Care Plan 27 Bipolar Disorder, Manic Episode
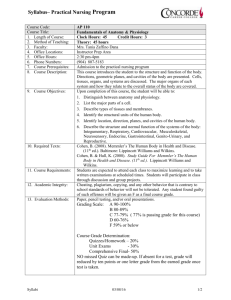
advertisement

Care Plan 27 Bipolar Disorder, Manic Episode CARE PLAN 27 Bipolar Disorder, Manic Episode Nursing Diagnosis Risk for Other-Directed Violence At risk for behaviors in which an individual demonstrates that he or she can be physically, emotionally, and/or sexually harmful to others. RISK FACTORS • • • • • • Restlessness Hyperactivity Agitation Hostile behavior Threatened or actual aggression toward self or others Low self-esteem EXPECTED OUTCOMES Immediate The client will • • • • Be safe and free from injury throughout hospitalization Demonstrate decreased restlessness, hyperactivity, and agitation within 24 to 48 hours Demonstrate decreased hostility within 2 to 4 days Refrain from harming others throughout hospitalization Stabilization The client will • Be free of restlessness, hyperactivity, and agitation • Be free of threatened or actual aggression toward self or others Community The client will • Demonstrate level moods • Express feelings of anger or frustration verbally in a safe manner From Schultz, J. M. & Videbeck, S. L. (2013). Lippincott’s Manual of Psychiatric Nursing Care Plans, 9th edition. © Wolters Kluwer Health | Lippincott Williams & Wilkins. Care Plan 27 Bipolar Disorder, Manic Episode IMPLEMENTATION Nursing Interventions * denotes collaborative interventions Rationale Provide a safe environment. See Care Plan 26: Suicidal Behavior, Care Plan 46: Hostile Behavior, and Care Plan 47: Aggressive Behavior. Physical safety of the client and others is a priority. The client may use many common items and environmental situations in a destructive manner. Administer PRN medications judiciously, preferably before the client’s behavior becomes destructive. Medications can help the client regain self-control but should not be used to control the client’s behavior for the staff’s convenience or as a substitute for working with the client’s problems. Set and maintain limits on behavior that is destructive or adversely affects others. Limits must be established by others when the client is unable to use internal controls effectively. The physical safety and emotional needs of other clients are important. Decrease environmental stimuli whenever possible. Respond to cues of agitation by removing stimuli and perhaps isolating the client; a private room may be beneficial. The client’s ability to deal with stimuli is impaired. Provide a consistent, structured environment. Let the client know what is expected of him or her. Set goals with the client as soon as possible. Consistency and structure can reassure the client. The client must know what is expected before he or she can work toward meeting those expectations. Give simple direct explanations (e.g., for procedures, tests, etc.). Do not argue with the client. The client is limited in the ability to deal with complex stimuli. Stating a limit tells the client what is expected. Arguing interjects doubt and undermines limits. Encourage the client to verbalize feelings such as anxiety and anger. Explore ways to relieve tension with the client as soon as possible. Ventilation of feelings may help relieve anxiety, anger, and so forth. Encourage supervised physical activity. Physical activity can diminish tension and hyperactivity in a healthy, nondestructive manner. From Schultz, J. M. & Videbeck, S. L. (2013). Lippincott’s Manual of Psychiatric Nursing Care Plans, 9th edition. © Wolters Kluwer Health | Lippincott Williams & Wilkins. Care Plan 27 Bipolar Disorder, Manic Episode Nursing Diagnosis Defensive Coping Repeated projection of falsely positive self-evaluation based on a self-protective pattern that defends against underlying perceived threats to positive self-regard. ASSESSMENT DATA • • • • • • • Denial of problems Exaggeration of achievements Grandiose schemes, plans, or stated self-image Buying sprees Inappropriate, bizarre, or flamboyant dress or use of makeup or jewelry Flirtatious, seductive behavior Sexual acting-out EXPECTED OUTCOMES Immediate The client will • Demonstrate more appropriate appearance (dress, use of makeup, etc.) within 2 to 3 days • Demonstrate increased feelings of self-worth within 4 to 5 days Stabilization The client will • Verbalize increased feelings of self-worth • Demonstrate appropriate appearance and behavior Community The client will • Use internal controls to modify own behavior From Schultz, J. M. & Videbeck, S. L. (2013). Lippincott’s Manual of Psychiatric Nursing Care Plans, 9th edition. © Wolters Kluwer Health | Lippincott Williams & Wilkins. Care Plan 27 Bipolar Disorder, Manic Episode IMPLEMENTATION Nursing Interventions * denotes collaborative interventions Rationale Ignore or withdraw your attention from bizarre appearance and behavior and sexual acting-out, as much as possible. Minimizing or withdrawing