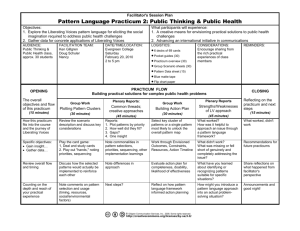
practicum paper - Professional Portfolio Erin K. Kibbey, BS, RN, CCRN
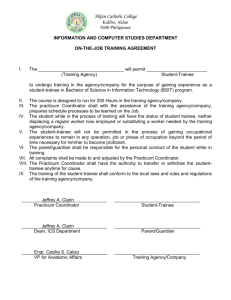
advertisement

Running head: CLINICAL PRACTICUM 1 Nurse Educator and NPD Specialist Clinical Practicum Paper Erin Kibbey Ferris State University CLINICAL PRACTICUM 2 Abstract Gaining competency in the role of the nurse educator and nursing professional development specialist can be obtained through the utilization of a practicum experience. This paper describes a practicum experience designed to gain experience and practical knowledge related to the educational process utilized by both of these specialty roles. The three standards of practice this practicum experience focused on included: a) facilitation of learning, b) participation in curriculum design and evaluation of program outcomes, and c) use of assessment and evaluation strategies. Based on these competencies and guided by Kolb’s experiential learning theory, several key objectives and activities were completed during this experience. This paper describes challenges related to the application of these roles, strategies applied to address the challenges, description and analysis of clinical projects completed during the project, and an evaluation of the practicum. Keywords: competency, nurse educator, nursing professional development specialist, standards of practice CLINICAL PRACTICUM 3 Nurse Educator and NPD Specialist Clinical Practicum Paper According to the American Nurses Association and National Nursing Staff Development Organization (ANA & NNSDO, 2010) the nursing professional development (NPD) specialist uses their expertise in nursing education to help other nurses develop their competence in various settings. They support continuous learning and help create an environment that supports the adult learning process. Competencies related to the educational process including assessment, planning, implementation, and evaluation are the same for both NPD specialists and academic nurse educators (Brunt, 2007). This practicum was designed to gain confidence and skills related to the educational process within both of these specialty roles. The purpose of this paper is to describe the clinical practicum experience, including role issues and challenges, strategies utilized to address role challenges, clinical projects completed, and evaluation of the practicum. The importance of obtaining hands-on, practical experience prior to taking on a new role cannot be underestimated. As a future academic nurse educator or NPD specialist, fulfillment of a 300 hour clinical practicum experience provided the opportunity to gain competency towards these roles. The following paper describes the clinical practicum intended to provide experience in the educational process similar to both of these specialty roles. Practicum Overview The overall goal of the clinical practicum was to gain competency in the specialty roles of the NPD specialist and nurse educator as based on my previous background and clinical experience and future career goals. Since the educational process utilized by these roles is a competency area I had little experience in, this practicum was designed to specifically focus on growth in this area. As such, this practicum focused on three particular National League for Nursing (NLN, 2012) standards of practice. These three standards included: the facilitation of CLINICAL PRACTICUM 4 learning, participation in curriculum design and evaluation of program outcomes, and the use of assessment and evaluation strategies (2012). Although these standards are specific to the nurse educator role, the NPD specialist has several responsibilities related to these education based standards. Some of the key responsibilities for NPD specialists related to educational competency include: assessing and validating competency, assessing educational needs, participating in on-the-job activities, orienting, assisting in role transition, and developing curricula (ANA & NNSDO, 2010). Thus, several of these responsibilities were integrated into the clinical practicum experience. Finally, the practicum experience provided several additional opportunities for growth in the ANA and NNSDO (2010) standards of leadership, collegiality, and collaboration. In order to gain competency in the educational process as an NPD specialist and nurse educator, this practicum took place at Munson Medical Center (MMC) in Traverse City, Michigan. Within this setting, I gained experience in the educational process by working closely with the program coordinator for the critical care internship program as well as the transition to practice program. The coordinator for both of these programs, Ms. Hresko, was also my preceptor for the clinical practicum experience. Foundational Theory Progression of competency within the three nurse educator standards of practice were designed based on Kolb’s experiential learning theory. From this theory comes the notion that ideas are not fixed, they are shaped and reshaped through experience (Kolb, 1984). Thus, learning is a process that continually changes through experience. Also central to this theory is the idea that learning involves the environment and real-world experience. In addition, learning CLINICAL PRACTICUM 5 is a cyclical, adaptive process occurring in all human settings and all life stages. This practicum amplified these ideas and provided the foundation for the clinical practicum. Objectives for the practicum were based on Kolb’s (1984) idea that the experiential learning cycle is a continuous process. The first objective for the practicum was to become acclimated to the educator role and educational process through observation. The second objective was to reflect on the observational experiences and the third objective was to apply knowledge and actively participate in the educational process. This is similar to Kolb’s (1984) idea that individuals have a concrete experience, they reflect on that experience, they derive meaning from it, and they try out the meaning they’ve constructed (Jeffries & Clochesy, 2012). Additional objectives for the practicum were based on the desire to further apply the proposed concrete experiences, as Kolb’s theory suggests. Issues, Challenges, and Strategies In retrospect, five main challenges related to implementation of the NPD specialist and educator roles were encountered during the practicum experience. These issues related to role clarity, assessing learning needs, anxiety about teaching, organizing and planning, and communication. Several strategies and approaches were applied in order to gain further experience in these roles and to ultimately allow for a successful practicum experience. Congruence of Role Expectations Since this practicum was completed at MMC, where I am also a staff nurse employee, one of the first issues of concern was the congruence of expectations to individuals encountered while immersed in the practicum. Since I was also working with Ms. Hresko for completion of another Ferris course, I had similar concerns about the need to clarify and differentiate expectations and practicum goals compared to the other course. In addition, as I progressed CLINICAL PRACTICUM 6 within the practicum experience, there were various individuals that requested my help with projects or endeavors that they felt would be mutually beneficial. Some of the time I was able to help with these requests and still work towards my own practicum goals. However, I did feel that I had to continually ensure the expectations of others still met the practicum goals for development in the NPD specialist and educator roles. According to McKinley (2008), expectations of nursing administration, management, and staff may not be mutually exclusive, which can result in educators feeling frustrated and spread too thin. There were a few times throughout the practicum where Ms. Hresko and I were involved in several different projects, roles, and responsibilities, occasionally resulting in an inability to complete some of the tasks we had planned on completing for the day. Similarly, it was a challenge to keep in mind that there are limitations to the role. As McKinley (2008) notes, the clinical educator cannot fix every problem, nor do they have the answer to every question. Strategies. One of the main strategies evoked at the beginning of the practicum was to share with Ms. Hresko the practicum planning guide I had previously created (see Appendix A). By sharing the goals and objectives for the practicum with Ms. Hresko, she was able to have a clearer picture of what the practicum experience intended to focus on. From the beginning, providing clarity about expectations is essential to implementation of the educator role (McKinley, 2008). In addition, establishment of goals and an outline of specific activities and responsibilities for a defined time frame can assist the educator in establishing successful implementation of the educator role (2008). Another strategy employed to clarify my role outside of my normal job at MMC was to dress differently than I do as a staff nurse. On the unit I typically work, I wear burgundy colored scrubs. Once I was visiting units as a student instructor, I wore blue hospital scrubs. This CLINICAL PRACTICUM 7 usually caused those that I typically work with to question why I was wearing something different, resulting in a conversation that clarified my role as a student instructor for the critical care interns. Outside of the hospital units, Ms. Hresko also announced my presence at meetings and clarified my role. A similar approach was taken with individuals that approached me about helping them with various projects. I carefully consulted with the individuals and clarified what my role would be and considered how the activity would be beneficial to my own goals and whether it was appropriate to take part. For example, I was able to help on several occasions in the simulation lab, allowing valuable experience in the facilitator and operator roles. However, before taking part in these opportunities, achieving clarity about expectations, time commitment, and goals, were key to these being successful experiences for all parties involved. Assessing Learning Needs At the onset of the practicum, I was unsure as to how Ms. Hresko had obtained her insight into what the course learning needs may be for the next class of critical care interns. She had several ideas about what needed to be included in the next class, but it was not until I saw the stacks of folders with raw evaluation in her filing cabinet that I began to understand some of the ways she had assessed learning needs. I was surprised and overwhelmed with the amount of evaluation data pertaining to the internship that had been collected over the years. Accordingly, needs assessments for clinical educators can be both formal and informal (McKinley, 2008). Although Ms. Hresko had clearly looked at feedback, test results, and worked closely with the past interns, I was concerned about the lack of compilation of the data that could have been further analyzed to assess learning gaps. For instance, the written tests that had been given to past interns could have been used to identify areas of education that needed strengthening in CLINICAL PRACTICUM 8 order to achieve program outcomes (McKinley, 2008). However, the raw evaluations, as well as the pre and post internship knowledge tests were in a filing cabinet but had never been placed into a usable form. According to Avillion, Brunt, and Ferrell (2007), a needs assessment can identify specific needs, validate the needs to key stakeholders, and document the identified needs into a format that can be developed. Because these items were never placed into a format where the data could be meaningfully interpreted, it was difficult for me to assess the potential learning needs for the next class of critical care interns. Strategies. In order to fix the issue of unclear needs assessment data, I compiled the pre and post test results from the Basic Knowledge Assessment Tool for Critical Care (BKAT). This tool is an example of a test that can be used to assess the knowledge level of staff and are available for various nursing care specialties (Toth, 2008). The BKAT-7 or the BKAT-8 were given to all the previous classes of interns at the start of the critical care internship program and then again at the end of the internship program. Since the results of how the interns had improved and what content areas they were still having difficulty with were never placed into any kind of spreadsheet and analyzed, I spent a great deal of time completing this process. In scoring the BKAT’s there is an answer sheet and score sheet that tells what content area the question pertains to (such as emergency situations, electrocardiogram interpretation, monitoring of lines, ventilators, etc.). Toth (2008), the author of the BKAT, noted that the BKAT can be useful for identifying needed content and as a measure of learning. Content areas were tabulated across each of the interns. In total, I tabulated results from 28 interns that completed the BKAT8. All 90 questions were examined on both the pre-test and post-test, so