 3 2 1 1 Adapted from: http://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=1695 Sentinel Event Focused Review Algorithm It is determined that a focused review should be conducted Manager schedules the RCA to be conducted within 30 days of the event Measurement plan is implemented; the action plan is evaluated for effectiveness RCA documents are reviewed by medical staff in the Department Meeting (includes action plan) The RCA is conducted and an action plan is established The action plan is facilitated by the manager Root Cause Analysis • Participating in a RCA is an opportunity to learn • Opportunity for staff to tell their story • Emphasis is on improving the system and not correcting the individuals Root Cause Analysis • Systematic process for identifying the most basic causal factor or factors for an undesirable event or problem • Focus is on process and systems, not individuals • Frequently ask “why “ • Confidential • Conduct within 45 days Root Cause Analysis • Who • What • When • Where • Why Goals of a Root Cause Analysis • Mechanism for reporting Sentinel Events • Investigating and evaluating causative factors • Initiation of performance improvement • Action plan development to prevent recurrence Goals of a Root Cause Analysis Understand the sequence of events – Flow chart – Cause and Effect Diagram Chronological details can be done before to save time Reviewing literature can help the team to differentiate between what they may or may not have within their control RCA Team • Multidisciplinary : – Key staff and departments directly and indirectly involved in the event – Physicians, nurses and managers – Performance Improvement Staff Key Aspects • CONFIDENTIAL • Safe protected environment • Quality Management v.s. Risk Management • Gain better insight into processes involved in the event – Frequently asks “why” • Peer Review – MN Statute §§ 145.61 • QM acts as a facilitator Key Elements of RCA • • • • • • • • • Details of the event Human factors Staffing Communication Education Equipment Environmental Uncontrollable external factors Other factors Triage Questions • Helps team understand event • Assures thoroughness of investigation – Human factors/Communication – Human factors/Training – Human factors fatigue/scheduling – Environment/Equipment – Rules/Policies/Procedures – Barriers Minimum Scope of Root Cause Analysis for Specific Types of Sentinel Events Detailed inquiry into these areas is expected when conducting a root cause analysis for the specified type of sentinel event Inquiry into areas not checked (or listed) should be conducted as appropriate to the specific event under review. Suicide (24care) Med Error Procedure Complic Behavioral assessment process* Physical assessment process** Patient identification process Patient observation process Care planning process X Staffing levels X X X Orientation & training of staff Competency assessment/ credentialing Supervision of staff*** X X X Communication with patient/family Communication among staff members Availability of information Adequacy of technological support Equipment maintenance/ management Physical environment**** X Security systems and processes Control of medications: storage/access Labeling of medications X X Wrong site surgery Treatment delay X X Restraint death Elopement death Assault, rape,hom X X X X X X Transfusin death Infant abduction X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X X RCA Reporting Tools • Root Cause Analysis Summary • Root Cause Analysis Corrective Action Plan • Confidential under MN Statute §§ 145.61 Root Cause Analysis Summary To be thorough, a RCA must include: – Determination of human and other factors – Determine related processes and systems – Analysis of underlying causes and effects – series of why’s – Identification of risks and their potential contributions Determining the Root Cause • 5 Rules of Causation – Causal statements must clearly show the “cause and effect” relationship – Negative descriptors are not used in a causal statement – Each human error must have a preceding cause – Each procedural deviation must have a preceding cause – Failure to act is only causal when there was a pre-existing duty to act HealthEast Root Cause Analysis Summary Level of Analysis Questions/Factors involved What happened: What departments were involved? What are the details of the event? Why did it happen: What was the missing or weak (Proximate cause) step in the process? Why did that happen? What caused the missing or weak step in the process? Why did that happen? What is currently done to prevent failure at this step? Why did it happen: What was the human error? (Proximate cause) Why did that happen? Was staff performance in the process addressed? Was staff properly qualified? Was staffing adequate? Why did that happen? Can orientation and inservice training be improved? Why did it happen: Was all necessary information available: -when needed? -accurate? -complete? Why did that happen? Is communication among participants adequate? Why did that happen? Are there barriers to communication? Is prevention of adverse outcomes considered a high priority? (Proximate cause) Findings and Opportunities to Improve Why did it happen: How did the equipment fail? What broke? Why did that happen? What is currently being done to prevent an equipment failure? Why did that happen? What is currently being done to protect against a bad outcome if an equipment failure does occur? (Proximate cause) Why did it happen: What environmental factors directly affected the outcome? Why did that happen? Was the physical environment appropriate for the process to be carried out? Why did that happen? Are systems in place to identify environmental risks? Are responses to environmental risks planned and tested? (Proximate cause) Why did it happen: Were there any uncontrollable external factors? Why did that happen? Are they truly beyond the organization’s control? Why did that happen? How can we protect against them? (Proximate cause) Why did it happen: Were there any other factors that directly influenced the outcome? Why did that happen? What caused the breakdown at this step in the process? Why did that happen? How can we protect against them? (Proximate cause) Type of Event: Patient suicide Op/post-op complication Medication error Wrong-site surgery Delay in treatment Patient death/injury in restraints Patient fall Assault/rape/homicide Patient elopement Perinatal death/loss of function Transfusion