The Neuroscience of Orthopedic Dysfunction
advertisement

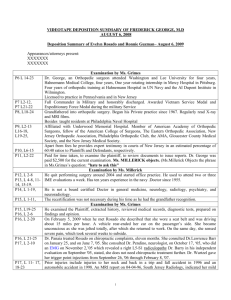
THE NEUROSCIENCE OF ORTHOPEDICS COMPLEX PROBLEMS WITH SIMPLE SOLUTIONS RODERICK HENDERSON, PT, SCD, OCS, MA, CSCS WHAT YOU’LL LEARN • ORTHOPEDIC DIAGNOSES ARE OFTEN VERY STRAIGHTFORWARD • THE PATIENT’S RESPONSE TO A DIAGNOSIS MAY VARY ACCORDING TO: • SENSORY PHYSIOLOGY • CENTRAL PROCESSING (COGNITIVE / AFFECTIVE) • AUTONOMIC DRIVE THE NERVOUS SYSTEM • DRIVES THE RESPONSE • ADAPTS TO NEW INFORMATION WHERE WE’RE GOING • HOW DID WE PUT THE NEURO IN ORTHO? • HOW DO WE TREAT COMPLEX PROBLEMS WITH STRAIGHTFORWARD SOLUTIONS? ORTHOPEDIC PT STEREOTYPE • FORMULAIC • PROTOCOL-DRIVEN • BORING… WHAT WE REALLY SEE • TREMENDOUS VARIABILITY • CHALLENGING PROBLEMS • EXCITING OPPORTUNITIES CHALLENGE #1 • ORTHOPEDIC PTS TRAINED AS CLINICAL BIOMECHANISTS • BUT – LINES BETWEEN BIOMECHANICS AND PATHOLOGY ARE BLURRY! CHALLENGE #2 • WE DON’T LIKE CHASING PAIN • BUT - PAIN IS OFTEN THE PATIENT’S CHIEF COMPLAINT! Symptoms TRADITIONAL INJURY MODEL Pathology Halderman S. Presidential Address, North American Spine Society: Failure of the pathology model to predict back pain. 1990; Spine 15:718-724. Symptoms IDEAL RECOVERY Pathology Halderman S. Presidential Address, North American Spine Society: Failure of the pathology model to predict back pain. 1990; Spine 15:718-724. EXPECTATIONS • PATHOLOGY AND SYMPTOMS SHOULD IMPROVE WITH EFFECTIVE TREATMENTS • IDEALLY SHOULD ALSO SEE A REVERSAL OF ANY STRUCTURAL ABNORMALITY Symptoms PERSISTENT PAIN Pathology Halderman S. Presidential Address, North American Spine Society: Failure of the pathology model to predict back pain. 1990; Spine 15:718-724. Symptoms THE AGING BODY Pathology Halderman S. Presidential Address, North American Spine Society: Failure of the pathology model to predict back pain. 1990; Spine 15:718-724. A GROWING TREND • PATHOLOGICAL SIGNS PRESENT WITHOUT SYMPTOMS (FALSE POSITIVES) • SEEN WITH INCREASING REGULARITY • LUMBAR SPINE • SHOULDER • FOOT AND ANKLE CONSEQUENCES • DISABILITY, FEAR, FRUSTRATION • HIGHER COSTS, OVERUTILIZATION, DEPENDENCE UPON PASSIVE INTERVENTION STILL BORED?? • THOUSANDS OF NEW ARTICLES PUBLISHED • EVOLVING CLINICAL GUIDELINES • MORE WAYS TO HELP OUR PATIENTS ANSWERS • FULLY UNDERSTANDING RESPONSE TO INJURY • SEE WHERE THINGS GO WRONG • TREAT THE PATIENT USING A BIOPSYCHOSOCIAL MODEL EVOLUTION OF PAIN THEORY • SPECIFICITY • GATE • PAIN MATRIX SPECIFICITY PRINCIPLES • TISSUES HAVE “PAIN” RECEPTORS • PAIN SIGNALS TRANSMITTED TO THE BRAIN KEY ASSUMPTIONS • PAIN IS AN INPUT TO THE CNS • PATHOLOGY = PAIN • PINEAL GLAND IS THE PAIN CENTER IMPLICATIONS • PATHOLOGY = PAIN • ERADICATE PATHOLOGY = ERADICATE PAIN UPSIDE OF SPECIFICITY • UPGRADE FROM THE MYSTICAL