this was quite a bit of data to record. CLINICAL PRACTICUM 9 Once I was able to interview and spend more time with the new class of interns I was also able to begin less formally assessing learning needs. Gaberson and Oermann (2010) note that the first area of assessment involves understanding the learner’s current level of knowledge, skill, and attitude. Interactions with interns while on the various critical care units were utilized as an opportunity to assess the current level of knowledge and skill and other characteristics that could influence achievement of the internships learning outcomes. In addition, e-journals and post conferences were helpful for assessing learning gaps and identifying accomplishments in clinical practice. A second assessment area should consider individual characteristics that could potentially influence performance (Gaberson & Oermann, 2010). “Understanding the background, experience, and style of learners, determining the number of learners, and focusing on the desired outcome must all be a part of the assessment for the educator to select the best approach to learning” (McKinley, 2008, p. 392). Finally, another strategy for assessing learning needs is to assess possible barriers to learning (2008). Time, motivation, lack of resources, lack of support, and resistance to change are potential roadblocks to learning. Thus, all of these considerations were utilized in the assessment of learning needs and planning of clinical learning approaches, as well as the development of the first clinical project (see Appendix B). Anxiety about Teaching As a novice to the nurse educator role, one of the biggest concerns I had going into this practicum was worrying about my ability to help new nurses, new critical care nurses, and the critical care interns learn the essential knowledge and skills to become a competent nurse. As Penn, Wilson, and Rosseter (2008) point out, “many nurses who have spent years in the practice setting are only vaguely aware of what is involved in teaching…” (p. 6). This was true in my case. Although, I have been a preceptor, spent the last six years as a bedside nurse, and was CLINICAL PRACTICUM 10 starting my last semester of graduate school, I had never been immersed in the educator role outside of the unit I worked. Moving out of my comfort zone and teaching in other areas with nurses I did not know, was a new experience that definitely evoked some concern at the start of the practicum. Research has identified effective teachers as knowing how to teach, being clinically competent, supportive, patient, friendly, and having the ability to maintain collegial relationships with students and staff (Stokes & Kost, 2012). Educators must also have the ability to deliver knowledge in an effective manner (2012). Since I was new to the role, I was concerned about my ability to portray these qualities and actually be an effective teacher. Strategies. Consequently, the ability to help students’ master essential skills and knowledge in order to become professional nurses is so paramount that the need for preparation and development of individuals taking on teaching roles is an important issue (Stokes & Kost, 2012). Therefore, through a variety of experiences, both observational and experimental, my learning and knowledge about facilitation grew, allowing me to become more comfortable with teaching. As previously mentioned, the proposed practicum was designed based on Kolb’s experiential learning theory and cycle of learning. Within Kolb’s cycle of learning the various learning processes can include concrete experience, reflective observation, abstract conceptualization, or active experimentation (Ullrich & Haffer, 2009). Thus, in this practicum I utilized this process in order to gain confidence and ease my fears about teaching. I began by watching and carefully observing my preceptor and the speaker at the first role transition class, then reflected on the experiences, and finally I began refining and improving my comfort level with teaching through active experimentation. Imperative to Kolb’s cycle of learning framework was the opportunity to interact with Ms. Hresko, several other educators, and my graduate degree program peers that I got to know CLINICAL PRACTICUM 11 throughout the practicum. Not only did these individuals serve as mentors and guides to the educator role, but they helped me feel welcome and encouraged throughout the process. In a study by Schoening (2013) it was found that peer mentors provided beneficial emotional support during the role transition process from nurse to nurse educator. According to Penn et al. (2008), faculty mentors and professional development opportunities that promote learning about the teaching environment and opportunities to enhance teaching skills should be encouraged for novice educators. Participating as a facilitator in a role transition class was my first attempt at teaching in this practicum. The first and main focus during this time was on creating the right tone for students to feel comfortable sharing, especially with the difficult topics that were presented in the class. According to the NLN (2012), facilitation of learning can be accomplished by creating an environment conducive for students to learn the desired outcomes. In addition, I knew it was also important, as noted by the NLN (2012), to display interest and respect for the learners. I shared stories that demonstrated patience, caring, and integrity. Attending the simulation facilitator class was another strategy utilized to become more comfortable with teaching and facilitating. It was extremely useful to utilize the information learned from the beginning of the facilitator class and apply it when assigned to act as a facilitator. I essentially practiced being a facilitator, without having real students. This opportunity provided individualized attention in both the operator and facilitator roles. In addition, I was able to obtain feedback from the other learner and the class instructor on my facilitator techniques. Finally, I had the opportunity to practice debriefing and to discuss effective ways to debrief. This approach was very helpful in decreasing my anxiety related to facilitation and debriefing. CLINICAL PRACTICUM 12 According to Shellenbarger and Edwards (2012), simulation activities can benefit graduate nurse educator students. Accordingly, simulation activities can be a useful way for novice nurse educators to create scenarios for simulation so they can practice the skills of planning, implementing, and evaluating teaching and learning skills. Thus, not only was it beneficial to learn this technology for future use, but the process of learning and practicing using it throughout this practicum helped me gain experience in feeling more comfortable with teaching as well as planning, which was another challenge as described in the following section. Organizing and Planning Throughout the clinical practicum experience, there were several hours spent planning and organizing. McDonald (2010), notes that many educators take work home with them and that an excessive workload for educators is often a factor in faculty retention. From the beginning, I realized this was a potential issue for the success of my practicum experience. Since Ms. Hresko’s educator position was only a 24 hour a week position this was a concern from the start and one that felt like we had to frequently come to terms with. Duties that included teaching, preparation, administrative meetings, and other committee meetings often times left us both with the added burden of planning and organizing outside of MMC. Educators must also prepare students for orienting to the clinical environment, be familiar with the clinical setting, and know the knowledge and skill level needed in the practice area where teaching will take place (Gaberson & Oermann, 2010). During the transition stage from nurse to nurse educator, one of tendencies for novice educators is to over prepare for student encounters (Schoening, 2013). This was a real challenge at the onset of this practicum. Before facilitating in skills sessions, I often spent several hours preparing myself for teaching content that I was already very familiar with. This concern CLINICAL PRACTICUM 13 seemed to coincide with my anxiety of teaching. According to Schoening (2013), novice educators that over prepare may fear failure due to a lack of experience. In planning my first clinical project, the physical assessment simulation, I also spent several hours not only in creating the lesson plan but playing the facilitation over in my head and researching how to perform a proper head-to-toe assessment. As a critical care nurse of nearly six years, I am very comfortable performing head-to-toe assessments, but I felt the need to prepare and plan for the learning activity more than what I believe would be required for an educator that is more confident in their role. Strategies. One strategy I utilized to deal with organizational and planning issues was to frequently consult my calendar and carve out time for necessary tasks. Utilizing the practicum planning guide (see Appendix A), I placed all of the activities and responsibilities Ms. Hresko and I had committed to into a calendar. I frequently consulted my calendar and estimated the length of time it would take to carry out various tasks and plugged those in as necessary. Ms. Hresko and I frequently communicated via email and telephone in order to ensure we were prepared for the planned activities. Planning for the lessons also became easier with practice. In addition, when I came to the realization that I would never be completely prepared for every single question that could be asked or for every contingency that could occur, I began to lighten up on my planning. According to Schoening (2013), faculty that successfully transitioned from nurse to nurse educator identified the strategy of focusing on the learning process, rather than the product. Thus, teaching became more learner focused than content-focused. This was something I still need practice with, but was a mindset I tried to utilize as I continued in my practicum experience. CLINICAL PRACTICUM 14 Communication One of the biggest issues and concerns encountered during this practicum experience was related to the topic of communication. According to McKinley (2008), communication is essential to the success of any role but even more so for that of an educator. Moreover, McKinley (2008) notes that unclear, indirect, inefficient, and poor communication techniques can result in frustration and failure. Finally, the NLN (2012) notes that an important competency for the nurse educator is to practice skilled oral, written, and electronic communication. In addition, communication should reflect awareness about one’s self and others as well as convey ideas in a range of situations (2012). This concern was important in my interactions with the critical care interns. Emphasis on the lines of communication on clinical units, who to go to for help, and under what circumstances they should seek help were important issues that needed to be communicated to students, or in this case the interns, before they entered the critical care units (Gaberson & Oermann, 2012). Providing feedback that is constructive and respectful was another concern I had during the practicum experience, due to my lack of experience in this area. Often evaluation is one of the most intimating skills for new educators (Penn et al., 2008). Another example of a communication concern that occurred earlier in the practicum was when the last class of interns were working on their case study presentations. This was the final component to the internship program and was scheduled for March 14. An issue that came about in relation to communication was the lack of guidelines about Ms. Hresko’s expectations for the presentations. In talking with some of the past interns, as well as Ms. Hresko, there was no description of what the presentation should entail or identification of how the interns would be evaluated based on the presentation. CLINICAL PRACTICUM 15 Another important consideration when communicating with learners is that too much information can result in overload and shutting down communication (McKinley, 2008). According to Penn et al. (2008), the ability to differentiate between critical content and logically sequencing the information to maximize learning is an important communication consideration. On the first day of the internship, the interns were given a huge binder of unit specific articles, the syllabus I developed, the electrocardiogram course book, and the skills lab book. It was very apparent that this approach resulted in overload and a portrayal of being overwhelmed. Finally, promoting clear communication with internship preceptors, unit managers, and others encountered throughout the practicum was another important concern related to communication. During one of the meetings I attended about the development of the professional practice model, I was called on to voice my opinion about the idea of back rubs being part of the model. Knowing that this topic was a source of contention amongst the group, it