attention given to unacceptable behaviors can be more effective than negative reinforcement in decreasing unacceptable behavior. Set and maintain limits regarding inappropriate behaviors. Convey expectations for appropriate behavior in a nonjudgmental, matter-of-fact manner. The client needs to learn what is expected before he or she can meet expectations. Limits are intended to help the client learn appropriate behaviors, not as punishment for inappropriate behavior. You may need to limit contact between the client and other clients or restrict visitors for a period of time. Discuss the situation with the client as tolerated. The client may need to gain self-control before he or she can tolerate the presence of other people and behave in an appropriate manner. Initially, give the client short-term, simple projects or activities. Gradually increase the number and complexity of activities and responsibilities. Give feedback at each level of accomplishment. The client may be limited in the ability to deal with complex tasks. Any task that the client is able to complete provides an opportunity for positive feedback. Give client positive feedback whenever appropriate. Positive feedback provides reinforcement for the client’s growth and can enhance self-esteem. It is essential to support the client in positive ways and not to give attention only for unacceptable behaviors. From Schultz, J. M. & Videbeck, S. L. (2013). Lippincott’s Manual of Psychiatric Nursing Care Plans, 9th edition. © Wolters Kluwer Health | Lippincott Williams & Wilkins. Care Plan 27 Bipolar Disorder, Manic Episode Nursing Diagnosis Disturbed Thought Processes* Disruption in cognitive operations and activities. *Note: This nursing diagnosis was retired in NANDA-I Nursing Diagnoses: Definitions & Classification 2009–2011, but the NANDA-I Diagnosis Development Committee encourages work to be done on retired diagnoses toward resubmission for inclusion in the taxonomy. ASSESSMENT DATA • • • • • • • Disorientation Decreased concentration, short attention span Loose associations (loosely and poorly associated ideas) Push of speech (rapid, forced speech) Tangentiality of ideas and speech Hallucinations Delusions EXPECTED OUTCOMES Immediate The client will • • • • Demonstrate orientation to person, place, and time within 24 hours Demonstrate decreased hallucinations or delusions within 24 to 48 hours Demonstrate decreased push of speech, tangentiality, loose associations within 24 to 48 hours Demonstrate an increased attention span, for example, talk with staff about one topic for 5 minutes, or engage in one activity for 10 minutes, within 2 to 3 days • Talk with others about present reality within 2 to 3 days Stabilization The client will • Demonstrate orientation to person, place, and time • Demonstrate adequate cognitive functioning Community The client will • Sustain concentration and attention to complete tasks and function independently • Be free of delusions or hallucinations From Schultz, J. M. & Videbeck, S. L. (2013). Lippincott’s Manual of Psychiatric Nursing Care Plans, 9th edition. © Wolters Kluwer Health | Lippincott Williams & Wilkins. Care Plan 27 Bipolar Disorder, Manic Episode IMPLEMENTATION Nursing Interventions * denotes collaborative interventions Rationale Set and maintain limits on behavior that is destructive or adversely affects others. Limits must be established by others when the client is unable to use internal controls effectively. The physical safety and emotional needs of other clients are important. See Care Plan 21: Delusions, Care Plan 22: Hallucinations, and Care Plan 46: Hostile Behavior. Initially, assign the client to the same staff members when possible, but keep in mind the stress of working with a client with manic behavior for extended periods of time. Consistency can reassure the client. Working with this client may be difficult and tiring due to his or her agitation, hyperactivity, and so on. See Care Plan 1: Building a Trust Relationship. Decrease environmental stimuli whenever possible. Respond to cues of increased agitation by removing stimuli and perhaps isolating the client; a private room may be beneficial. The client’s ability to deal with stimuli is impaired. Reorient the client to person, place, and time as indicated (call the client by name, tell the client your name, tell the client where he or she is, etc.). Repeated presentation of reality is concrete reinforcement for the client. *Provide a consistent, structured environment. Let the client know what is expected of him or her. Set goals with the client as soon as possible. Consistency and structure can reassure the client. The client must know what is expected before he or she can work toward meeting those expectations. Spend time with the client. Your physical presence is reality. Show acceptance of the client as a person. The