2015-6-19_-Dural-Venous-Thromb_Apenbrinck
advertisement

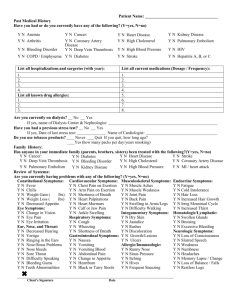
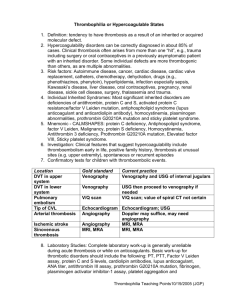
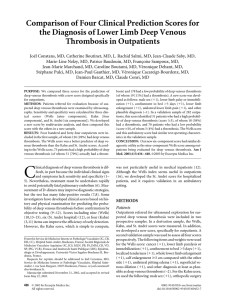
Grand Rounds Eddie Apenbrinck M.D. University of Louisville School of Medicine Department of Ophthalmology & Visual Sciences 5/1/2015 Subjective CC: blurry vision and headache HPI:47 year old white male admitted to the VA hospital for syncope after climbing a flight of stairs 2 days prior to admission. Consulted for blurry vision associated with headache. POH: refractive error (lost glasses) PMHx: seizures (not on medication), bipolar disorder (not on medication), GERD left upper deep venous thrombosis (5 years ago) and pulmonary embolus (10 years ago) ROS: denies any flashes/floaters/ocular pain. +intermittent dizziness Meds: Cetirizine 10mg daily Omeprazole 20mg daily, Allergies: NKDA Social:+Cocaine use Denies cigarettes and alcohol use Imaging: On admission CT head: High attenuation in the right transverse dural venous sinus as well as the posterior descending portion of the superior sagittal sinus. “These may be normal intravascular blood in a patient with high hematocrit.” MRI/MRV: pending CT head Superior Superior Sagittal Sinus Right Transverse Sinus Inferior Exam OD OS VA(cc, near): 20/30-2 20/40-2 Pinhole 20/20 20/20 Pupils: 3 3 2 2 no RAPD IOP: EOM: 16 15 full full Exam OD Anterior Segment L/L: C/S: Cornea: AC: I/L: Vitreous: OS WNL OU WNL OU WNL OU No cell or flare OU WNL OU WNL OU DFE Optic Nerve: MVP: 3+ disc edema WNL OU Optic Nerve iPhone Photo OD OS MRV showing dural venous thrombosis Normal Normal Dural venous thrombosis involving superior sagittal sinus, right transverse sinus and right sigmoid sinus. No flow seen in the right internal jugular vein Normal MRV MRI T2 Axial: Absence of Flow Void Absence of flow void in superior sagittal sinus Labs CBC: 13.9 5.9 334 40.7 PT: 12.0 INR: 1.0 PTT: 25.0 (11.8-14 seconds) (21.7-36.5 seconds) Labs: Hypercoagulation Workup Prothrombin Gene Mutation: not detected Factor V Leiden Gene Mutation: not detected Antithrombin III: Protein C and Protein S: WNL Cardiolipin IgG and IgM: WNL WNL Assessment and Plan Assessment: 47 year old white male with bilateral disc edema secondary to Dural Venous Thrombosis involving the right transverse sinus and the superior sagittal sinus Plan: Anticoagulate with heparin Discuss medication compliance and need to stop cocaine use Patient was transferred to UL for Neurosurgery evaluation Hematology consult placed once patient at UL UL Hospital Course Ophthalmology: Re-consulted for bilateral papilledema, planned for outpatient followup at the VA for HVF testing and refraction Neurosurgery: Initially planned for angiography with attempt to do a thrombectomy but deemed unrealistic as patient had complete occlusion of the right internal jugular UL Hospital Course Hematology Reviewed hypercoagulability work-up and were unable to determine cause of patient’s clotting disorder Patient initially placed on heparin drip during hospitalization then placed on Lovenox and bridged to Coumadin, planned for life-long anticoagulation Follow-up arranged with VA hematology/oncology 2 months Hematology Follow-up No additional thrombotic events Patient to remain on chronic anticoagulation due to high risk of another thrombotic event despite negative tests. Plan to complete hypercoagulable work up: flow cytometry for PNH and lupus anticoagulant Cerebral Venous Thrombosis Cerebral venous thrombosis (CVT) is a pathologic