Biochemistry of Cardiac Muscle and Lung
advertisement

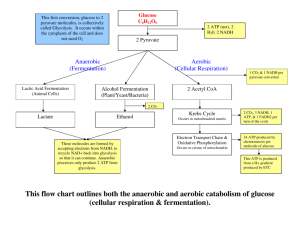
Biochemistry of Cardiac Muscle and Lung Jana Novotná Department of Biochemistry 2nd Faculty of Medicine Charles University Specifity of Cardiac Metabolism Myocardial function depends on a fine equilibrium between the work the heart has to perform to meet the requirements of the body & energy that it is able to synthesize and transfer in the form of energy-rich phosphate bonds to sustain excitation-contraction coupling. To support high rates of cardiac power, metabolism is design to generate large amount of ATP. Specifity of Cardiac Metabolism Heart muscle is highly oxidative tissue. Mitochondrial respiration produces more than 90% of energy. Mitochondria occupy ~30% of cardiomyocyte space. >95% of ATP formation comes from oxidative phosphorylation in mitochondria. ~ 60-70% of ATP hydrolysis is used for muscle contraction, ~30 - 40% for the sarcoplasmic reticulum (SR) Ca2+-ATPase and other ion pumps. Regulation of Metabolic Pathways in the Heart Glycolysis + b-oxidation acetyl-CoA citric acid cycle NADH, FADH2 electron transport chain ATP W.C. Stanley et all. Physiol. Rev. 85, 2005 Carbohydrate Metabolism • • • Glycolytic substrate is derived from exogenous glucose and glycogen stores. Glycogen pool in the heart is relatively small (~30 mmol/g wet wt compared with ~150 mmol/g wet wt in skeletal muscles). Glucose transport into cardiomyocyte is regulated by transmembrane glucose gradient and the content of glucose transporter in the sarcolema – GLUT-4 (lesser extent GLUT-1). Carbohydrate Metabolism Insulin stimulation, increased work demand, or ischemia increase glucose transport and rate of glucose uptake. Glycolytic pathway converts glucose 6-phosphate and NAD+ to pyruvate and NADH+H+, generate 2 ATP for each glucose molecule. Pyruvate and NADH+H+ are shuttled to the mitochondrial matrix to generate CO2 and NAD+ - complete aerobic oxidative glycolysis. Carbohydrate Metabolism Fosfofructokinase-1 (PFK-1) – key regulatory enzyme in glycolytic pathway – catalyzes the first irreversible step. PFK-1 utilized ATP fructose 1,6bisphosphate, is activated by ADP, AMP and Pi and inhibited by ATP and fall in pH. PFK-1 can be also stimulated by fructose -2,6-bisphosphate (formed from fructose 6-phosphate by PFK2). W.C. Stanley et all. Physiol. Rev. 85, 2005 Carbohydrate Metabolism Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) converts glyceraldehyde-3-phosphate to 1,3-diphosphoglycerate → production of NADH. GAPDH is major regulatory step → accumulation of NADH within cytoplasm inhibits, and NAD+ activates the GAPDH activity Severe ischemia in heart → lactate and NADPH accumulation → cessation of oxidative metabolism and lactate production. Under anaerobic condition pyruvate is converted to lactic acid – nonoxidative glycolysis. Lactate is released in the blood stream through specific monocarboxylate transporter (MCT). Critical role of transporter in maintaining the intracellular pH (removes also the protons produced by glycolysis). Carbohydrate Metabolism In the mitochondria pytuvate is: dexarboxylated and oxidized into acetyl CoA by pyruvate dehydrogenase (PDH) or carboxylated into oxalacetate by pyruvate carboxylase. The control of PDH activity is an essential part of overall control of glucose metabolism. PDH – mitochondrial multicomplex, activity is controlled by work, substrate and hormones. Fatty Acid Metabolism FFA enter the cardiomyocyte by: passive diffusion protein-mediated transport across sarcolema – fatty acid translocase (FAT) or plasma membrane fatty acid binding protein (FABPpm). Acyl-CoA synthase (FACS) activates nonesterified FA by esterification to fatty acylCoA. W.C. Stanley et all. Physiol. Rev. 85, 2005 Fatty Acid Metabolism Long chain fatty acyl-CoA can be: esterified to triglyceride (glycerolphosphate acyltransferase) converted to long chain fatty acylcarnitine by carnitine palmitoyltransferase-I (CPT-I) between inner and outer mitochondria membranes. or W.C. Stanley et all. Physiol. Rev. 85, 2005 Fatty Acid Metabolism Carnitine acyltranslocase (CAT) transports long-chain acylcarnitine across the inner membrane in exchange for free carnitine. Carnitine palmitoyltransferase II (CPT-II) regenerates long chain acylCoA . W.C. Stanley et all. Physiol. Rev. 85, 2005 Fatty Acid Metabolism CPT-1 can be strongly inhibited by malonyl CoA (on the cytosolic side of the enzyme). Two isoforms of CPT-1: liver CPT-1a and heart CPT-1b CPT-1b is 30-fold more sensitive to malonyl-CoA inhibition. W.C. Stanley et all. Physiol. Rev. 85, 2005 Fatty Acid Metabolism Malonyl-CoA - key physiological regulator of FA oxidation in heart (in malonyl-CoA FA uptake and