was a concern that poor communication about my thoughts on this subject could result in a poor outcome. Lastly, there was an issue with an intern feeling unwelcomed on one of the critical care units and proper communication in handling this problem was critical for all parties involved. Strategies. One strategy utilized to promote communication to the interns related to the issue about the case presentations was to provide clear, written expectations for the assignment as well as a copy of the tool that would be utilized to evaluate the interns on. As such, rubrics are a type of rating scale and can be used to help provide a clear direction for grading and assignment criteria (Bonnel, 2012). Since the case presentations by the interns are an important evaluation component to the internship program, it was deemed necessary by myself and Ms. Hresko that a rubric could be utilized to help facilitate a clearer understanding of the CLINICAL PRACTICUM 16 expectations for the presentation. Rubrics can be a convenient form for providing feedback and allows for more discrimination in judging than checklists (Bonnel, 2012). While a rubric worked well for the case study presentation, a checklist was utilized for the physical assessment simulation learning activity. The use of a checklist, in this instance, provided me, the observer, with clear criteria for evaluation resulting in feedback that was viewed as fair, direct, constructive, and respectful. Another strategy utilized to combat communication challenges was my promotion of credibility. McKinley (2008) has said that real-world credibility is an essential component that needs to be portrayed by the educator. Hence, having appropriate credentials, experience, and knowledge can communicate a message of credibility (2008). In meeting with the interns it was conveyed by both Ms. Hresko and myself that we were both still critical care staff nurses, had obtained critical care certification, and had several years of experience at the bedside. Similarly, another strategy that is important to communicating credibility is just being available, dressing the part, and bringing forth a positive attitude (2008). When working with the interns, I met with them on a daily basis, wore scrubs, lent a hand with patient care, and was available throughout the day. Additional communication strategies utilized throughout the practicum focused on the use of personal attributes. Accordingly, the NLN (2012) facilitation of learning competency notes the importance of using personal attributes such as caring, confidence, patience, integrity and flexibility. This strategy is also supported by studies that have found faculty considered the most successful by students when they possessed attributes such as enthusiasm, flexibility, a sense of humor, approachability, and respectfulness (Penn et al., 2008). Key to promoting a positive learning environment is the fostering of collegial working relationships with the CLINICAL PRACTICUM 17 personnel in the clinical learning environment (NLN, 2012; Gaberson & Oermann, 2010). Thus, Ms. Hresko and I had several discussions with preceptors, unit educators, unit managers, and unit coordinators in order to keep communication open and foster trusting relationships with staff members. Clinical Project The fourth competency for the nurse educator, or the ability to participate in curriculum design and evaluate program outcomes, should reflect today’s health care and educate graduates to be effective nurses in the modern day health care milieu (NLN, 2012). In light of current health care trends such as the increasing critical nature of patient illness, increasing emphasis on high quality care, and decreased spending, it is important for curriculum to keep pace (Boland, 2012). In order to help accomplish the goal of developing competency in curriculum design and evaluation of program outcomes, I originally planned to develop two didactic lessons that could be incorporated into the critical care internship program. However, after developing the first lesson, outlined in the following section, the opportunity to develop a program syllabus became a second clinical project. Clinical Project 1: Lesson Plan After careful consideration of learning needs as previously discussed, Ms. Hresko suggested I plan a simulation activity focused on how to conduct a proper physical assessment and the differences encountered on the critical care patient. This learning topic was one Ms. Hresko had identified as an area for potential growth based on feedback from preceptors and interns in previous classes. In addition, according to Gaberson and Oermann (2010), clinical instructors are responsible for assessing the level of skill development prior to entrance in to the clinical setting. Thus, utilization of simulation settings or skills labs can provide this opportunity CLINICAL PRACTICUM 18 before being expected to do so in a fast-paced, demanding environment like critical care (Gaberson & Oermann, 2010). Once a time and date were established, I coordinated the reservations for the simulation lab where the learning activity would take place. I also obtained materials to help in not only designing the simulation activity, but also in evaluation of the activity and learning outcomes. I utilized a teaching outline the staff development and simulation coordinator sent to me, in order to begin writing the teaching plan for the simulation. This project utilized adult learning theory as well as evidence based practice for developing lesson plans, needs assessments and learning objectives. According to Knowles (1980) theory of adult learning, adults prefer learning that is practical, promotes self-esteem, utilizes past experiences, demonstrates respect and allows self-direction, and synthesizes new ideas with previous knowledge. In looking at the development of a teaching lesson for simulation, I first focused on the objectives, outcomes, and competencies of what the desired outcome was for the simulation activity (see Appendix B). Identification of the learners and their level of expertise, including knowledge gaps, was an essential step in creating the learning activity with adult learning theory in mind. According to Billings (2012), each lesson should state the purpose, outcomes, assignments, learning activities, and evaluation being used. Since the identified learning gap was performing a physical assessment on a critically ill, hospitalized patient, the learning outcomes focused on improving clinical performance and self-confidence. The introduction of the critically ill patient in the simulation lab, early in the orientation period, was felt to be a safe and less threatening way of learning how to perform a complete physical assessment and become familiar with some of the equipment that would be seen throughout the orientation period. In addition, the design of this activity considered potential past knowledge with a plan to integrate new knowledge related to critical care, as adult learning CLINICAL PRACTICUM 19 theory suggests. According to Jeffries and Clochesy (2012), simulation can provide a safe environment conducive to learning skills that require practicing a number of times. The learning outcomes and placement of this particular simulation learning activity at the beginning of critical care orientation was also in line with the idea that learning activities should build from level to level and be threaded throughout the course as they fit with the program outcomes (Billings, 2012). Moreover, the simulation activity could assist with a more effective method of measuring the skill and level of comfort the interns possessed before allowing them on the critical care units (Billings, 2012). The last stage in developing the lesson plan was determining evaluation methods. According to Saunders (2003), this should be a twofold evaluation, considering evaluation of learning or outcomes and evaluation of the instruction or the process. Primary strategies for evaluating and measuring learning in a clinical setting is through observation, written communication, oral communication, simulation, and self-evaluation (Bonnel, 2012). Accordingly, Bonnel (2012) notes the importance of creating a checklist of behaviors and skills to be observed during the simulation or performance so the potential for direct visualization and confirmation of student performance is easier to evaluate. In working on the competencies and evaluation for the simulation activity MMC’s intranet and information from the Lippincott reference manual were utilized. Thus, organizational and nursing standards were followed and considered throughout the development of this activity. Since structured observational tools can contribute to a more objective and fair evaluation, I created an evaluation checklist based on information from the previously mentioned sources. An analysis of the evaluations for this project will be discussed further in the evaluation section of this paper. CLINICAL PRACTICUM 20 Clinical Project 2: Program Syllabus Prior to the start of the critical care internship on March 13, I learned that there was no program syllabus. A syllabus can be seen as an important component to student understanding of what is expected of them throughout a course. According to Sauter, Nightingale Gillespie, and Knepp (2012), the syllabus can also be used during review of instructors and effectiveness in teaching. Furthermore, the syllabus should be reviewed for expectations that are clear and evaluation methods that are detailed. I found that Ms. Hresko did have written program goals but there was really nothing formal, written, and given out to the interns that described all the things that a normal program syllabus would contain. Since I was still working toward gaining experience in the competency of curriculum design and evaluation of program outcomes, I believed working on the components of a program syllabus and putting them all together would provide me with additional growth in this area. According to Billings (2012), the syllabus sets the tone for the course and should start off by being written in a welcoming style. In addition she says a title, purpose, description, prerequisites, corequisites, outcomes, teaching-learning strategies, learning activities, topical outline, policies and procedures, assessment and evaluation strategies, as well as the grading plan should be standard and essential components in a syllabus. Keeping this information in mind and the difference between creating the program’s syllabus I needed to create for the internship to one that would be created for an academic course, I set out to the task of creating a program syllabus (see Appendix C). In doing this, I also had to email the electrocardiogram class instructor and request course information to add to the syllabus about this program component. The first step to creating the internship syllabus was to figure out the course outcomes. Although, my preceptor had already created some broader program objectives, I felt the syllabus CLINICAL PRACTICUM 21 needed to have more specific intern learning outcomes. Objectives and outcomes specify what students should know, do, value, and determine how they will be graded (Billings, 2012). Dillard and Siktberg (2012) also note that objectives and outcomes provide the framework for the curriculum. In addition, learning activities and course objectives should focus on the three main domains of learning, the cognitive, affective, and psychomotor domain. By matching objectives with learning activities students are better able to make connections between what the content is and why it is important, thus, promoting learning. One resource I utilized for this component was the American Association of Critical-Care Nurse’s website for information about the learning objectives related to the online modules that the internship utilizes for didactic learning. According to Dillard and Siktberg (2012), one way to demonstrate that learning objectives match the assignments is to use an evaluation grid or matrix. Therefore, I did create a grid to demonstrate how the learning objectives would be assessed. One observation noted after creating the grid was that in looking at all the various learning activities utilized in the internship program, there was a great mix of active and passive learning approaches. Evaluation According to Saunders (2003), instructional evaluation can be done formally or informally. Informal examples could include remarks from learners during the class session. Thus, the evaluation of the first clinical project, the simulation activity, was completed using both of these methods. Informal examples included remarks from the group during the simulation activity. Comments made by the interns during the simulation activity itself were very positive. In addition, the interns were all very engaged throughout the learning session, each taking on the role of the nurse performing the physical assessment. An evaluation form for the simulation learning activity was also created (see Appendix D). The beginning of the CLINICAL PRACTICUM 22 evaluation form was created based on the learning objectives for the simulation. It has been shown