MODEL! • ACKNOWLEDGED THE NERVOUS SYSTEM LIMITATIONS OF SPECIFICITY • PAIN CAN BE PRESENT WITHOUT TISSUE DAMAGE • TISSUE DAMAGE CAN BE PRESENT WITHOUT PAIN KEY NOTE: NOCICEPTION IS NEITHER NECESSARY NOR SUFFICIENT FOR THE PRODUCTION OF PAIN OTHER PROBLEMS • PHANTOM LIMB PAIN • CHRONIC REGIONAL PAIN SYNDROME BODY PARTS ARE REPRESENTED IN THE CNS THROUGH MAPS THE SECOND EVOLUTION GATE THEORY (1965) • DESCENDING CONTROL FROM BRAIN AND SPINAL CORD • FORMED THE BASIS FOR TENS • MOST PTS ARE AWARE OF THIS MODEL WHAT CHANGED? • CHALLENGES THE CONCEPT OF “PAIN GENERATOR” • NOXIOUS STIMULI MODULATED BY DORSAL HORN AND CNS • OUTPUT IS THE “PAIN EXPERIENCE” LIMITATIONS OF THE GATE • WIDESPREAD OR CHRONIC PAIN SYNDROMES? • PAIN FOLLOWING SPINAL CORD INJURY • STILL NO ACCOUNTING FOR CRPS! Melzack R. From the Gate to the Neuromatrix. Pain Supplement. 1999; 6:S121-S126. ENTER THE MATRIX • ALSO KNOWN AS THE “PAIN MATRIX” OR “NEUROMATRIX” • FRAMEWORK FOR MULTI-SYSTEM RESPONSE TO INJURY • THE MOST CURRENT MODEL OF INJURY RESPONSE TO DATE Melzack R. Pain and the Neuromatrix in the Brain. Journal of Dental Education. 2001;65(12):1378-1382 GETTING ORGANIZED Inputs Outputs Processing Melzack R. Pain and the Neuromatrix in the Brain. Journal of Dental Education. 2001;65(12):1378-1382 WHAT IS AN INPUT? • BRAIN CONSTANTLY SAMPLING INFORMATION • INTERNAL INFORMATION FROM BODILY TISSUES • EXTERNAL INFORMATION FROM THE ENVIRONMENT INPUTS • SENSORY • COGNITIVE • AFFECTIVE SENSORY INPUTS Mechanical Chemical Thermal • Movement • Touch • Inflammation • Neurotransmitters • Warmth produced by metabolic activity Butler D, Moseley P and DL. Explain Pain. 1st ed. Orthopedic Physical Therapy Products; 2003. RELEVANCE OF SENSORY INPUTS • WE ARE HIGHLY SELECTIVE • PRIORITY OF INPUTS IS VARIABLE • ALTERED BY ATTENTION NOT A ONE-WAY STREET Butler D, Moseley P and DL. Explain Pain. 1st ed. Orthopedic Physical Therapy Products; 2003. CLINICAL RELEVANCE • COMMUNICATION BETWEEN TISSUE AND CNS IS BIDIRECTIONAL • LONG-STANDING MSK PROBLEMS SHOW SIGNS OF NEUROGENIC INFLAMMATION • IMPLICATIONS FOR NEURODYNAMICS THE VALUE OF GOOD INPUT • STIMULUS-DETECTION SYSTEM OF THE BODY • TISSUE DAMAGE WILL INCREASE SIGNAL INTENSITY FROM THAT REGION • PURPOSE IS TO GET YOUR ATTENTION! • SENSORY FIBERS ARE NOT PURELY SENSORY Butler D, Moseley P and DL. Explain Pain. 1st ed. Orthopedic Physical Therapy Products; 2003. COGNITIVE INPUTS • KNOWLEDGE • EXPERIENCE • EXPECTATION COGNITIVE INPUTS • WHAT DOES THE PATIENT BELIEVE IS HAPPENING? • HAVE THEY DEALT WITH SIMILAR PROBLEMS? COGNITIVE INPUTS • HOW DID THEY HANDLE IT? • WHAT DO THEY THINK IS GOING TO HAPPEN? RELEVANCE OF COGNITIVE INPUTS • BELIEF INFLUENCE OUTCOMES • EXPERIENCE SHAPES COPING • EXPECTATION INFLUENCES RESPONSE