INFECTION control lecture ( 2)
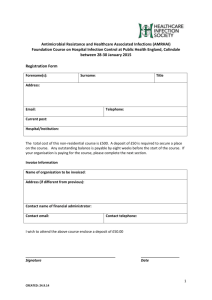
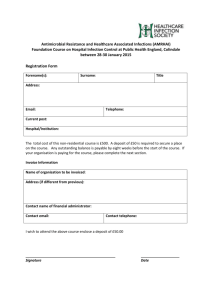
advertisement

2016 - 2017 Outlines • At the completion of this lecture the student will be able to identify the concept and related terms of: • Infection- Infection control- Infectious disease - Communicable disease • Occupational health strategies • Healthcare-associated infection • Healthcare-associated disease transmission • Healthcare workers • Nosocomial infection - Asymptomatic infection • Colonization- Fomite - Vehicle • Definition: infection defined as: The invasion and multiplication of microorganisms such as bacteria, viruses, and parasites that are not normally present within the body. • N.B: An infection may cause no symptoms and be subclinical, or it may cause symptoms and be clinically apparent. • N.B: Infection may be local or generalized and spread throughout the body. Definition: Infection control defined as is practices help to protect clients and healthcare providers from disease by reducing and /or eliminating sources of infection. • Defined as is Measures that aim to ensure the protection of those who might be vulnerable to acquiring an infection both in hospital due to health problems and in general community. The basic principle of infection prevention and control is hygiene. 1. Infectious disease: any infection caused by microbes or parasites. 2. Communicable disease: infection transmitted from persons or animals to other persons. Patient may acquire infection before admission to the hospital = Community acquired infection. Patient may get infected inside the hospital = Nosocomial infection. It includes infections infections that appear more than 48 hours after admission, those acquired in the hospital but appear after discharge also occupational infections among staff. Absence of symptoms or signs of illness in the infected person. • Colonization: Proliferation of microorganisms within body sites without detectable host immune response, cellular damage, or clinical expression (i.e. without symptoms or signs of disease). The host may become a source of potential transmission. • Fomite: Nonliving object that transmits infectious agents from a reservoir to a host. • Fomites: such as food, water or blood are called vehicles. • Examples: include tissues, doorknobs, telephones, bed linens, toilet seats, and clothing. Any healthcare equipment, supplies, or surfaces that have become contaminated with pathogens can become a fomite. • Vehicle: Objects such as food, water, biological products (e.g. blood) and that may indirectly transmit an infectious agent from a reservoir to a host. • All fomites are vehicles, but not all vehicles are fomites. • Outbreaks of disease are linked to common vehicles, such as bacteremia resulting from use of intravenous fluids contaminated with a gram-negative organism, or gastroenteritis resulting from food contaminated with E. coli. Any person who has contact with patients, body fluids, or supplies used for patient care as part of their job. This includes physicians, nurses, occupational therapists, physical therapists, as well as administrative, environmental hygiene, and laboratory staff in medical facilities. All healthcare workers should be trained in basic infection control regardless of whether they deliver direct care to patients. The ways in which a pathogen is spread from an infected person to another person. Common modes of transmission include: 1. Carrying: pathogens on unwashed hands 2. Contact: with surfaces or medical instruments that are not cleaned between patients. 3. Droplets: released into the environment when an infected person coughs. 4. Airborne: Most agents have multiple modes of transmission. Introduction • Healthcare-associated infections (HAIs) are among the most common adverse events in hospitals, and the morbidity and mortality associated with them are significant. • The Centers for Disease Control and Prevention (CDC) estimate that 1 out of every 20 hospitalized patients develop a healthcare-associated infection each year, corresponding to almost 2 million infections and nearly 100,000 deaths in U.S. hospitals alone ( Yokoe, 2008/ CDC, 2011). The total burden of HAIs is likely to be even higher, since the CDC estimates don't include nursing homes, home health care, rehabilitation centers, dialysis centers, outpatient acute care. Patients in nursing homes and in home care are at risk for developing HAIs, particularly if they have invasive medical devices such as urinary catheters or central venous catheters in place. In the United States, 1.6 to 3.6 million infections occur each year in longterm care facilities—almost as many HAIs as in acute care hospitals (SHEA/APIC, 2008). Site of Infection Total Cases Percent of Hospital HAIs Urinary tract 561,667 32 Bloodstream 248,678 14 Pneumonia 250,202 15 Surgical site 290,485 22 Other sites 386,090 17 1,737,125 100 Total • Refers to A set of activities intended to assess, prevent, and control infections and communicable diseases in healthcare workers. • About 3% to 15% of nursing home residents acquire infection, and infection accounts for up to 30% of transfers of nursing home residents to hospitals. • Healthcare-associated infections not only cause suffering and death, but the medical costs for treating them, prevention of HAIs has become a national healthcare priority. • Prevention of HAIs is the responsibility of all healthcare personnel. Many states and most medical professional organizations have defined standards of professional behavior and responsibility as they pertain to infection control. • Healthcare workers—from physicians to dental hygienists— may be sanctioned, including loss of license, for not following effective infection control practices. Four Ways to Prevent HAI 1. Maintain cleanliness of the hospital. 2. Personal attention to hand washing before and after every contact with a patient or object. 3. Use personal protective equipment whenever indicated. 4. Use and dispose of sharps safely. • In 2001, the Occupational Safety and Health Organization (OSHA), the federal organization regulating workplace safety, issued the Blood borne Pathogens Standard aimed at preventing transmission of HIV and Hepatitis B and C viruses in the workplace. • The scientific basis for such infection control guidelines and standards are derived from the work of experts at organizations such as the Centers for Disease Control and Prevention (CDC), the Association for the Prevention and Infection Control (APIC), and the Society for Healthcare Epidemiology of America (SHEA). Purposes of IPC in health care To prevent the occurrence of HAI in patients, health-care workers, visitors and other. Persons associated with health-care facilities. (Infection Program Control) These infections may be: − endemic, associated with the use of devices or procedures during health care; − epidemic, originating within the population of the health-care facility; To prepare health-care facilities for the early detection and management of epidemics and to organize a prompt and effective response; To contribute to a coordinated response to control community-acquired infectious diseases, endemic or epidemic. To contribute to preventing the emergence of antimicrobial resistance and/or dissemination of resistant strains of microorganisms; and To minimize the environmental impact of these infections or their management. Questions 1. Define ( infection, infection control) 2. List common modes of transmission? 3. Enumerate purposes of IPC in health care? 4. What are Four Ways to Prevent HAI?