that student ratings are considered highly reliable as well as positively correlated with student achievement, however, there remains challenges with the validity and reliability of the instrument used to evaluate teaching effectiveness (Hayes, 2011). The rest of the evaluation form utilized for the simulation activity was a standard form created and used by MMC for the simulation lab. The evaluation consisted of a Likert five point scale, asking the learner to rate how they felt about various evaluation criteria. Likert scales are the most widely used scaling technique (Polit & Beck, 2012). A Likert scale allows the evaluator the opportunity to express an opinion on a particular issue through indicating the degree to which they agree or disagree (Bourke & Ihrke, 2012). Overall, each of the intern’s evaluations reflected strong, positive feelings towards the learning activity. All responses were marked “strongly agree” related to their feeling of whether or not they were able to achieve the learning objectives for the activity. In addition, one of the comments made on the evaluation noted that hands on learning was a preferred learning method. Lastly, no remarks were made on the evaluations suggesting recommendations for future simulations. An evaluation tool was also created as a means of assessing how well the goals for the entire practicum were met (see Appendix E). The evaluation was completed by myself and Ms. Hresko. The evaluations were based on the standards of practices for the academic nurse educator as outlined by the NLN (2012). Both of these evaluations also utilized a Likert five point scale. Overall, I believe this was a successful practicum experience. Significant experience was gained in not only the specified areas outlined on the evaluation, but also in learning more about the nurse educator and NPD specialist roles related to leadership and change in an organization. Ms. Hresko’s evaluation was also highly rated. CLINICAL PRACTICUM 23 Formal evaluation forms administered to students are often used by institutions at the end of a course in order to solicit feedback on various criteria and are another way to receive feedback (Saunders, 2003). Thus, at the end of this practicum I created an evaluation form that once again utilized a Likert five point scale (see Appendix F). The evaluation form was given to the interns on April 25, 2014 by Ms. Hresko when I was not present. The evaluations were collected and given back to me by Ms. Hresko in order to provide the interns with an opportunity to submit the evaluations anonymously. Evaluations from the interns were overall very positive. On each of the 21 questions, all interns rated me as “excellent”, which was at the top of the scale provided. Additional comments provided were also positive in nature. Lastly, in telling the interns that I would not be working with them anymore, I received several informal comments that they were going to miss me and that they were really grateful for my help. Conclusion Obtaining experience and knowledge in the educational process is an important goal in the development of the academic nurse educator and NPD specialist roles. Competency in the educational process can be gained through the utilization of a practicum experience. This paper described a practicum experience designed to expand competency related to the educational process utilized by both of these roles. Kolb’s experiential learning theory was described as the foundation for the practicum experience. Challenges encountered in implementing these roles as well as the strategies applied to meet these challenges were also detailed. Lastly, this paper described and analyzed the clinical projects undertaken during the practicum and provided an evaluation of the practicum experience. CLINICAL PRACTICUM 24 References American Nurses Association and National Nursing Staff Development Organization [ANA & NNSDO]. (2010). Nursing professional development: Scope and standards of practice. Silver Spring, MD: Nursesbooks.org. Avillion, A., Brunt, B., & Ferrell, M. J. (2007). Nursing professional development: Nursing review and resource manual (1st ed.). Silver Spring, MD: American Nurses Credentialing Center. Boland, D. (2012). Developing curriculum: Frameworks, outcomes, and competencies. In D. Billings & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 138159). St. Louis, MO: Elsevier Saunders. Bonnel, W. (2012). Clinical performance evaluation. In D. Billings & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 485-502). St. Louis, MO: Elsevier Saunders. Bourke, M. P. & Ihrke, B. A. (2012). The evaluation process: An overview. In D. Billings & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 422-440). St. Louis, MO: Elsevier Saunders. Brunt, B. A. (2007). Competencies for staff educators: Tools to evaluate and enhance nursing professional development. Danvers, MA: HCPro, Inc. Gaberson, K. & Oermann, M. (2010). Clinical teaching strategies in nursing (3rd ed.). NY: Springer Publishing Company. Hayes, J. (2011). Student evaluation of teaching. In M. Bradshaw & A. Lowenstein (Eds.), Innovative teaching strategies in nursing and related health professions (5th ed.). (pp. 563-574). Sudbury, MA: Jones & Bartlett Publishers. CLINICAL PRACTICUM 25 Jeffries, P. R. & Clochesy, J. M. (2012). Clinical simulations: An experiential, student-centered pedagogical approach. In D. Billings & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 352-368). St. Louis, MO: Elsevier Saunders. Knowles, M.S. (1980). The modern practice of adult learning. Chicago, IL: Follett. Kolb, D. (1984). Experiential learning: Experience as the source of learning and development. Englewood Cliffs, NJ: Prentice Hall. Retrieved from http://academic.regis.edu/ed205/kolb.pdf McDonald, P. (2009). Transitioning from clinical practice to nursing faculty: Lessons learned. Journal of Nursing Education, 49(3), 126-131. doi:10.3928/01484834-20091022-02 McKinley, M. (2008). Walking on water and other lessons learned as a clinical educator. AACN Advanced Critical Care, 19(4), 388-395. National League for Nursing [NLN]. (2012). The scope of practice for academic nurse educators 2012 revision. NY: author. Penn, B., Wilson, L., & Rosseter, R. (2008). Transitioning from nursing practice to a teaching role. OJIN: The Online Journal of Issues in Nursing, 13(3), 1-14. Polit, D. F. & Beck, C. T. (2012). Nursing research: Generating and assessing evidence for nursing practice (9th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. Saunders, R. (2003). Constructing a lesson plan. Journal for Nurses in Staff Development, 19(2), 70-80. Schoening, A. M. (2013). From bedside to classroom: The nurse educator transition model. Nursing Educator Research, 34(3), 167-172. CLINICAL PRACTICUM 26 Shellenbarger, T. & Edwards, T. (2012). Nurse educator simulation: Preparing faculty for clinical nurse educator roles. Clinical Simulation in Nursing, 8(6), 249-255. doi:10.1016/j.ecns.2010.12.006 Stokes, L. G. & Kost, G. C. (2012). Teaching in the clinical setting. In D. Billings & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 311-334). St. Louis, MO: Elsevier Saunders. Toth, J. (2008). The basic knowledge assessment tool, version eight (BKAT-8): For adult critical care nursing. Retrieved from http://www.bkat-toth.org/BKAT-8.html. Ullrich, S. & Haffer, A. (2009). Precepting in nursing: Developing an effective workforce. Sudbury, MA: Jones and Bartlett Publishers. CLINICAL PRACTICUM 27 Appendix A Project Planning Guide Title of Project: Practicum Proposal for Nurse Educator or NPD Specialist Goals Goal 1: Develop knowledge and experience in the standards of practice for both the education domain of the advanced specialty role of the NPD specialist and competencies I – Facilitate Learning & III – Use Assessment & Evaluation Strategies for the advanced specialty role of the nurse educator (ANA & NNSDO, 2010; NLN, 2012) Objectives 1.1 Orient to the clinical educator/staff development role at MMC through multiple observation experiences focused on facilitation of learning and the use of assessment and evaluation strategies 1.2 Use reflective observation to gain knowledge in facilitation of learning techniques and evaluation strategies Activities 1.1a Observe preceptor facilitation in one role transition class & review class evaluations Timeline 1.1a Jan. 16 1.1b Participate in interviews and selection process of candidates for internship program 1.1b January 1.1c Observe facilitator and preparation of EKG course for new nurses 1.1c Feb. 20, 27, Mar. 6, Mar. 13, Mar. 20 1.1d Shadow preceptor and her interactions, facilitation of learning, and use of assessment and evaluation techniques with the interns, unit educators, and managers 1.1d Mar. 10 – May 2 1.1e Meet with preceptor and interns during any scheduled learning sessions 1.1e Internship starts Mar. 10 1.2a 1.2a Engage in weekly to bi-weekly Jan. 13- May reflection and journaling of 2, 2014 experiences 1.2b Meet regularly with preceptor to discuss, evaluate, and plan experiences for professional growth 1.2b Jan. 13-May 2, 2014 CLINICAL PRACTICUM 1.3 Take on an active role as a facilitator of learning in the clinical setting 28 1.3a Help preceptor with preparation for start of internship program (preparing program materials, schedules, coordination with unit educators/managers) 1.3a Jan. 13- Mar. 9 1.3b Teach stations at skills labs 1.3b Feb. 26 & Mar. 20 1.3c Participate as facilitator in transition classes 1.4 Implement assessment and evaluation strategies into active facilitation experiences 1.5 Use simulation technology for facilitation of learning in at least one lab session 1.3c Feb., Mar., Apr. (1 day month for 3 hrs.) 1.3d Select meetings with interns and preceptor to focus the planning and leading of 1.3d Select 1-2 Fridays in April 1.3e Facilitate agreed upon topics in March EKG course 1.3e Mar. 27, Apr. 10, Apr. 17, Apr. 24, May 1 1.4a Use evaluation strategies and review outcomes from facilitation at skills labs 1.4a February 26 & March 20 1.4b Use evaluation strategies and review outcomes from facilitation in role transition classes 1.4b Feb., Mar., Apr. (1 day month for 3 hrs.) 1.5a Attend 4 hour simulation operator class 1.5a By end of February 1.5b Attend 4 hour simulation 1.5b By end of CLINICAL PRACTICUM Goal 2: Gain knowledge and experience in the NLN (2012) nurse educator competency IV – Participation in Curriculum Design and Evaluation of Program Outcomes 2.1 Implement at least two didactic lessons into existing educational materials for the critical care interns 29 facilitator class February 1.5c Facilitate simulation scenario(s) at skills lab(s) and with interns, use debriefing and evaluation strategies 1.5c April 30 & various date(s) once internship program starts in March 2.1a Meet with preceptor to determine gaps in program learning outcomes 2.1a Jan. 13 – Jan 27 2.1b Create an outline of education needs 2.1b Jan.27 – Feb. 10 2.1c Review the literature on topics that need additional educational facilitation of learning 2.1c Feb. 10 – Feb. 17 2.1d Revise curricula and write learning objectives and select appropriate learning activities to fulfill needs 2.1d Feb. 17 – Mar. 3 2.1e Determine and implement evaluation strategies appropriate to the interns and learning goals for new curricula 2.1e Mar. 3 – Mar. 10 CLINICAL PRACTICUM 30 Appendix B Clinical Project 1 High-fidelity Simulation Case Planning Munson Medical Center Scenario name: Critical Care Physical Assessment Simulation Estimated scenario run time: 20 minutes each intern Estimated debriefing time: 40 minutes Target audience: Critical Care Interns Location of simulation: Simulation Lab Learning gap: Physical assessment of critically ill hospitalized patient What outcome/s are you measuring? Clinical performance Brief overview: Fran York is a 75-year-old Caucasian female that lives alone. Her husband Jack passed away a year ago. She has a cat, Pumpkin, who is very important to her. Fran has one daughter, Phoebe Miller, who is 52, lives nearby, and is Fran's major support system. Self-confidence Her current medical problems include: hypertension, atrial fibrillation, glaucoma, osteoarthritis of the knee, stress incontinence, osteoporosis, and hypercholesterolemia. Fran is taking several anti-hypertensive medications, diuretics, Coumadin, and analgesics. She was admitted to the hospital last night with a diagnosis of urinary tract infection, dehydration, and change in mental status. The scenario takes place at 7:00 AM shift change. Fran has been in her room on A2 for about six hours. Due to her confusion, Fran did not take her medications properly in the CLINICAL PRACTICUM 31 days prior to admission and as a result, her blood pressure is very elevated. Fran's daughter, Phoebe is at the bedside and is quite concerned about the confusion and elevated blood pressure. The learner receives handoff report from the previous nurse and is expected to perform and document a general assessment. Learning objectives: At the end of the simulation, the participant will be able to: - Perform a complete systematic head to toe assessment of a simulated patient. - Identify major alterations in assessment findings: elevated blood