AFFECTIVE INPUTS • BASELINE IMMUNE / ENDOCRINE FUNCTION • AUTONOMIC NERVOUS SYSTEM FUNCTION • LIMBIC SYSTEM – EMOTIONAL REGULATION RELEVANCE OF AFFECTIVE INPUT • INTERACTION BETWEEN NERVOUS AND IMMUNE • AUTONOMIC FUNCTION INFLUENCES PROCESSING THERAPEUTIC INPUTS • PATIENT EDUCATION • MANUAL THERAPY • ACTIVE MOVEMENT IMPLICATIONS • MULTIPLE AVENUES TO PAIN RELIEF • OR EXACERBATION • MAYBE WHY “EVERYTHING” SEEMS TO WORK? Melzack R. Pain and the Neuromatrix in the Brain. Journal of Dental Education. 2001;65(12):1378-1382 DYNAMIC PROCESSING • INPUTS CONSTANTLY EVALUATED • INJURY • MOVEMENT • TOUCH • OUTPUT IS PRODUCED AND EVALUATED • THINK OF STEPPING ON A STICKER BURR! • CHANGES MAY OCCUR THROUGHOUT THE CNS DYNAMIC PROCESSING • DISTRIBUTED PROCESSING WITH NO “PAIN CENTER” • CORRESPONDS WITH CHARACTERISTIC PAIN BEHAVIORS Butler D, Moseley P and DL. Explain Pain. 1st ed. Orthopedic Physical Therapy Products; 2003. CENTRAL INFLUENCES • COGNITION AND CONTEXT • EMOTIONS AND MOOD • ATTENTION AND VIGILANCE DORSAL HORN Butler D, Moseley P and DL. Explain Pain. 1st ed. Orthopedic Physical Therapy Products; 2003. IMPLICATIONS OF DORSAL HORN • SPINAL CORD ACTS AS AN AMPLIFIER OR INHIBITOR OF SOMATOSENSORY INPUT • PERSISTENT NOCICEPTION CREATES AN EXPANSION OF RECEPTIVE FIELDS • PAIN WITH A-BETA STIMULATION • INCREASING PATTERNS OF REFERRAL WITH CHRONICITY MANUAL CARE AND THE DORSAL HORN • ALTERATIONS IN MOTOR NEURON POOL RECRUITMENT • MODIFIED C-FIBER ACTIVITY FOLLOWING MANIPULATION • RECEPTIVE FIELDS ALTERED BY OPIOID AND B-ENDORPHIN RESPONSE CEREBRAL PLASTICITY • PAIN AND INJURY ALTER CEREBRAL PHYSIOLOGY AND ARCHITECTURE • NEURONS THAT “FIRE TOGETHER, WIRE TOGETHER” • NEURAL PLASTICITY UNDERAPPRECIATED IN ORTHOPEDIC PT! May A. Chronic pain may change the structure of the brain. Pain. 2008;137:7-15. EVIDENCE FOR CENTRAL CEREBRAL CHANGES • REDUCTION IN GREY MATTER SHOWN IN YELLOW COMPARED TO HEALTHY CONTROLS • STILL UNCLEAR IF A CAUSE OR CONSEQUENCE May A. Chronic pain may change the structure of the brain. Pain. 2008; 137:7-15. CEREBRAL CHANGES – ACL • CASE CONTROL STUDY OF 17 ACL-DEFICIENT KNEES AND 18 HEALTHY CONTROLS • BRAIN ACTIVITY MEASURED USING FMRI • CONCLUSIONS • ACL INJURY CAUSED FUNCTIONAL REORGANIZATION OF CNS • SHOULD BE CONSIDERED A NEUROPHYSIOLOGIC DYSFUNCTION, NOT A SIMPLE MUSCULOSKELETAL INJURY • FINDINGS COULD LEAD TO NEW STANDARDS OF REHABILITATION AND MOTOR CONTROL APPLICATION Kaprieli E, Athanasopoulous S, et al. Anterior Cruciate Ligament injury causes brain plasticity: A functional MRI study. Am J Sports Med. 2009;37:2419-2426. CORTICAL CHANGES - LBP • CLBP INDUCES SIGNIFICANT CORTICAL CHANGES • MAY EXPLAIN PERSISTENT SYMPTOMS IN THE ABSENCE OF STRONG MECHANICAL FINDINGS Flor H, Braun C, Elbert T, Birbaumer N. Extensive reorganization of primary somatosensory cortex in chronic back pain patients. Neurosci. Lett. 1997;224(1):5-8. CORTICAL CHANGES - CTS Napadow V, Kettner N, Ryan A, et al. Somatosensory cortical plasticity in carpal tunnel syndrome--a cross-sectional fMRI evaluation. Neuroimage. 