condition encompassing thrombosis of the cortical and deep cerebral veins and the dural sinuses. First described in the early 19th century in a 45year-old man harboring a systemic malignancy who had thrombosis of the superior sagittal sinus demonstrated at autopsy. Cerebral Venous Thrombosis Incidence Rare disease and the incidence is unknown as most of the estimates are derived from autopsy studies Autopsy studies have reported the incidence to be as low as 0.03% and as high as 9%. Cerebral Venous Thrombosis Despite a long list of possible causes of CVT, some investigators estimate that as many as 40% of cases are idiopathic CVT affects all age groups and both sexes, but with a strong preponderance in women between 20 and 40 years of age Clinical Findings Highly variable clinical manifestations Increased intracranial pressure is thought to be the underlying cause of these symptoms. Headache is the most common and often the earliest symptoms seen in ~80% of patients Papilledema ~50% Mental status changes ~25% Nausea, Vomiting Diagnosis/Treatment Diagnosis: MRI/MRV gold standard CTA/CTV Treatment Treatment of underlying condition Anticoagulation Thrombolytics Thrombectomy Endovascular stenting Literature review to determine the link between cocaine and arterial or venous thrombosis Review of Medline, CINAHL, Embase, Psycinfo, and Cochrane databases 2458 abstracts reviewed with 15 full-texts papers meeting inclusion criteria Conclusions: Cocaine is a pro-thrombotic agent that activates the thrombotic pathways There is an association between cocaine and myocardial infarction particularly among young adults Cocaine may casually associated with cerebrovascular accident though studies lacked sufficient power to determine a statistically significant effect There is a gap in the evidence pertaining to the issue of cocaine and venous thrombosis Case report of a 30 year patient who presented with occipital headache and vomiting without a history of trauma but admitted to extensive cocaine abuse Examination revealed bilateral papilloedema and imaging confirmed a superior sagittal and transverse sinus thrombosis. The patient was diagnosed with cocaine-induced central venous thrombosis Managed with routine anticoagulation and a repeat MRV showed re-cannulation of the vessels. References Nat MJ Wright, Matthew Martin, Tom Goff, et al. Cocaine and thrombosis: a narrative systematic review of clinical and in-vivo studies. Substance Abuse Treatment, Prevention, and Policy 2007, 2:27 Hunt MG, Lee AG, Kardon RH, et al. Improvement in papilledema and visual loss after endovascular stent placement in dural sinus thrombosis. Neuroophthalmology 2001 Sep;26(2):85-92. Burns H, Rich P, An Unpleaseant hit from Cocaine: A Case of Cocaine-induced Cerebral Venous Sinus ThrombosisJ Neurol Neurosurg Psychiatry 2012;83:A1 Carhuapoma JR, Mitsias P, Levine SR. Cerebral venous thrombosis and anticardiolipin antibodies. Stroke. 1997;28:2363. Erez N, Babuna C, Uner A. Low incidence of thromboembolic disease. An evaluation of obstetric and gynecologic patients in Istanbul. Obstet Gynecol. 1966;27:833. Towbin A. The syndrome of latent cerebral venous thrombosis: its frequency and relation to age and congestive heart failure. Stroke. 1973;4:419. Ribes M. Des rescherches faites sur la phlébite. Revue Médicale Française et Etrangère et Journal de Clinique de l’Hôtel-Dieu et de la Charité de Paris. 1825;3. Bousser MG, Chiras J, Bories J, et al. Cerebral venous thrombosis—a review of 38 cases. Stroke. 1985;16:199.