pressure, confusion, rhonchi, murmur - Evaluate the data - Respect and maintain patient privacy within the context of the examination. - Implement patient safety standards throughout the assessment. -Communicate clearly to patient, family member and all members of the healthcare team. Simulation outcome checklist See attached (Lippincott skills checklist, ACLS, NRP or other Monitor Layout List parameters that you want to show: Initially just the ECG, once student assesses then add as they assess the BP, temp, SpO2 Patient Description Name Fran York Age 75 years old Weight and Height 48 kg, 61 inches Gender Female History of present complaint Fran’s daughter became concerned yesterday when she stopped over to check on her and found her still in her CLINICAL PRACTICUM 32 bathrobe at 3:00 PM. The house was very unkempt, and Fran couldn’t remember her daughter’s name. Fran was brought to the emergency department by her daughter and she was admitted to A2 around midnight. U/A, CBC, and basic metabolic panel labs have been completed and sent to the lab. Results are available. Setting A2 - Acute care hospital unit Patient Info: Religion: Lutheran History, Meds, Allergies and Physician/s Emergency Contact: Phoebe (daughter). Phone: 555-1210 Allergies: No known allergies Immunizations: Influenza & pneumonia (2 years ago) Attending Physician/Team: Dr. Yost Past Medical History: Glaucoma, hypertension, atrial fibrillation, osteoarthritis, stress incontinence, hypercholesterolemia Social History: Widow for one year; involved in church activities and gardening. Daughter and grandchildren live nearby. Primary Medical Diagnosis: Dehydration; UTI Surgeries/Procedures & Dates: Cholecystectomy at age 30 CLINICAL PRACTICUM 33 Show this information on the monitor before starting the simulation. Initially just the ECG, once student assesses then add as they assess the BP, temp, SpO2 Make this information available throughout the simulation. Significant Lab Values: Urine Analysis: Color: dark amber, cloudy Specific gravity: 1.050 (normal 1.005-1.035) ph 6.0 (normal 4.5-8.0) RBC - 9 (normal 0-2) WBC - 150,000 (normal 0-5) Basic Metabolic Panel Na - 149 K - 3.5 Glucose - 105 CBC H/H - 9.9/32 WBC 12,000 Physician Orders: Bedrest Bathroom privileges with assistance Regular, low fat diet I&0 Home Medications: captopril, metoprolol, furosemide, Coumadin, Lipitor, CLINICAL PRACTICUM 34 pilocarpine eye drops, Fosamax, Celebrex, Tramodol for arthritis pain prn Continue home medications and add: ciprofloxacin 200 mg IV q 12 hours acetaminophen prn IV fluids D5 .45 NaCl 20 mEq KCL at 60ml/hr List equipment needed: A. B. C. D. E. F. G. H. I. J. K. L. SimMan and equipment & SimMan 3G and equipment Ventilator (not used in the simulation but will be used after) Central line Telemetry Wound Chest tube Stage I pressure ulcer Foley IV pole, pump, with IV solutions, bags with expiration dates Computer with Powerchart training mode Checklist for evaluation Facilitator cards Prep of the simulator: I. Content outline A. Introduce students to expectations of simulation a. Treat SimMan as you would a real patient. i. Manikin talks (unless vented), blinks, has pulses, heart sounds, breath sounds, etc. b. Student learning objectives include: i. Conduct a head-to-toe assessment of the patient ii. Identify critical assessment findings (will be outlined on outcome checklist) iii. Evaluate patient data iv. Use SBAR techniques when communicating with other members of the health care team v. Document patient assessment c. Facilitator will be a family member and observe, will be given a role card d. Facilitator can answer questions about what manikin can do. e. After the simulation you will be charting your assessment in Powerchart f. At the end, the team will debrief. CLINICAL PRACTICUM 35 B. Intro. To SimMan a. Capabilities: pulse oxygen can be applied, take BP b. Gather all of your assessment data is if it was a real live patient c. Check IV and medications C. Simulation a. Physical Assessment on non-vented pt with SimMan software i. Receive report 1. FY is a 75-year-old female admitted from home with confusion. Her daughter noticed she wasn’t making sense or acting right when she stopped in to visit her yesterday evening. Her daughter brought her in to the ED yesterday afternoon; she was in the ED until about midnight. FY has a history of hypertension, atrial fibrillation, glaucoma, osteoporosis, arthritis, elevated cholesterol, and stress incontinence. It is unclear whether she has taken her medications properly the past few days, her daughter couldn't tell from looking at her medication box. Labs just came back, I haven’t had a chance to look at them. She has medications ordered, but they just came up from pharmacy and they all need to be given. She has not had any pain. Number of roles and participants per scenario: 2 Primary nurse - Intern Family member - Facilitator CLINICAL PRACTICUM Timing (approxi mate) and Patient Monitor Settings 36 Patient/Manikin (Actions) (Actions) Student Expected Interventions Cue/Prompt (Events) Frame Name Initial: Initial State: Vocal Sounds: 0-5 minutes Vital Signs “My daughter dropped me off and left me here. I’m not quite sure where I am or why I’m here. I feel ok. I can’t believe how my life has changed in the past couple of weeks now. Howard died a couple of weeks, no months ago. I can’t remember. Why can’t I remember? Things have changed. I don’t like that; I’ve always been a strong woman. I feel ok and I take a lot of pills – not sure what they all are you can look on the kitchen counter or ask my daughter what they are. Where is Phoebe? I haven’t seen her in 6 years; no one ever comes to see me.” Only initial display is heart rhythm/rate (pt is on a tele monitored floor) Once interns takes vitals then display BP, spO2, temp BP 180/110, P – 100, Afib R – 25 (do not display, want to check accuracy of intern’s assessment); T - 98.4 Wash hands Introduce self Identify patient Take vital signs Begins headto-toe assessment Role member providing cue: Daughter Cue: “I don't think she's been taking her medicine.” What advances frame to next frame? CLINICAL PRACTICUM 37 Heart, lung sounds etc. Murmur Rhonchi 5-10 minutes Complains of headache “Has anyone checked on Pumpkin lately?" Continues assessment Notice elevated BP Role member providing cue: Daughter – 7-8 minutes into scenario Cue: “Isn’t her blood pressure too high?” 10-20 minutes (If student asks about medications) “I don't remember when I took my Lopressor last.” Continues to complains of headache Calls Dr. Yost to notify of BP using SBAR communicatio n tool Completes physical assessment Role member providing cue: Dr. Yost Cue: “Has she taken her antihypertensiv e? I’ll be there shortly” Debriefing outline/questions: A. B. C. D. E. F. G. What do you think went well? How did you feel throughout the simulation experience? Did you have the knowledge and skills to meet objectives? What were the key assessment findings and interventions? What would you do differently if we repeated the simulation? How can you apply this to your clinical practice? Differences in assessment techniques with a vented pt. a. Demonstrate on other manikin H. Discuss areas for improvement. CLINICAL PRACTICUM 38 Physical Assessment Evaluation Criteria General Gather appropriate equipment Performs hand hygiene Puts on gloves, if necessary Introduce self Identify the pt Provide privacy and maintain pt dignity Explain your purpose Checks patient concerns (chief complaint) prior to start of assessment Physical environment (temp, cleanliness, equipment in use or in room) Inspection - using senses of vision, smell, and hearing to observe condition of various body parts, including any deviations from normal Visually surveys the patient (details of appearance, overall condition, body habitus) Makes sure body area being inspected is sufficiently exposed and adequately lit, noting overall condition, color, shape, texture, odor, sound, and size LOC Disposition (facial expressions, mood, behavior) Note tubes, drains, IV's, etc. (include amount, color, odor, etc.) Always looks before touching Performs Vital Signs Palpation - touching and feeling body parts with hands to determine the following characteristics Texture (roughness, smoothness) Temperature (warm/hot/cold) Moisture (dry/wet/moist) Motion (stillness/vibration) Consistency of structures (solid/fluid filled) Tender areas are palpated last Auscultation - Listening for various breath, heart, vasculature, and bowel sounds using a stethoscope Lungs Heart Bowels Vasculature Additional Considerations Provide opportunity for patient to ask questions, express concerns, etc. Pt bed in lowest position once complete Lock bed wheels if necessary Call light within reach and pt is aware of how to use Bedside table and personal items are within reach Performs appropriate documentation of nursing assessment CLINICAL PRACTICUM 39 References: Lippincott Procedures – Assessment techniques, Ventilator management; Lippincott Skills Checklist – Assessment techniques, Cardiac Assessment Weber, J. (2010). Nurses’ handbook of health assessment (7th ed.). Philadelphia, PA: Lippincott Williams & Wilkins CLINICAL PRACTICUM 40 Appendix C Clinical Project 2 Critical Care Internship Program Program Description The purpose of the Critical care Internship program is to provide the novice nurse with the essential foundation to safely care for patients and their families with in the critical care environment. The program consists of five months of clinical and didactic training. Program Objectives 1. Provide a consistent approach for critical care orientation. 2. Reduce nurse turnover and attrition in the critical care units. 3. Establish a supportive environment to promote nurse maturation, acceptance and successful transition from academia to the RN role. 4. Provide a sustained approach for addressing the critical care shortage and current vacancy rates. 5. Attract new critical care recruits through an internship-marketing program. 6. Promote overall job satisfaction for program participants and existing staff. 7. Foster an educational environment that supports critical thinking and evidenced based practice. 8. Maintain AACN practice standards and healthy work environment initiatives. 9. Endorse Relationship Based Care principles. 10. Establish preceptoring and mentoring role components to support skill acquisition and position integration. 11. Facilitate competency through AACN’s ECCO module test scores, Skills lab competencies, Simulation competencies, EKG class exercises, blended learning activities, self-evaluation, and unit Educator, preceptor and program coordinator evaluations. 12. Provide safe, quality, critical care to fulfill the community need. Program Teaching Strategies Clinical Practicum with Preceptor(s) Computer based modules via Essentials of Critical Care Orientation (ECCO) by the American Association of Critical-Care Nurses (AACN) Hands-on Skills Labs CLINICAL PRACTICUM 41 High Fidelity Simulation Articles Basic ECG Interpretation Classroom Course Case Studies/Clinical Reasoning Activities Guided Self-Reflection Conferences/Face-to-Face Meetings Program Schedule Please see the program calendar for information on specific dates of required labs, classes, meeting times, etc. Interns will be notified of changes to the schedule via email. It is the intern’s responsibility to check his/her outlook email to be aware of schedule changes. Program Coordinator Information Patti Hresko, MSN, RN, CCRN Critical Care Internship Coordinator Office: South One (Offices past payroll) Phone: O: (231) 392-0193 H: (231) 264-9193 C: (231) 590-9968 phresko@mhc.net Preferred method of contact: Email Participating Clinical Units Emergency Department (ED) o Offers state-of-the-art design and technology with 43 private rooms, including three full service trauma bays. Accredited through The American College of Surgeons as a Level II Trauma Center, the only one in northern Michigan. o Manager: Kristi Johnson o Resource Clinician/Unit Educator: Rachel Blanchard Intensive Care Unit (ICU) o 20-bed unit that serves a combined medical/surgical, trauma, and neurological population. The Progressive Care Unit is housed in the ICU and is responsible for caring for a variety of patients with multisystem complexity. o Manager: Jerry Huron o Resource Clinician/Unit Educator: Cathy Mowbry Cardiothoracic Unit (A2) o 30-bed unit which encourages open visitation. The innovative acuity adaptable rooms are designed to provide efficient care to cardiac surgical patients, immediately post-op until patient discharge. o Manager: Eva Voisin o Resource Clinician/Unit Educator: Jeanette Reynolds Cardiac Care Unit (A3) CLINICAL PRACTICUM 42 o 30-bed unit in the Webber Heart Center is also acuity-adaptable. A3 serves a patient population that includes adult cardiac critically ill and cardiac interventional patients. o Manager: Lori Kirkey o Resource Clinician/Unit Educator: Julie Bergsma Program Materials The following materials will be provided for you: Critical Care Internship binder with research articles and relevant critical care nursing information ECCO skills lab book Policies You are accountable for your own learning which includes keeping track of changes to the program syllabus and calendar made by the coordinator and unit schedulers throughout the program. It is the intern’s responsibility to contact the program coordinator with any issues, concerns, or questions related to the internship program. The Internship covers a large amount of material. It is imperative to keep up with assigned ECCO modules. Professional conduct is expected at all times including dress code and social media policies. Please review Munson’s employee handbook. Program Learning Outcomes By the end of the internship program, the critical care intern will be able to: 1. Identify and implement evidence-based care strategies to prevent hospitalassociated infections and complications. 