2006;31(2):520-530. CORTICAL CHANGES - CTS • ALTERED AFFERENT PROCESSING PRODUCED CORTICAL CHANGES IN SYMPTOMATIC SUBJECTS • TAKE HOME – INJURY CHANGES THE BRAIN! Napadow V, Kettner N, Ryan A, et al. Somatosensory cortical plasticity in carpal tunnel syndrome--a cross-sectional fMRI evaluation. Neuroimage. 2006;31(2):520-530. Melzack R. Pain and the Neuromatrix in the Brain. Journal of Dental Education. 2001;65(12):1378-1382 OUTPUTS • INPUTS AND PROCESSING PRODUCE OUTPUTS • PRIMARY REASON FOR OUTPUTS IS TO MAINTAIN HOMEOSTASIS • OUTPUTS GET US OUT OF TROUBLE! IMMUNE / ENDOCRINE RESPONSE • THE CHEMICAL “MUSCLES” OF THE CNS • INTEGRAL TO RESPONSE OR OUTPUT • STRONG INFLUENCES ON AROUSAL, ATTENTION, AND FEAR IMMUNE / ENDOCRINE RESPONSE • BOTH SYSTEMS RESPOND TO STRESS AND TISSUE INJURY • INFLUENCE NEURAL RESPONSE • STRONG INFLUENCE ON TISSUE HEALING • TWO PRIMARY RESPONSE AXES • HYPOTHALAMUS-PITUITARY-ADRENAL AXIS • SYMPATHOADRENAL AXIS HPA AXIS • PAIN ELICITS A CORTISOL RESPONSE • CHRONIC PAIN RESULTS IN ALTERATIONS OF CORTISOL VARIABILITY • ASSOCIATED WITH HIGH FEAR, DISABILITY, AND CATASTROPHIZING Johannson et al. Pain, disability and coping reflected in the diurnal cortisol variability in patients scheduled for lumbar disc surgery. Eur J Pain. 2008;12:633-640 SA AXIS • SNS CAN CONTRIBUTE TO SENSITIVITY OF A-DELTA AND C AFFERENTS • PERSISTENT PAIN CAN LEAD TO ADRENORECEPTOR UPREGULATION AT DRG Chapman CR, Tuckett RP, Song CW. Pain and Stress in a Systems Perspective: Reciprocal Neural, Endocrine, and Immune Interactions. Journal of Pain. 2008;9(2): 122-145 IMMUNE RESPONSE: CYTOKINES • CHEMICAL MESSENGERS PRODUCED DURING TISSUE INJURY AND STRESS Pro-Inflammatory Anti-Inflammatory TNF – Alpha IL-4 IL-1 IL-10 IL-6 IL-13 Powerful contributors to inflammation and pain! Chapman CR, Tuckett RP, Song CW. Pain and Stress in a Systems Perspective: Reciprocal Neural, Endocrine, and Immune Interactions. Journal of Pain. 2008;9(2): 122-145 CYTOKINES IN DIAGNOSIS • DIAGNOSTIC UTILITY OF CYTOKINE BIOMARKERS IN ACUTE KNEE PAIN • PROSPECTIVE COHORT OF 70 KNEES • 32 PATIENTS • 15 CONTROLS • SEVENTEEN INFLAMMATORY CYTOKINES EVALUATED • STUDY EXAMINED: • PREOPERATIVE MRI • CYTOKINE PROFILE • OPERATIVE FINDINGS Cuellar JM, Scuderi GJ, Cuellar VG, et al. Diagnostic Utility of Cytokine Biomarkers in the Evaluation of Acute Knee Pain. Journal of Bone and Joint Surgery. 