Andy_GroupB_StaticAsthmaResource
advertisement
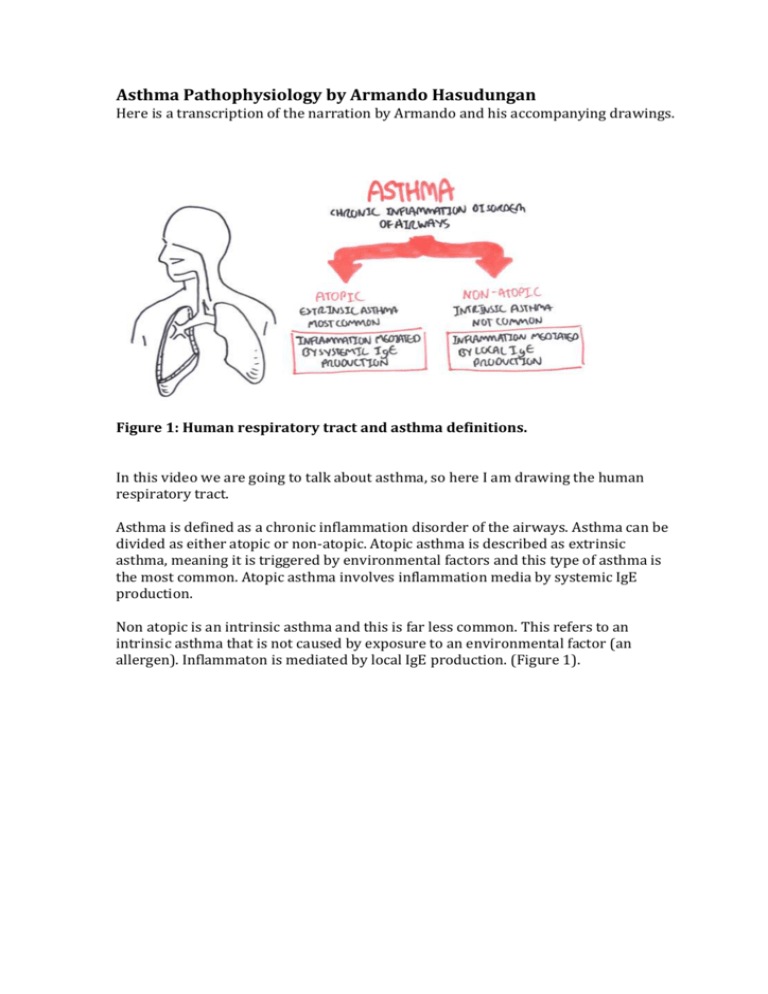
Asthma Pathophysiology by Armando Hasudungan Here is a transcription of the narration by Armando and his accompanying drawings. Figure 1: Human respiratory tract and asthma definitions. In this video we are going to talk about asthma, so here I am drawing the human respiratory tract. Asthma is defined as a chronic inflammation disorder of the airways. Asthma can be divided as either atopic or non-atopic. Atopic asthma is described as extrinsic asthma, meaning it is triggered by environmental factors and this type of asthma is the most common. Atopic asthma involves inflammation media by systemic IgE production. Non atopic is an intrinsic asthma and this is far less common. This refers to an intrinsic asthma that is not caused by exposure to an environmental factor (an allergen). Inflammaton is mediated by local IgE production. (Figure 1). Figure 2: Cross-section and histological representation of the normal lung. So let’s look at a cross-section through a normal lung. Here we have the mucus layer, we have pseudostratified endothelial cells, we have the lamina propria and the smooth muscles surrounding all of this. If we were to look at an asthmatic bronchiole, the lumen (the inside) would be seen to be much narrower. But before we focus on the asthmatic bronchiole, what do the normal histological layers look like? We have a mucus layer and the pseudostratified columnar epithelial cells. Below this we have a basement membrane, and within the epithelial layer we can find goblet cells that are responsible for secreting mucus into the lumen. Below the epithelium we have the lamina propria which contains the main cells including macrophages and mast cells. Mast cells are responsible for secreting histamine. Below the LP we have the smooth muscle. (Figure 2). Figure 3: Asthmatic bronchiole. If we were to compare the normal bronchiole with the asthmatic bronchiole we would see many differences. Firstly we would see an increase in in mucus production, so there is an increase in goblet cells. Also there is an increase in eosinophils in the mucus and tissue. Here we have the pseudostratified columnar epithelial cells and below it the basement membrane thickens. Within the lamina propria we see an increase in mast cell numbers so we get an increase in histamine release. We also get an increase in neutrophils and T helper cells. We see smooth muscle hypertrophy which means an increase in smooth muscle size, and this is due to an increase in constriction. (Figure 3). Figure 4A (left) – three main characteristics of asthma, and 4B (right) – main symptoms. Because of all these changes there are three characteristics of asthma. These are airflow obstruction, bronchiole hyper-responsiveness because of histamine release, and inflammation due to the increased release of neutrophils and other immune cells to the area. Symptoms of asthma include shortness of breath therefore, wheeze, chest tightness and dry irritating cough. (Figures 4A and 4B). Figure 5: Pathophysiology of asthma. So now that we have identified some changes that occur in an asthmatic bronchiole, let us look at the pathophysiology. Let’s look at some