2. Evaluate assessment data and develop a plan of care for patients with critical illness. 3. Understand basic hemodynamic monitoring concepts. 4. Identify the clinical consequences of basic cardiac arrhythmias and choose interventions that are appropriate for basic cardiac arrhythmias. 5. Demonstrate knowledge of common conditions experienced by acutely ill patients requiring critical care nursing. 6. Develop a treatment plan for patients experiencing critical illness. 7. Evaluate the effectiveness of the treatment plan for patients experiencing critical illness. 8. Analyze and evaluate the role of the critical care nurse and seek to improve the quality and effectiveness of nursing practice. CLINICAL PRACTICUM 43 Program Learning Activities & Assessment Methods Assessment Activity Clinical Competency Orientation Tool & Weekly Goal Sheets Outcome(s) Assessed Due Date 1, 2, 3, 4, 5, 6, 7, 8 Weekly 3, 5 Start of internship & end of internship 1, 2, 3, 5, 6, 7 6 modules must be completed prior to skills labs, rest must be completed by end of internship 2, 3, 4, 5, 6, 7, 8 See course calendar 4 May 1, 2014 1, 2, 5, 6, 7, 8 End of internship 1, 2, 3, 4, 5, 6, 7, 8 Throughout orientation program 8 Weekly Basic Knowledge Assessment Test (BKAT) ECCO Module Exams Skills Lab & Simulation Competency Tools ECG Exam Case Study Presentation Case Studies/Clinical Reasoning Activities Reflection Journals Description of Required Learning Activities Clinical Practicum with Preceptor(s) A. Goal: To provide opportunities for the student to gain knowledge and participate in patient care. B. Description: Upon completion of hospital orientation, the intern will rotate on each of the four participating critical care units for approximately one week per unit. This is considered the familiarization period. After familiarization, the intern will be assigned to one of the critical care units. The intern will spend the next 4 months of their clinical practicum on their assigned unit to complete critical care orientation. C. Objectives a. During familiarization the critical care intern will: i. Have an understanding of the various patient diagnoses treated on the participating critical care units ii. Meet interdisciplinary team members on participating units. iii. b. At the end of the clinical practicum the critical care intern will: i. Become aware of the various aspects of nursing care as an interdisciplinary component of patient care. ii. Identify the operation of the department, i.e. 1. Duties and functions of the various personnel 2. Equipment CLINICAL PRACTICUM 44 3. Role-play with the interdisciplinary team using SBAR Communication 4. Use information and patient care technology to communicate effectively with members of the healthcare team iii. Observe and/or assist with the use of treatments and therapeutic measures related to the department. 1. Administer and document administration of medications in the critical care environment 2. For assigned patients, compare observed practices with published standards. iv. Identify the need for skills in assessment based on all body systems. 1. Perform patient assessment and evaluation of patient’s response to pharmacological agents v. Identify the skills needed in patient and family teaching. 1. Address end-of-life decision making vi. Provide emotional support for the client, family members as needed. 1. Provide evidence-based, patient-centered end-of-life care to a dying patient and their significant others. vii. Infection control 1. Reporting communicable diseases required 2. Universal Precautions D. Evaluation: Clinical Competency Orientation Tool & Weekly Goal Sheets Basic Knowledge Assessment Test (BKAT) A. The BKAT is a 90-item paper and pencil test that measures basic knowledge in critical care nursing. These items measure content related to the following areas of critical care nursing practice: cardiovascular, pulmonary, monitoring lines, neurology, endocrine, renal, gastrointestinal/parenteral, infection control, hypothermia, burns, and spiritual care. B. The BKAT will be taken once at the beginning of the internship program and once at the completion of the program to assess knowledge attainment. ECCO Module Exams A. ECCO is comprised of 10 critical care training modules; each containing multiple lessons that provide in-depth, interactive content. Each module addresses the anatomy and physiology of a distinct body system, relevant diagnostic information and the clinical presentation and management of common disorders for each of the body systems. B. A variety of media formats are used in the modules including: text, audio, video, animation, and tests. C. Interns will be paid 62 hours of educational time for completion of the ECCO modules. Modules that correlate with the skills lab topics should be completed PRIOR to attending skills lab. All other modules are required to be completed by the end of the orientation program. D. Module content includes: a. Introduction to Care of the Critically Ill CLINICAL PRACTICUM b. c. d. e. f. g. h. i. j. 45 Care of the Patient with Cardiovascular Disorders Care of the Patient with Pulmonary Disorders Basic Hemodynamic Monitoring Care of the Patient with Neurological Disorders Care of the Patient with Gastrointestinal Disorders Care of the Patient with Renal Disorders Care of the Patient with Endocrine Disorders Care of the Patient with Hematological Disorders Care of the Patient with Multisystem Disorders ECCO Skills Labs, Simulation, & Case Studies A. There will be four skills labs tailored for “hands-on” learning to take place over five major content areas that correlate with ECCO learning modules including: cardiovascular, pulmonary, hemodynamics, and neuro/multisystem (neuro and multisystem are combined into one skills lab). B. See ECCO skills lab description sheet on the next page for information about meeting locations, times, and topics covered for each of the four skills labs. C. Simulation and unfolding case studies, as well as written case studies will be also be utilized throughout the orientation program. The purpose of these learning opportunities is to promote critical thinking, clinical reasoning, and adherence to internal and external standards of care. During simulation, the interns will often work together to care for a patient (simulated by a manikin) as a specified scenario unfolds. The intern is expected to fully engage and participate in the simulation session. CLINICAL PRACTICUM Pulmonary: May 28, 2014 46 ECCO Skills Lab: January 2014 – April 2014 All Skills Labs Are Located In Meeting Room 11 & 12 Time: 0800-1230 Cardiovascular: Hemodynamics: June 25, 2014 July 30, 2014 Neuro & Multi-System: April 30, 2014 Estimated pre-assignment completion time: 12.75 hours Estimated pre-assignment completion time: 15.5 hours Estimated pre-assignment completion time: 12.75 hours Estimated pre-assignment completion time: 13.25 hours ECCO modules which must be completed prior to attending skills lab: ECCO modules which must be completed prior to attending skills lab: ECCO modules which must be completed prior to attending skills lab: ECCO modules which must be completed prior to attending skills lab: Introduction to Critical Care Nursing (4.5) Pulmonary (8.25) Respiratory distress & Intubation Ventilators/CPAP/ BiPAP Trach care & suctioning ABG’s Cardiovascular (15.5) Cardiac assessment Groin management Heart sounds Temporary pacemakers Permanent pacemakers Arterial lines Hemodynamics (8.75) PA Catheter Modules (4) PA Caths: Insertion & SVO2 PA Caths: Waveforms and Trouble-Shooting PA Caths: Blood draws & Removal PA Caths: Cardiac Output Mega Code CVP Neurologic (8.75) Multi-System (4.5) Neurological Assessment Multi-system/Sepsis Simulation Neuro Simulation/ICP Neuro Case Studies Organ Donation Clinical Experience: Patient care with preceptor relevant to ECCO topics covered Adjunct Learning Activities: Policy/procedure review/case review (on unit) Don’t forget to complete all other ECCO modules by the end of the internship program Renal, GI, Endocrine, and Hematology CLINICAL PRACTICUM 47 Basic ECG Interpretation Course A. Focus of Course Content: The content of the course will focus on basic ECG interpretation skills for cardiac monitoring that a nurse needs to utilize in the care of critically ill patients. B. Hours and Length of Course: Basic ECG Interpretation classroom time occurs once a week for five weeks. The classroom time total is 9 hours. Class time per day varies according to the week. The education may have nursing contact hours. Participants will spend at least 6 hours outside of class reading, studying and completing homework. C. Rationale of the Course: Most critically ill patients will be on a cardiac monitor. Cardiac monitoring takes place in areas like telemetry units, acute critical care, the emergency room, recovery room, outpatient and procedural areas, obstetric units, pediatric units and interventional radiology. Basic ECG interpretation is a valuable skill to have. This course provides the opportunity to practice and learn the skills of interpreting cardiac rhythms that will help the critically ill patient. Nurses need to take the interpretation in context with the patient, and make a decision for interventions and education. D. Course Description: The Basic ECG Interpretation education is a blended learning experience. Students are expected to complete the assigned reading and review prior to each class. During the class time, an instructor will review the key points. Learning activities will include interpreting strips and case studies to strengthen concepts and skills. E. Course Outcomes: At the completion of the Basic ECG Interpretation course, the participant will be able to: a. Interpret basic cardiac rhythms using a standard process. b. Identify the clinical consequences of basic cardiac rhythms. c. Choose interventions that are appropriate for basic cardiac rhythms. d. Identify key points for patient education regarding basic cardiac rhythms and their interventions. F. Course Delivery Method: This education will be presented weekly in a classroom setting. The course provides an opportunity for the learner to practice and develop the basic ECG Interpretation skills needed in the critical care environment. This delivery format follows adult learning principles and experiential learning. The learning activities will engage visual, auditory, verbal, social and physical learners. The use of technology will engage the millennial generation. G. Attendance Policy: Interns are expected to attend all sessions as this learning activity is required for their position in the critical care department. If an interns is ill or unable to attend, they must call the Basic ECG Interpretation course instructor and also the internship program coordinator. The session content will need to be completed either on the nursing unit with their preceptor or educator, or during the next cycle of Basic ECG Interpretation. H. Course Instructors: a. Nancy Irish, MSN, RN-BC has taught Basic ECG Interpretation since 1997. She has over 20 years of critical care experience in cardiac, surgical and emergency critical care. She also performed 12 lead ECGs and interpretation for home care cardiac patients. She graduated with an ADN from CLINICAL PRACTICUM I. J. K. L. 48 Northwestern Michigan College in 1979, a BSN from Ferris State University in 1993, and an MSN from Walden University in 2012. Email is the best method of contact: nirish@mhc.net or phone: 935-7275. b. Debra Hart, MSN, BS, RN has been one of the primary and/or substitute teachers of Basic ECG Interpretation since 1988. She has over 15 years of cardiovascular patient care experience in acute and critical care settings. Deb graduated with an ADN from Northwestern Michigan College in 1974, a BS in Allied Health Education from Ferris State University in 1987, and an MSN from Walden University in 1012. Email is the best method of contact: dhart1@mhc.net or phone: 935-6498. Course Resources: a. Aehlert, B. (2013). ECG’s made easy (5th ed.). St. Louis: Mosby Year Book, Inc. b. Atwood, S., Stanton, C., & Storey-Davenport, J. (2009). Introduction to basic cardiac dysrhythmias (4th ed.). China: Mosby Jems Elsevier c. Dubin, D. (2011) Rapid interpretation of ECG’s (6th ed.). Hong Kong:COVER Inc. d. Wolters Kluwer, & Lippincott, Williams & Wilkins. (2011). ECG interpretation made incredibly easy (5th ed.). Philadelphia: Wolters Kluwer/Lippincott, Williams & Wilkins. e. Wolters Kluwer, & Lippincott, Williams & Wilkins. (2013, July 