2009;91:2313-20. RESULTS • SIGNIFICANTLY HIGHER CYTOKINE CONCENTRATION IN SYMPTOMATIC KNEES • PRESENCE OF FOUR INFLAMMATORY CYTOKINES PERFORMED AS WELL AS MRI IN PREDICTING INTRAOPERATIVE FINDINGS Cuellar JM, Scuderi GJ, Cuellar VG, et al. Diagnostic Utility of Cytokine Biomarkers in the Evaluation of Acute Knee Pain. Journal of Bone and Joint Surgery. 2009;91:2313-20. CONCLUSIONS “INTRA ARTICULAR CONCENTRATIONS OF FOUR INFLAMMATORY CYTOKINES….WERE MARKEDLY LOWER IN ASYMPTOMATIC NORMAL KNEES AND IN ASYMPTOMATIC KNEES WITH MENISCAL TEARS.” Cuellar JM, Scuderi GJ, Cuellar VG, et al. Diagnostic Utility of Cytokine Biomarkers in the Evaluation of Acute Knee Pain. Journal of Bone and Joint Surgery. 2009;91:2313-20. MORE ON CYTOKINES • CYTOKINES PLAY A ROLE IN OA PATHOGENESIS • NOT PURELY A MECHANICAL PHENOMENON Orita S, Koshi T, Mitsuka T, et al. Associations between proinflammatory cytokines in the synovial fluid and radiographic grading and pain-related scores in 47 consecutive patients with osteoarthritis of the knee. BMC Musculoskelet Disord. 2011;12:144. CYTOKINES IN OA • Inflammatory cytokines produced by synovial tissue • Injection of inhibiting agents slowed progression in animal models FERNANDES JC, MARTEL-PELLETIER J, PELLETIER J-P. THE ROLE OF CYTOKINES IN OSTEOARTHRITIS PATHOPHYSIOLOGY. BIORHEOLOGY. 2002;39(1-2):237-246. CYTOKINES AND MUSCLE TIISSUE • Potential anti-inflammatory role of muscle tissue in cartilage degeneration • Another avenue for the benefits of physical activity? CAIRNS DM, UCHIMURA T, KWON H, ET AL. MUSCLE CELLS ENHANCE RESISTANCE TO PRO-INFLAMMATORY CYTOKINE-INDUCED CARTILAGE DESTRUCTION. BIOCHEM. BIOPHYS. RES. COMMUN. 2010;392(1):22-28. OUTPUTS: WHAT WE SEE Pain Behavior Stress Response Movement Alterations Severity Fear / Anxiety Postural Irritability Helpless / Hopeless Nature Autonomic changes Dynamic THE MATRIX UPGRADE • MULTIPLE INPUTS • DYNAMIC PROCESSING • PAIN IS THE OUTPUT WHY IS THIS A BIG DEAL? • CONSIDER CLINICAL PHENOMENON LIKE ANTALGIC GAITS AND POSTURES • ARE THEY DEFECTS OR DEFENSE? • WOULD IT CHANGE OUR MANAGEMENT? IMPLICATIONS • EFFECTS OF INJURY DISTRIBUTED ACROSS SEVERAL SYSTEMS • CHANGES IN PAIN REFLECTS A CHANGES TO ONE OR MORE OF THESE SYSTEMS Tracey I, Mantyh PW. The Cerebral Signature for Pain and its modulation. J Neuron. 2007;55:377-391 IMPLICATIONS • NERVOUS SYSTEM ACUTELY ADAPTS TO INJURY AND TREATMENT • REHABILITATION INFLUENCES CEREBRAL AND DORSAL HORN PLASTICITY Boudreau SA, Farino D, Falla D. The role of neuroplasticity in designing rehabilitation approaches for musculoskeletal pain disorders. Manual Therapy (2010), doi:10:1016/j.math.2010.05.008 Traditional Model Contemporary Model EXERCISE – IT’S WHAT WE DO • ALMOST SYNONYMOUS WITH OUR PROFESSION • FOUNDATIONAL COMPONENT OF OUR PRACTICE • WE SHOULD