client is acceptable as a person regardless of his or her behaviors, which may or may not be acceptable. Use a firm yet calm, relaxed approach. Your presence and manner will help to communicate your interest, expectations, and limits, as well as your self-control. Make only promises you can realistically keep. Breaking a promise will result in the client’s mistrust and is detrimental to a therapeutic relationship. Limit the size and frequency of group activities based on the client’s level of tolerance. The client’s ability to respond to others and to deal with increased amounts and complexity of stimuli is impaired. Help the client plan activities within his or her scope of achievement. The client’s attention span is short, and his or her ability to deal with complex stimuli is impaired. Avoid highly competitive activities. Competitive situations can exacerbate the client’s hostile feelings or reinforce low self-esteem. From Schultz, J. M. & Videbeck, S. L. (2013). Lippincott’s Manual of Psychiatric Nursing Care Plans, 9th edition. © Wolters Kluwer Health | Lippincott Williams & Wilkins. Care Plan 27 Bipolar Disorder, Manic Episode *Evaluate the client’s tolerance for group activities, interactions with others, or visitors, and limit these accordingly. The client is unable to provide limits and may be unaware of his or her impaired ability to deal with others. Encourage the client’s appropriate expression of feelings regarding treatment or discharge plans. Support any realistic plans the patient proposes. Positive support can reinforce the client’s healthy expression of feelings, realistic plans, and responsible behavior after discharge. See Care Plan 18: Dual Diagnosis. Substance abuse often is a problem in clients with bipolar disorder. From Schultz, J. M. & Videbeck, S. L. (2013). Lippincott’s Manual of Psychiatric Nursing Care Plans, 9th edition. © Wolters Kluwer Health | Lippincott Williams & Wilkins. Care Plan 27 Bipolar Disorder, Manic Episode Nursing Diagnosis Bathing Self-Care Deficit Impaired ability to perform or complete bathing activities for self. Dressing Self-Care Deficit Impaired ability to perform or complete dressing activities for self. Feeding Self-Care Deficit Impaired ability to perform or complete self-feeding activities. Toileting Self-Care Deficit Impaired ability to perform or complete toileting activities for self. ASSESSMENT DATA • • • • • • • • • Inability to take responsibility for meeting basic health and self-care needs Inadequate food and fluid intake Inattention to personal needs Impaired personal support system Lack of ability to make judgments regarding health and self-care needs Lack of awareness of personal needs Hyperactivity Insomnia Fatigue EXPECTED OUTCOMES Immediate The client will • Participate in self-care activities, such as bathing, grooming, with nursing assistance, within 24 hours • Establish adequate nutrition, hydration, and elimination, with nursing assistance, within 24 to 48 hours (e.g., eat at least 30% of meals) • Establish an adequate balance of rest, sleep, and activity, within 48 to 72 hours (e.g., sleep at least 3 hours per night within 48 hours) Stabilization The client will • Maintain adequate nutrition, hydration, and elimination, for example, eat at least 70% of meals by a specified date • Maintain an adequate balance of rest, sleep, and activity, for example, sleep at least 5 hours by a specified date From Schultz, J. M. & Videbeck, S. L. (2013). Lippincott’s Manual of Psychiatric Nursing Care Plans, 9th edition. © Wolters Kluwer Health | Lippincott Williams & Wilkins. Care Plan 27 Bipolar Disorder, Manic Episode Community The client will • Meet personal needs independently • Recognize signs of impending relapse IMPLEMENTATION Nursing Interventions * denotes collaborative interventions Rationale Monitor the client’s calorie, protein, and fluid intake. You may need to record intake and output. The client may be unaware of physical needs or may ignore feelings of thirst and hunger. The client may need a high-calorie diet and supplemental feedings. The client’s increased activity increases nutrition requirements. Provide foods that the client can carry with him or her (fortified milkshakes, sandwiches, “finger foods”). See Care Plan 52: The Client Who Will Not Eat. If the client is unable or unwilling to sit and eat, highly nutritious foods that require little effort to eat may be effective. Monitor the client’s elimination patterns. The client may be unaware of or ignore the need to defecate. Constipation is a frequent adverse effect of antipsychotic medications. Provide time for a rest period during the client’s daily schedule. The client’s increased activity increases his or her need for rest. Observe the client for signs of fatigue and monitor his or her sleep patterns. The client may be unaware of fatigue or may ignore the need