12) Cardiac Monitoring. Retrieved from http://procedures.lww.com/lnp/view.do?pId=656349&s=p&fromSearch=tr ue&searchQuery=cardiac+monitoring f. www.skillstat.com Special Requirements: Interns will need to borrow the “Basic ECG Interpretation made Incredibly Easy,” 5th ed. book. This book can be signed out in Staff Development, Monday through Friday 0700-1630. Please see the following Basic ECG Interpretation Schedule for details regarding class dates and times, expected learning to complete prior to class, class topics, and class locations. Evaluation a. Participants must pass the written ECG exam with 84% and all mandatory rhythms identified correctly. b. If participants score between 80-84% on the written ECG exam and have all mandatory rhythms correctly identified, they must meet and review their exam with their unit educator. The unit educator will verify that they have passed the exam after the meeting. c. If participants incorrectly identify a mandatory rhythm (VFib, VTach, AFib, Asystole and 3 degree AV block) and/or score less than 80%, they will need to do a retake exam, after they have practiced more. d. An education activity evaluation will be administered at each class date and at the end of the course. e. Learning outcomes will be measured via a brief online rhythm quiz at 3 months and 6 months after passing the written ECG exam. CLINICAL PRACTICUM 49 Basic ECG Interpretation Schedule Start Date: March 27th Schedule Date Time Day 1 4:00-7:00 p.m. Thursday March 27 Complete Prior to Class Read chapters 1-4 prior to the 1st class, filling in the Sinus Node Arrhythmia note sheets as you read chapter 4. Complete all of the chapter quizzes. Class Topics Location A & P, Basic Interpretation, Sinus Rhythms 14 Day 2 4:00–5:30 p.m. Read chapters 5 – 6, chapter quizzes, and complete homework Atrial and Junctional Rhythms D6 meeting room 1 4:00 – 5:30 p.m. Read chapters 7-8, chapter quizzes, and complete homework Ventricular Rhythms, and AV Blocks 14 4:00-6:00 p.m. Read chapters 9 and 10, chapter quizzes, and complete homework Pacemakers, Interventions and Review 14 Written Test 14 Thursday April 10 Day 3 Thursday April 17 Day 4 Thursday April 24 Day 5 4:00-5:00 p.m. Thursday May 1 Rhythm Review 1. Read “Brushing up on Interpretation Skills” 2. Read “Look Alike Challenge” 3. www.skillstat.com CLINICAL PRACTICUM 50 Case Study Presentation A. Objective: Presentation of an evolving case study appropriate for your peers. Choose a Critical Care topic. Follow the format of the educational planning table worksheet on the following page to create your outline. Choose and/or develop audiovisual aides for presentation of the case study. Review project with program coordinator prior to presentation. Deliver the presentation. Evaluate the effectiveness of the presentation. B. Instructions a. Each individual will select a topic of interest. b. Selected topic must be approved by program coordinator before you begin working on the project. c. Develop evolving case study that shows progression of patient’s disease process, with complications. d. Case study must be higher level learning geared toward nursing peers utilizing Evidence Based Practice. Case study may include experiences on your particular clinical unit. e. Presentation should be developed using the attached worksheet. f. Presentation should be scholarly, well researched utilizing current scholarly journal articles, appropriate websites, and AV/media/PowerPoint. g. Time frame for each presentation is approximately 1 hour. h. A copy of the presentation worksheet should be emailed to phresko@mhc.net by date on program calendar and must include references in APA format. C. The presentation must include the following information: a. Introduction: Section consists of introducing/presenting the patient. Required elements: Patient initials, date of birth, age, race and gender, current ht & wt, and date of admission. i. Chief complaint: (why the pt came into the hospital) and primary admitting diagnosis. ii. HPI: history of present illness (length of illness and signs and symptoms on admission). Provide a detailed course of illness and his or her present health state (are they better, worse or the same). b. Overview of patient: History, bio-psycho-social assessments, diagnostic tests (and why they were ordered), pharmacological interventions (including reason it was prescribed, therapeutic effects expected, and adverse effects to monitor), EKG interpretation, hemodynamics, nutritional measures, and genomic considerations. c. Pathophysiology: Review pathophysiology of the condition including etiologies, clinical manifestations, expected outcomes, current research, demographics, and relating this information to the assigned patient. d. Plan of Care i. Part 1: Generate and discuss nursing diagnosis in planning care for the patient. ii. Part 2: Priorities of care, plan, and evaluation of outcomes. e. Research-based Interventions: Evaluate the care this patient received related to your research of the condition. CLINICAL PRACTICUM 51 f. References: Cite all references used in the paper. The references must include at least one peer-reviewed journal article. The article must be less than 5 years old, and must be longer than 2 printed pages to count. Your other references can be textbooks and internet sites. The reference section must follow APA 6th edition format D. Evaluation of Presentation a. Please see rubric on the following page for evaluation criteria. CLINICAL PRACTICUM 52 EDUCATIONAL PLANNING TABLE LIVE EVENT Instructions: Type directly into blank cells of the tables. Educational Activity: Purpose of Activity: To improve the knowledge of nurses caring for patients with cardiac tamponade OBJECTIVES CONTENT List learner’s objectives in behavioral terms. (After completing this activity, the learner will be able to…) Provide an outline of the content for each objective. It must be more than a restatement of the objective. TIME FRAME State the time frame for each objective. PRESENTER List the faculty for each objective. TEACHING METHODS List the teaching methods, strategies, materials & resources for each objective. CLINICAL PRACTICUM 53 (Add more rows as needed by placing cursor outside of last row and clicking ‘Enter’ key.) Total minutes for this activity/session (including time spent evaluating the activity) = List the evidence-based reference(s) used for developing the content of this educational activity/session next to the appropriate category. Information from organization/website: (may be published or unpublished content. Examples – Centers for Disease Control, National Institutes of Health) Peer –reviewed journal/resource: (reference should be within past 5-7 years) Clinical guidelines: (published or online. Example www.guidelines.gov) Expert resource: (individual, organization, or educational institution - book, article, website) Textbook reference: Other: Running head: PRACTICUM PAPER 54 Case Study Presentation Rubric Organization Below Expectations Needs Improvement Meets Expectations Exceptional Comments Below Expectations Needs Improvement Meets Expectations Exceptional Comments The presentation was not clearly organized and was difficult to follow. There was no introduction or conclusion. The presentation was somewhat organized, but it may be a little difficult to follow. The presentation was missing an introduction or summary. The presentation was organized, but clear learning objectives and summary may be missing. An introduction provided sufficient background on topic and preview of major points. The presentation was well organized with clear objectives, introduction of topic and major points, and summary. Below Expectations Needs Improvement Meets Expectations Exceptional Presentation content lacks depth and breadth. Major points are unclear. Objectives are incomplete and not clearly supported by appropriate sources. Presentation content is somewhat developed. Major points are somewhat clear. Objectives may not be complete and may not be clearly supported by appropriate sources. Presentation content is developed. Major points are stated clearly. Objectives are mostly complete and supported by appropriate sources. Presentation content is thoughtfully developed and supported by appropriate and current sources (< 5 years unless a classical resource). Major points are stated clearly and supported by specific examples. Below Expectations Needs Improvement Meets Expectations Exceptional Presenter does not have grasp of information; presenter cannot answer questions about subject. Presenter is uncomfortable with information and is able to answer only rudimentary questions. Presenter is at ease with expected answers to all questions, but fails to elaborate. Presenter demonstrates knowledge by answering questions with explanation. Below Expectations Needs Improvement Meets Expectations Exceptional Presenter uses no audio/visual aids. Presenter use audiovisual aids to read out the material. Presenter's A/V relates to text and presentation. Presenter's A/V explains and reinforces topic and presentation. Below Expectations Needs Improvement Meets Expectations Exceptional Presenter reads all of report with no eye contact. Presenter occasionally uses eye contact, but still reads most of report. Presenter maintains eye contact most of the time but frequently returns to notes. Presenter maintains eye contact with audience, seldom returning to notes. Below Expectations Needs Improvement Meets Expectations Exceptional Presenter mumbles, incorrectly pronounces terms, and speaks too quietly for audience to hear. Presenter's voice is low. Presenter incorrectly pronounces terms. Audience members have difficulty hearing presentation. Presenter's voice is clear. Presenter pronounces most words correctly. Most audience members can hear presentation. Presenter uses a clear voice and correct, precise pronunciation of terms so that all audience members can hear presentation. Below Expectations Needs Improvement Meets Expectations Exceptional Enthusiasm Shows absolutely no interest in topic presented. Showed some negativity toward topic presented. Occasionally showed positive feelings about the topic. Demonstrated a strong positive feeling about topic during entire presentation. Below Expectations Needs Improvement Meets Expectations Exceptional Creativity No creativity/information appears to be taken be directly from a book. Lacks creativity. Shows some creativity. Creative. Content Subject Knowledge Audio/Visual Eye Contact Elocution Comments Comments Comments Comments Comments Comments Comments PRACTICUM PAPER 55 Reflection Journals A. Reflecting on one’s practice is considered an important part of the learning process. Thus, each week interns will make a journal entry of observations, insights, and discoveries encountered that week. Personal reflections should be related to clinical tasks, activities, and/or experiences. B. Examination of progress, identification of strengths and weaknesses, and goals for improvement should also be included in your journal entries. C. Journals should be approximately one page in length. Please date each entry by the week and place all entries into one ongoing document. D. Journals should be emailed to the program coordinator at the end of the intern’s clinical week. Intern Evaluation of Program Interns are provided the opportunity, and are strongly encouraged to participate in a program evaluation at the end of the internship. PRACTICUM PAPER 56 Appendix D Simulation Evaluation Munson Medical Center - Simulation Evaluation Form Title of Presentation: Critical Care Physical Assessment Simulation Date: 3/21/14 Location: Sim Lab Please complete the evaluation form below by placing an “X” in the box that best fits your evaluation of the educational activity. Completion of this form is required to successfully complete this conference and be awarded contact hours for the program. Purpose/Goal of this Simulation: At the end of this program, I was able to: 1. Perform a full systematic head-totoe physical assessment on a simulated patient 2. Identify major alterations in the assessment 3. Evaluate patient data 4. Communicate clearly to patient, family and healthcare team I clearly understood the purpose and objectives for the simulation. The scenario resembled a real-life situation. Did the scenario allow you to use your critical thinking and decision making skills? Did the scenario allow you to use your communication skills? The simulation provided a variety of ways in which to learn the material. The prep material provided to review before the simulation was valuable. The debriefing session was wellorganized. The facilitator, _Erin , demonstrated expertise in the content area. Feedback provided during the debriefing was constructive. The simulation activity reinforced my Strongly Agree Agree 4 4 4 4 4 3 4 4 4 4 4 4 4 4 Neutral Disagree Strongly Disagree PRACTICUM PAPER knowledge base. After participating in the simulation activity, do you feel more confident in a similar situation in the clinical environment? 