error Fire Infant abduction/wrong family Medical equipment – related Ventilator death/injury Maternal death Death associated with transfer Utility system failure Anesthesia – related Infection – related Dialysis – related In-patient drug overdose Self-inflicted injury Other (less frequent) Communication with patient/family Communication among care team members Availability of information Adequacy of technological support Equipment maintenance/management Physical environment Security systems and processes Control of medications: storage/access Labeling of medications Root Cause(s) Identified by the RCA Team: Check categories that apply: Behavioral assessment process Physical assessment process Patient identification process Patient observation procedures Care planning process/coordination of care Staffing levels Orientation and training of staff Competency assessment/credentialing Supervision of staff Access to care Additional Details: Patient Name/Number: Where incident occurred: Date of incident: Date Root Cause Analysis Completed: Participants in Root Cause Analysis: Conclusions/Recommendations: Please list references of literature search: Please attach the associated policies: (articles can be found in the central library) (including any newly revised policies) See attached bibliography. Questions? Focused Review of a Sentinel Event Developing a Corrective Action Plan Corrective Action Plan • Historically the weakest link to the process • Often RCA teams conclude solutions based on: – Recognition of warning signs – Training/education – Asking clinicians to “be more careful” • Creates challenges for the RCA team Corrective Action Plan • Strong actions: – Physical plant changes – New device with usability testing prior to purchase – Forcing functions – Simplifying process – remove unnecessary steps – Standardize process/equipment – Leadership is actively involved Corrective Action Plan • Intermediate actions: – – – – – – – – Decrease workload Software enhancements/modifications Eliminate/reduce distraction Checklists/cognitive aids/triggers/prompts Eliminate look alike and sound alike Read back Enhanced documentation/communication redundancy Corrective Action Plan • Weak actions: – – – – – Double checks Warnings/labels New policies/procedures/memorandums Training/education Additional study Corrective Action Plan • Do the Actions meet the following: – Address the root cause and contributing factors – Specific – Easily understood and implemented – Developed by process owners – Measurable Corrective Action Plan • Identifies opportunities for improvement • Assigns responsibility for actions • Target dates are set for completion • Looks at follow up for effectiveness by using a measurement plan Measure of Effectiveness Why Measure? • Confirmation that what we wanted to accomplish did in fact occur • Measures effectiveness of action, not the completion of the action • “All improvement will require change, but not all change will result in improvement” G. Langley, et al • “In God we trust. All other bring data” W.E Deming How will we know that the change results in improvement? Measurement answers the question • Quality improvement measurement is for learning, not judgment, not research • All measures have limitations • Measurement should be used to guide improvement and test changes • Focus on the changes made in the action plans What to Measure Outcome Measures • Reflect cumulative impact of multiple processes • “Big picture” – Are we doing the right thing – Are we getting the results we want – Did we influence the health of the patient • Reflect the health state of a patient resulting from our care • Further investigation is needed to understand what processes need to be changed Outcome Measures • How many falls on this unit? • How many pressure ulcers occurred on this unit? • How many wrong site surgery events did we have? • How many medication errors occurred on this unit What to Measure Process Measures Reflect current condition of our processes – Are they still working for us – Are we using them – Are we using the accurately • Determine if processes are functioning effectively and efficiently • Used to assess adherence to recommendations in clinical practice • Able to identify specific areas of care that may require improvement Process Measures • How many patients had the tool to assess for risk of falls • How many patients with a Braden score of 6 had a WOC nurse consult • How many times was the pause for cause observed correctly • How many nurses matched the patient’s ID band to the MAR How to Measure Complex and untimely Guide change, indicate progress, timely • Chart abstraction • Financial reports • Data obtained from existing databases and systems • • • • • • Tally sheets Checklists Questionnaires Feedback interviews Observation Daily reviews Measure of Effectiveness Measurement Plan • Measures effectiveness of action, not the completion of the action • Defined numerator/denominator • Defined sampling plan and time frame • Realistic performance threshold • Plan for when initial measure did not meet threshold Measure of Effectiveness Measurement Plan Examples • % patients with risk assessment tool used – Randomly sample 10 patients/month for 3 months. If goal of 90% not reached, discuss with staff to determine barriers and make necessary changes, then re-audit. • % Pause for Cause observed to be correctly done by OR staff – Randomly observe 10 surgeries/month for 3 months. If goal of 90% not reached, discuss with staff to determine barriers and make necessary changes, then reaudit. Spread the Success/knowledge • Share with staff and Administration – Need to go beyond “share at staff meeting” - action is not sustained • Collaborate with other units and sites • Report sent to Medical Department for review/comments CONFIDENTIAL HealthEast Root Cause Analysis Protected under Minnesota Statute §§ 145.61 et seq. IMPROVEMENT ACTION PLAN Type of Event: Category of Root Cause: Opportunity to Improve Measures: Follow-up for Effectiveness: Action Responsible Person Target Date For Implementation Completion Date ACTION PLAN OWNER(s): HealthEast Root Cause Analysis IMPROVEMENT ACTION PLAN Opportunity to Improve Measures Follow-up for Effectiveness Action Rating Action Responsible Person Target Date For Implementati on Completi on Date Initials Questions? Thank You! Rosemary Emmons RN,BSN HealthEast Quality Management 651-232-3392 phone 651-864-2535 pager 651-232-4435 fax remmons@healtheast.org