for rest. Decrease stimuli before bedtime (dim lights, turn off television). Limiting stimuli will help encourage rest and sleep. Use comfort measures or sleeping medication if needed. Comfort measures and medications can enhance the ability to sleep. Encourage the client to follow a routine of sleeping at night rather than during the day; limit interaction with the client at night and allow only a short nap during the day. See Care Plan 38: Sleep Disorders. Talking with the client during night hours will interfere with sleep by stimulating the client and giving attention for not sleeping. Sleeping excessively during the day may decrease the client’s ability to sleep at night. If necessary, assist the client with personal hygiene, including mouth care, bathing, dressing, and laundering clothes. The client may be unaware of or lack interest in hygiene. Personal hygiene can foster feelings of well-being and self-esteem. Encourage the client to meet as many of his or her own needs as possible. The client must be encouraged to be as independent as possible to promote self-esteem. From Schultz, J. M. & Videbeck, S. L. (2013). Lippincott’s Manual of Psychiatric Nursing Care Plans, 9th edition. © Wolters Kluwer Health | Lippincott Williams & Wilkins. Care Plan 27 Bipolar Disorder, Manic Episode Nursing Diagnosis Deficient Knowledge (Specify) Absence or deficiency of cognitive information related to a specific topic. ASSESSMENT DATA • Inappropriate behavior related to self-care • Inadequate retention of information presented • Inadequate understanding of information presented EXPECTED OUTCOMES Immediate The client will • Acknowledge his or her illness and need for treatment within 48 hours • Participate in learning about his or her illness, treatment, and safe use of medications within 4 to 5 days Stabilization The client will • • • • Verbalize knowledge of his or her illness Demonstrate knowledge of adverse and toxic effects of medications Demonstrate continued compliance with chemotherapy Verbalize knowledge and acceptance of the need for continued therapy, chemotherapy, regular blood tests, and so forth Community The client will • Participate in follow-up care, for example, make and keep follow-up appointments • Manage medication regimen independently From Schultz, J. M. & Videbeck, S. L. (2013). Lippincott’s Manual of Psychiatric Nursing Care Plans, 9th edition. © Wolters Kluwer Health | Lippincott Williams & Wilkins. Care Plan 27 Bipolar Disorder, Manic Episode IMPLEMENTATION Nursing Interventions * denotes collaborative interventions Rationale *Teach the client and family or significant others about manic behavior, bipolar disorder, and other problems as indicated. The client and family or significant others may have little or no knowledge of disease processes or need for continued treatment. *Teach the client and family or significant others about signs of relapse, such as insomnia, decreased nutrition, and poor personal hygiene. If the client and his or her family or significant others can recognize signs of impending relapse, the client can seek treatment to avoid relapse. *Inform the client and family or significant others about chemotherapy: dosage, need to take the medication only as prescribed, the toxic symptoms, the need to monitor blood levels, and other considerations. Some medications, such as oxcarbazepine (Trileptal), lamotrigine (Lamictal), valproic acid (Depakote), and gabapentin (Neurontin) may be contraindicated in clients with impaired liver, renal, or cardiac functioning. Safe and effective use of medications may require maintenance and monitoring of therapeutic blood levels. When the therapeutic level is exceeded, toxicity can result. See Appendix E: Psychopharmacology for a listing of signs and symptoms that may indicate toxic or near-toxic blood levels. *Stress to the client and family or significant others that medications must be taken regularly and continually to be effective; medications should not be discontinued just because the client’s mood is level. A relatively constant blood level, within the therapeutic range, is necessary for successful maintenance treatment with lithium and valproic acid. *Explain information in clear, simple terms. Reinforce teaching with written material as indicated. Ask the client and significant others to state their understanding of the material as you explain. Encourage the client to ask questions and to express feelings and concerns. The client and significant others may have little or no understanding of medications and toxicity. Asking for the client’s perception of the material and encouraging questions will help to eliminate misunderstanding and miscommunication. From Schultz, J. M. & Videbeck, S. L. (2013). Lippincott’s Manual of Psychiatric Nursing Care Plans, 9th edition. © Wolters Kluwer Health | Lippincott Williams & Wilkins.