57 4 What did you find most valuable participating in the simulation? Hands on training is always the best for me What would you like to see done differently in the next simulation? None How will you apply the information from the simulation activity into clinical practice? All of it I will apply PRACTICUM PAPER 58 Appendix E Practicum Evaluations Student name: Erin Kibbey________________________________________________________ Evaluated by: Erin Kibbey________________________________________________________ Goal/Objective Strongly Disagree Disagree Neutral Agree Strongly Agree Standard of Practice: Facilitation of Learning Shows enthusiasm for teaching, learning, and nursing X Demonstrates interest and respect for learners X Uses personal attributes such as caring, patience, integrity, flexibility, etc. to facilitate learning X Serves as a role model of professional nursing X Models critical and reflective thinking X Creates opportunities for learners to develop critical thinking skills X Uses information technologies skillfully to support the teaching-learning process X Practices X Comments PRACTICUM PAPER 59 communication that reflects awareness of self and others Ability to convey ideas in a variety of contexts X X Demonstrates recognition of multicultural, gender, and experiential influences on teaching and learning Implements a variety of teaching strategies X Teaching strategies are appropriate to learner, outcomes, context, content, etc. X X Engages in selfreflection and continued learning to improve teaching Standard of Practice: Use Assessment & Evaluation Strategies Uses literature to develop evidencebased assessment and evaluation practices X Uses a variety of strategies to assess and evaluate learning X Provides timely feedback to learners X Provides constructive feedback to learners X Uses evaluation data to enhance the X PRACTICUM PAPER 60 teaching-learning process Standard of Practice: Participate in Curriculum Design and Evaluation of Program Outcomes Ensures curriculum reflects current nursing and health care trends X Identifies program outcomes X Identifies learner needs X Writes appropriate learning objectives X Selects appropriate learning activities X Implements appropriate evaluation strategies for new curricula X Bases curriculum design on educational principles, theory, and research X Demonstrates overall knowledge of curriculum development X Comments: PRACTICUM PAPER 61 PRACTICUM PAPER 62 PRACTICUM PAPER 63 PRACTICUM PAPER 64 Appendix F Evaluations from Interns Evaluation 1 PRACTICUM PAPER 65 PRACTICUM PAPER Evaluation 2 66 PRACTICUM PAPER 67 PRACTICUM PAPER Evaluation 3 68 PRACTICUM PAPER 69 PRACTICUM PAPER Evaluation 4 70 PRACTICUM PAPER 71 PRACTICUM PAPER 72 Bibliography Alspach, J. G. (2000). The educational process in nursing staff development. Annapolis, MD: American Association of Critical Care Nurses. American Nurses Association and National Nursing Staff Development Organization [ANA & NNSDO]. (2010). Nursing professional development: Scope and standards of practice. Silver Spring, MD: Nursesbooks.org. Avillion, A., Brunt, B., & Ferrell, M. J. (2007). Nursing professional development: Nursing review and resource manual (1st ed.). Silver Spring, MD: American Nurses Credentialing Center. Baltimore, J. J. (2004). The hospital clinical preceptor: Essential preparation for success. Journal of Continuing Education in Nursing, 35(3), 133-140. Beyea, S. C., Slattery, M. J., & von Reyn, L. J. (2010). Outcomes of a simulation-based nurse residency program. Clinical Simulation in Nursing, 6(5). doi:10.1016/j.ecns.2010.01.005 Billings, D. M. (2012). Developing leaner-centered courses. In D. Billings & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 160-169). St. Louis, MO: Elsevier Saunders. Billings, D. M., & Halstead, J. A. (2012). Teaching in nursing: A guide for faculty (4th Ed.). Philadelphia: W.B. Saunders. Bjork, R., McDaniel, M., Pashler, H., & Rohrer, D. (2009). Learning styles: Concepts and evidence. Psychological Science in the Public Interest, 9(3), 105-119. Boland, D. (2012). Developing curriculum: Frameworks, outcomes, and competencies. In D. Billings & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 138159). St. Louis, MO: Elsevier Saunders. PRACTICUM PAPER 73 Bonnel, W. (2012). Clinical performance evaluation. In D. Billings & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 485-502). St. Louis, MO: Elsevier Saunders. Bourke, M. P. & Ihrke, B. A. (2012). The evaluation process: An overview. In D. Billings & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 422-440). St. Louis, MO: Elsevier Saunders. Bradshaw, M. (2011). Effective learning: What teachers need to know. In M. Bradshaw & A. Lowenstein (Eds.), Innovative teaching strategies in nursing and related health professions (5th ed.). (pp. 1-19). Sudbury, MA: Jones and Bartlett. Bradshaw, M. & Lowenstein, A. (2011). Innovative teaching strategies in nursing and related health professions (5th Ed.). Sudbury, MA: Jones & Bartlett Publishers. Bratt, M. (2009). Retaining the next generation of nurses: the Wisconsin Nurse Residency Program provides a continuum of support. Journal of Continuing Education in Nursing, 40(9), 416-425. doi:10.3928/00220124-20090824-05 Brunt, B. A. (2007). Competencies for staff educators: Tools to evaluate and enhance nursing professional development. Danvers, MA: HCPro, Inc. Buruss, N. & Popkess, A. (2012). The diverse learning needs of students. In D. Billings & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 15-33). St. Louis, MO: Elsevier Saunders. Center for Medical Simulation. (2013). Debriefing assessment for simulation in healthcare (DASH): Rater’s handbook. Retrieved from http://www.harvardmedsim.org/_media/DASH.handbook.2010.Final.Rev.2.pdf PRACTICUM PAPER 74 Clynes, M., & Raftery, S. (2008). Feedback: An essential element of student learning in clinical practice. Nurse Education in Practice, 8(6), 405-411. Deck, M. L. (2012). Nursing professional development: Stories, tips, and techniques. Journal for Nurses in Staff Development, 28(3), 143-149. Dillard, N. & Siktberg, L. (2012). Curriculum development: An overview. In D. M. Billings & J. A. Halstead (Eds.). Teaching in nursing a guide for faculty (4th ed.). (pp. 76-91). St. Louis, MO: Elsevier Saunders. Dyess, S. M., & Sherman, R. O. (2009). The first year of practice: New graduate nurses’ transition and learning needs. The Journal of Continuing Education in Nursing, 40(9), 403-410. http://dx.doi.org/10.3928/00220124-20090824-03 Flood, L., & Powers, M. (2012). Lessons learned from an accelerated post-master's nurse educator certificate program: Teaching the practicum course. Nursing Education Perspectives, 33(1), 40-44. doi:10.5480/1536-5026-33.1.40 Forneris, S., & Peden-McAlpine, C. (2007). Evaluation of a reflective learning intervention to improve critical thinking in novice nurses. Journal of Advanced Nursing, 57(4), 410-421. doi:http://0-dx.doi.org.libcat.ferris.edu/10.1111/j.1365-2648.2007.04120.x French, B. & Greenspan, M. (2011). The preceptored clinical experience. In M. Bradshaw & A. Lowenstein (Eds.), Innovative teaching strategies in nursing and related health professions (5th ed.). (pp. 437-457). Sudbury, MA: Jones and Bartlett Gaberson, K. & Oermann, M. (2010). Clinical teaching strategies in nursing (3rd ed.). NY: Springer Publishing Company. PRACTICUM PAPER 75 Goode, C. J., Lynn, M. R., Krsek, C., & Bednash, G. D. (2009). Nurse residency programs: An essential requirement for nursing. Nursing Economics, 27(3), 142-147, 159. Retrieved from https://www.nursingeconomics.net/ce/2011/article27142159.pdf Happell, B. (2009). A model of preceptorship in nursing: Reflecting the complex functions of the role. Nursing Education Perspectives, 30(6), 372-376. Hayes, J. (2011). Student evaluation of teaching. In M. Bradshaw & A. Lowenstein (Eds.), Innovative teaching strategies in nursing and related health professions (5th ed.). (pp. 563-574). Sudbury, MA: Jones & Bartlett Publishers. Henderson, A., & Eaton, E. (2013). Assisting nurses to facilitate student and new graduate learning in practice settings: What ’support’ do nurses at the bedside need? Nurse Education in Practice, 13(3), 197-201. Iwasiw, C, Goldenberg, D., & Andrusyszyn, M. (2005). Curriculum development in nursing education. Sudbury, MA: Jones and Bartlett Publishers. Jeffries, P. R. & Clochesy, J. M. (2012). Clinical simulations: An experiential, student-centered pedagogical approach. In D. Billings & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 352-368). St. Louis, MO: Elsevier Saunders. Jewell, A. (2013). Supporting the novice nurse to fly: A literature review. Nurse Education in Practice, 13(4), 323-327. doi:10.1016/j.nepr.2013.04.006 Kirkpatrick, J. M. & DeWitt, D. A. (2012). Strategies for assessing and evaluating learning outcomes. In D. Billings & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 441-463). St. Louis, MO: Elsevier Saunders. Knowles, M.S. (1980). The modern practice of adult learning. Chicago, IL: Follett. PRACTICUM PAPER 76 Kolb, D. (1984). Experiential learning: Experience as the source of learning and development. Englewood Cliffs, NJ: Prentice Hall. Retrieved from http://academic.regis.edu/ed205/kolb.pdf Leighton, K. & Johnson-Russell, J. (2011). Innovations in facilitating learning using simulation. In M. Bradshaw & A. Lowenstein (Eds.), Innovative teaching strategies in nursing and related health professions (5th ed.). (pp. 239-264). Sudbury, MA: Jones and Bartlett. Longo, A., & Tierney, C. (2012). Presentation skills for the nurse educator. Journal for Nurses in Staff Development, 28(1), 16-23. Lowenstein, A. J. (2011). Role play. In M. Bradshaw & A. Lowenstein (Eds.), Innovative teaching strategies in nursing and related health professions (5th ed.). (pp. 187-205). Sudbury, MA: Jones and Bartlett. McDonald, P. (2010). Transitioning from clinical practice to nursing faculty: lessons learned. Journal of Nursing Education, 49(3), 126-131. doi:10.3928/0148483420091022-02 McKinley, M. (2008). Walking on water and other lessons learned as a clinical educator. AACN Advanced Critical Care, 19(4), 388-395. Morris, L. L., Pfeifer, P. B., Catalano, R., Fortney, R., Hilton, E. L., McLaughlin, J., . . . Goldstein, L. (2007). Designing a comprehensive model for critical care orientation. Critical Care Nurse, 27(6), 37-60. Myrick, F., Yonge, O., & Billay, D. (2010). Preceptorship and practical wisdom: A process of engaging in authentic nursing practice. Nursing Education in Practice, 10(2), 8287. doi:10.1016/j.nepr.2009.03.018 PRACTICUM PAPER 77 National League for Nursing [NLN]. (2012). The scope of practice for academic nurse educators 2012 revision. NY: author. Penn, B., Wilson, L., & Rosseter, R. (2008). Transitioning from nursing practice to a teaching role. OJIN: The Online Journal of Issues in Nursing, 13(3), 1-14. Polit, D. F. & Beck, C. T. (2012). Nursing research: Generating and assessing evidence for nursing practice (9th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. Robinson, C. P. (2009). Teaching and clinical educator competency: Bringing two worlds together. International Journal of Nursing Education Scholarship, 6(1), 1-14. Rowles, C. J. (2012). Strategies to promote critical thinking and active learning. In D. Billings, & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 258-284). St. Louis, MO: Elsevier Saunders. Saunders, R. (2003). Constructing a lesson plan. Journal for Nurses in Staff Development, 19(2), 70-80. Sauter, M., Nightingale Gillespie, N., & Knepp, A. (2012). Educational program evaluation. In D. M. Billings & J. A. Halstead (Eds.). Teaching in nursing a guide for faculty (4th ed.). (pp. 503-549). St. Louis, MO: Elsevier Saunders. Scanlan, J. (2001). Learning clinical teaching: Is it magic? Nursing & Health Care Perspectives, 22(5), 240-246. Scheckel, M. (2012). Selecting learning experiences to achieve curriculum outcomes. In D. Billings & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 170187). St. Louis, MO: Elsevier Saunders. PRACTICUM PAPER 78 Schipper, L. (2011). The socialization process of newly graduated nurses into a clinical setting: role of the clinical nurse educator. Journal for Nurses in Staff Development, 27(5), 216219. doi:10.1097/NND.0b013e31822d68ba Schoening, A. M. (2013). From bedside to classroom: The nurse educator transition model. Nursing Educator Research, 34(3), 167-172. Shellenbarger, T. & Edwards, T. (2012). Nurse educator simulation: Preparing faculty for clinical nurse educator roles. Clinical Simulation in Nursing, 8(6), 249-255. doi:10.1016/j.ecns.2010.12.006 Stokes, L. G. & Kost, G. C. (2012). Teaching in the clinical setting. In D. Billings & J. Halstead (Eds.), Teaching in nursing: A guide for faculty (4th ed.). (pp. 311-334). St. Louis, MO: Elsevier Saunders. Tedesco-Schneck, M. (2013). Active learning as a path to critical thinking: Are competencies a roadblock? Nurse Education in Practice, 13(1), 58-62. Toth, J. (2008). The basic knowledge assessment tool, version eight (BKAT-8): For adult critical care nursing. Retrieved from http://www.bkat-toth.org/BKAT-8.html. Ullrich, S. & Haffer, A. (2009). Precepting in nursing: Developing an effective workforce. Sudbury, MA: Jones and Bartlett Publishers. Ulrich, B. (Ed.). (2012). Mastering precepting: A nurse’s handbook for success. Indianapolis, IN: Sigma Theta Tau International.