HAVE THIS DOWN RIGHT? TRADITIONAL FOCUS Physical • Stronger muscles • Improved flexibility • More endurance EMERGING EVIDENCE Psychological • Reduced fear • Improved efficacy • Stress tolerance CONTEMPORARY MODEL Physical • Stronger muscles • Improved flexibility • More endurance Psychological • Reduced fear • Improved efficacy • Stress tolerant OUR CHALLENGES • GROWING EVIDENCE-BASE OF EXERCISE SCIENCE • NOT A LOT OF ENTRY-LEVEL TRAINING • LIMITED POST-GRADUATE TRAINING NO EASY ANSWERS • WE KNOW MOVEMENT IS BENEFICIAL • NO CLEAR CONSENSUS EXIST REGARDING • TYPE • DOSE • SUB-GROUPING MAY GUIDE DECISIONS BUT STILL NOT CLEAR Kent P, Mjøsund HL, Petersen DHD. Does targeting manual therapy and/or exercise improve patient outcomes in nonspecific low back pain? A systematic review. BMC Med. 2010;8:22. WHERE’S THE EVIDENCE? MOST OF IT’S HERE… EXERCISE AND LOW BACK PAIN • HIGHEST FORMS OF EVIDENCE SUGGEST MINIMAL BENEFIT • LOWER FORMS OF EVIDENCE SUGGEST MODERATE BENEFIT van Middelkoop M, Rubinstein S, Kuijpers T, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. European Spine Journal. 2011;20(1):19–39. Choi BK, Verbeek JH, Tam WW-S, Jiang JY. Exercises for prevention of recurrences of low-back pain. In: The Cochrane Collaboration, Choi BK, eds. Cochrane Database of Systematic Reviews. POSSIBLE EXPLANATIONS? “THE PROBLEM WITH THE EVIDENCE PYRAMID IS THAT IT'S SORTED BY RIGOR, NOT BY RELEVANCE." -PHIL SIZER PT, PHD, FAAOMPT POSSIBLE EXPLANATIONS If you let systematic reviews dictate your practice this is what you'll do for low back pain: "stay active, it's not serious, no you don't need MRI, get regular exercise, avoid surgery, have a nice day. NEXT!“ -Jason Silvernail, DPT, DSc, FAAOMPT CURRENT CLINICAL GUIDELINES • EXERCISE RECOMMENDED FOLLOWING SELF-CARE • ALSO RECOMMENDED • YOGA • COGNITIVE-BEHAVIORAL THERAPY • SPINAL MANIPULATION Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478–491. IASP GUIDELINES • EXERCISE IS BENEFICIAL FOR MAJORITY OF MSK CONDITIONS • NO OPTIMAL TYPE OR DOSE OF ACTIVITY IS ESTABLISHED IASP Global Year Against Musculoskeletal Pain http://www.iasp-pain.org IASP GUIDELINES • LOWER INTENSITY PROGRAMS RECOMMENDED BASED ON TOLERANCE • HIGHER INTENSITY MAY BE INDICATED AS TOLERANCE IMPROVES • ACUTE TOLERANCE MAY NOT PREDICT LONG-TERM RESPONSE IASP Global Year Against Musculoskeletal Pain http://www.iasp-pain.org IASP GUIDELINES • SUPERVISED PROGRAMS PREFERABLE • COMPLIANCE IMPROVED BY COMBINING • EXERCISE • MOTIVATIONAL PROGRAMS IASP Global Year Against Musculoskeletal Pain http://www.iasp-pain.org POSSIBLE TAKE HOME • EXERCISE A BENEFICIAL COMPONENT OF MUSCULOSKELETAL MANAGEMENT • EDUCATION • MANUAL CARE • NO MAGIC BULLET “SYSTEMS” OR “EXERCISES” IN SHORT… • MOVEMENT CERTAINLY HELPS • SPECIFICS ARE VERY FUZZY • USE CLINICAL JUDGMENT • BIOMECHANICS+ • NEUROSCIENCE+ GREAT…SO NOW WHAT? • MOVEMENT-BASED PROGRAMS THAT • OPTIMIZE STRESSES ON RECOVERING TISSUE • MINIMIZE NOCICEPTIVE DRIVE • FACILITATE CENTRAL INHIBITION OF PAIN • LOT’S OF WAYS TO ACCOMPLISH THIS! OUR APPROACH • GRADED ACTIVITY / EXPOSURE • AEROBIC EXERCISE • AWARENESS THROUGH MOVEMENT (ATM) LESSONS • RESISTANCE EXERCISE GRADED ACTIVITY • IDENTIFY DIRECTIONAL PREFERENCES • MINIMIZES NOCICEPTIVE DRIVE • STRONG EMPHASIS ON LOW-THRESHOLD INPUTS • BENEFICIAL FOR PATIENT AND THERAPIST • DIAGNOSTIC • THERAPEUTIC • HIGHLY BENEFICIAL FOR NOCICEPTIVE AND PERIPHERAL NEUROGENIC PAIN STATES EXAMPLE • LUMBAR AND CERVICAL ROTATION • PASSIVE AND AA SHOULDER ELEVATION • ACTIVE NEURODYNAMIC “SLIDERS” EMPHASIS • PAIN-FREE MOTION • WORKING ALONG THE “EDGES” • DISCOURAGE UNHELPFUL BELIEFS • “NO PAIN. NO GAIN” • “AVOID PAIN AT ALL COSTS” BENEFITS • PATIENT ABLE TO EVALUATE THEIR OWN PROGRESSION • THERAPIST CAN GUIDE THE PATIENT WITH • EDUCATION • REASSURANCE • GOAL SETTING GRADED PROGRESSION WHAT IF “EVERYTHING” HURTS? • NOT UNCOMMON IN PATIENTS WITH CENTRAL SENSITIZATION • CLINICAL EXAMS MAY NOT EFFECTIVELY GUIDE INTERVENTION • BUT WE STILL DO THEM! • CONSIDER ACTIVITIES THAT WILL ENHANCE CENTRAL INHIBITION WHAT IF EVERYTHING HURTS? • CONSIDER GRADED MOTOR IMAGERY • EVIDENCE IS ENCOURAGING BUT STILL DEVELOPING Moseley GL, Zalucki N, Birklein F, et al. Thinking about movement hurts: the effect of motor imagery on pain and swelling in people with chronic arm pain. Arthritis Rheum. 2008;59(5):623–631. Moseley GL. Graded motor imagery for pathologic pain: a randomized controlled trial. Neurology. 2006;67(12):2129–2134. MOTOR IMAGERY Butler D, Moseley P and DL. Explain Pain. 1st ed. Orthopedic Physical Therapy Products; 2003. MOTOR IMAGERY NeuroOrthopedic Institute: www.noigroup.com MENTAL VS PHYSICAL PRACTICE Lederman E. Neuromuscular Rehabilitation in Manual and Physical Therapies: Principles to Practice, 1e. 1 Har/DVD. Churchill Livingstone; 2010. VIRTUAL MOVEMENT • IMAGINING MOVEMENTS • ALTER CONTEXT • PLAY WITH BALANCE • CHANGE VISUAL OR AUDITORY INPUTS Butler D, Moseley P and DL. Explain Pain. 1st ed. Orthopedic Physical Therapy Products; 2003. VIRTUAL MOVEMENT • CHANGE THE MOVEMENT ENVIRONMENT • MOVE UNDER DIFFERENT EMOTIONAL STATES • EXERCISE WHILE DISTRACTED • PLAN CHALLENGING ACTIVITY Butler D, Moseley P and DL. Explain Pain. 1st ed. Orthopedic Physical Therapy Products; 2003. PACING AND GRADED EXPOSURE Lederman, E. Neuromuscular Rehabilitation in Manual and Physical Therapies: Principles to Practice, 1e. 1 Har/DVD. Churchill Livingstone; 2010. PACING AND GRADED EXPOSURE Butler D, Moseley P and DL. Explain Pain. 1st ed. Orthopedic Physical