players in the pathophysiology. The main one is IgE antibodies. This are important because they bind to receptors on mast cells forming a mast cell-IgE complex. The complex will recognise antigens and start releasing histamine. Other players include eosinophils, dendritic cells and T helper cells. There are 2 types of T helper cells, Th1 and Th2. In the lungs Th1 are usually found, but in asthma there is an imbalance, and Th2 cells that are not normally found in the lungs are up-regulated in asthma. So we have more Th2 cells in the lungs of asthmatics. Th1 usually promotes inflammation by increasing cell-mediated immunity, but Th2 promotes inflammation by increasing the humoral immunity, promoting antibody production, so I hope you can see how this correlates. (Figure 5). Figure 6. Pathogenesis of atopic asthma. By putting these cells together we can do a diagram focusing on the pathogenesis of atopic asthma. We have the pseudostratified columnar epithelial cells and goblet cells secreting mucus into the lumen. Below the pseudostratified columnar cells we have the lamina propria where we have the mast cells and dendritic cells and macrophages. Let’s say the asthmatic inhales an allergen and this allergen will trigger a reaction. The allergen will be engulfed by dendritic cells and then activate the dendritic cells. The columnar epithelial cells recognise this and secrete a substance called thymicstromal lymphocyte (TSL). TSL will condition activated dendritic cells to produce chemokines to attract specifically Th2 cells; the activated dendritic cell itself activates the T helper cells to differentiate to Th2 and secrete chemokines to attract Th2 to the lungs and bronchioles. The activated T helper 2 cells do several things. Firstly the Th2 role is to promote humoral immunity so will stimulate plasma cells thru IL13 and Il4 and this will promote IgE production by the plasma cells. IgE will help bind to mast cells to create the IgE-mast cell complex. Th2 itself via IL9 will stimulate or promote mast cell activity. Another important activity of Th2 cells is to stimulate eosinophil production from the bone marrow via IL5, so you get more eosinophils, and there is a chemotactic response occurring to attract the eosinophils to the lungs, so we have increased eosinophil amounts in the lungs. The inhaled allergen will bind to IgE-mast cell complex causing it to release histamine, prostaglandins and leukotrienes. All of this will stimulate smooth muscle in the airways to constrict, so we get bronchiole constriction. There is also a release of stem cell factors to maintain mast cells in the area. So if there is IgE being produced, essentially memory, whenever the same type of allergen is inhaled again we get the whole process reoccurring. (Figure 6). That is the end of the learning material relating to the pathogenesis of asthma. NOTE Asthma Pathophysiology by Armando Hasudungan For students studying biomedical science at UWE it is noted that this video was randomly selected from YouTube for the purposes of this research, and that UWE would not necessarily endorse the quality of it. It is published under a Standard YouTube License and we are reproducing it here solely for research purposes.