Therapy Products; 2003. Butler D, Moseley P and DL. Explain Pain. 1st ed. Orthopedic Physical Therapy Products; 2003. IS THIS REALLY ANY DIFFERENT? TRADITIONAL APPROACH • STRENGTHEN WEAK MUSCLES • STRETCH TIGHT MUSCLES • TRAIN “THE CORE” • DISCOURAGE HARMFUL MOVEMENT IS THIS REALLY ANY DIFFERENT? CONTEMPORARY APPROACH • EMPHASIS ON MOVEMENT – NOT MUSCLE • MOTOR CONTROL VERSUS “CORE TRAINING” • POSTURE IS CONTEXT DEPENDENT • ENCOURAGE GRADED EXPOSURE TO MOVEMENT GET SYMPATHETIC • MORE SPECIFICALLY – PARASYMPATHETIC • STRONG SYMPATHETIC DRIVE LINKED TO HIGHER PAIN LEVELS • MOVEMENT AND MANUAL CARE INFLUENCES IT! Kregel KC, Seals DR, Callister R. Sympathetic Nervous System Activity During Skin Cooling in Humans: Relationship to Stimulus Intensity and Pain Sensation. J Physiol. 1992;454(1):359–371. Perry J, Green A, Singh S, Watson P. A preliminary investigation into the magnitude of effect of lumbar extension exercises and a segmental rotatory manipulation on sympathetic nervous system activity. Manual Therapy. 2011;16(2):190–195. GETTING PARA-SYMPATHETIC • EXPLICITLY ENCOURAGE REGULAR AEROBIC EXERCISE • PROGRESSION TOWARD ACSM GUIDELINES Glass JM, Lyden AK, Petzke F, et al. The effect of brief exercise cessation on pain, fatigue, and mood symptom development in healthy, fit individuals. Journal of Psychosomatic Research. 2004;57(4):391–398. Koltyn K.F. Exercise-Induced Hypoalgesia and Intensity of Exercise. Sports Medicine. 2002;32(8):477–487. Mueller PJ. Exercise training and sympathetic nervous system activity: evidence for physical activity dependent neural plasticity. Clin. Exp. Pharmacol. Physiol. 2007;34(4):377–384. ACSM GUIDELINES • AT LEAST 150 MINUTE OF MODERATE INTENSITY EXERCISE EACH WEEK • BETWEEN 3.0 AND 5.9 METS • MORE VIGOROUS EXERCISE 20-60 MINUTES THREE TIMES A WEEK ALSO ACCEPTABLE • OVER 6 METS Garber CE, Blissmer B, Deschenes MR, et al. Quantity and Quality of Exercise for Developing and Maintaining Cardiorespiratory, Musculoskeletal, and Neuromotor Fitness in Apparently Healthy Adults. Medicine & Science in Sports & Exercise. 2011;43(7):1334–1359. OTHER WAYS Satyapriya M, Nagendra HR, Nagarathna R, Padmalatha V. Effect of integrated yoga on stress and heart rate variability in pregnant women. Int J Gynaecol Obstet. 2009;104(3):218–222. Telles S, Reddy SK, Nagendra HR. Oxygen consumption and respiration following two yoga relaxation techniques. Appl Psychophysiol Biofeedback. 2000;25(4):221– 227. Veerabhadrappa SG, Baljoshi VS, Khanapure S, et al. Effect of yogic bellows on cardiovascular autonomic reactivity. J Cardiovasc Dis Res. 2011;2(4):223–227. SUMMARY OF RECOMMENDATIONS • GRADED PROGRESSION OF PHYSICAL ACTIVITY • PACING AND GRADED EXPOSURE • DAILY AEROBIC EXERCISE REMEMBER THANK YOU