oxidation). formed from the carboxylation of acetyl-CoA (acetyl-CoA carboxylase – ACC) from extramitochondrial acetyl-CoA (derived from citrate via ATP-citratelyase reaction) rapid rate of turnover in the heart. ACC activity is inhibited by fosforylation of AMPKacceleration of FA oxidation. W.C. Stanley et all. Physiol. Rev. 85, 2005 Fatty Acid Metabolism FA undergo b-oxidation generating NADH+H+ and FADH2. Acetyl-CoA formed in b-oxidation generate more NADH+H+ in citric acid cycle (CAC). W.C. Stanley et all. Physiol. Rev. 85, 2005 Interregulation of fatty acid and carbohydrate oxidation The primary physiological regulator of flux through PDH and the rate of glucose oxidation in the heart is fatty acid oxidation. PDH activity is inhibited by high rate of FA oxidation via an increase in mitochondrial acetyl-CoA/free CoA and NADH/NAD+ which activates PDH kinase. Interregulation of fatty acid and carbohydrate oxidation Inhibition of FA oxidation increases glucose and lactate uptake and oxidation by: 1. decreasing citrate levels and inhibition of PFK 2. lowering acetyl CoA and/or NADH levels in the mitochondria matrix. Keton Body Metabolism During starvation or poorly controlled diabetes the heart extracts and oxidized ketone bodies (bhydroxybutyrate and acetoacetat). Low insuline and high fatty acids ketone bodies. Ketone bodies become a major substrate for myocardium. Ketone bodies inhibit PDH (inhibition of glucose oxidation) and fatty acid b-oxidation. Some Aspects of Myocardial Biochemistry of Heart Failure Heart failure reduces the capacity to transduce the energy from foodstuff into ATP. In the advanced stage of HF down regulation in FA oxidation; increased glycolysis and glucose oxidation; reduced respiratory chain activity. Cardiac Muscle and Ischemia Coronary artery occlusion → ischemia → significant change in cell structure, chemistry and function loss of contractile function arrhythmias cell death The decrease of the ATP / ADP, the accumulation of AMP, inorganic phosphate, metabolic products are removed (lactate). The rapid decline in creatine phosphate - creatine kinase + ADP → phosphorylation of ADP → ATP (only short-term mechanism to compensate for reduced ATP production in mitochondria) Cardiac Muscle and Ischemia Even mild ischemia reduces the concentration of ATP and creatinephosphate, increases the level of inorganic phosphate → activation of glycolysis (glucose needed from the bloodstream into the heart cells) → increase in the concentration of pyruvate → conversion by LDH to lactate. Prolonged ischemia - the accumulation of substrates (lactate, NADH+ and H+) → inhibition of glycolysis at the level of phosphofructokinase and glyceraldehyde-3-dehydrogenase. Cardiac Markers Troponin (T or I) - the most sensitive and specific test for myocardial damage released during MI from the cytosolic pool of the myocytes. Approximate peak release in 12 hours in MI Cardiac Markers Creatin kinase (CK) is relatively specific when skeletal muscle damage is not present. CK has two subunits – CK-M (muscle), CK-B (brain) and mitochondrial CKmi CK-MM (CK-1) - skeletal muscle 95%, heart 42%, smooth muscle 2 – 3% CK-MB (CK2) – skeletal muscle 3%, heart 28%, smooth muscle 1 – 5% CK-BB (CK-3) – skeletal muscle 1%, heart 1%, smooth muscle 87% Approximate peak release in 10 to 24 hours. Cardiac Markers Lactate dehydrogenase (10 – 24 hours) is not as specific as troponin. LDH is tetramer with 2 subunits – H – heart, M - muscle Isoenzymes LDH1 (4 H) – heart and red blood cells, LDH2 (3HM) – heart and reticuloendothelial system, LDH3 (2H2M) - lungs, LDH4 (H3M) – kidneys, placenta, pancreas, LDH5 (4M) – liver and striated muscles In normoxia – LDH2 is higher than LDH1 A high LDH1 level to LDH2 suggest MI Myoglobin (2 hours) has low specificity for MI – it is high when muscle tissue is damaged but it lacks specificity. Cardiac Markers Aspartate transaminase (AST) was the first used it is also one of the liver function test Glycogen phosphorylase isoenzyme BB (GPBB) One of 3 isoforms of glycogen phosphorylase exists in heart and brain tissue Because of the blood-brain barrier GP-BB can be seen as heart muscle specific. One of the "new cardiac markers" which are discussed to improve early diagnosis in acute coronary syndrome. Elevated 1–3 hours after process of ischemia. References Reviews: W.C. Stanley, F.A. Recchia, G.D. Lopaschuk: Myocardial substrate metabolism in the normal and failing heart. Physiol. Rev. 85:1093-1129, 2005 CH. Depré, M.H. Rider, L. Hue: Mechanism of control of heart glycolysis. Eur. J. Biochem. 258:277290, 1998 R. Ventura-Clapier, A. Garnier, V. Veksler: Energy metabolism in heart failure. J. Physiol. 555:1-13, 2003 Biochemistry of Lungs Biochemistry of Lungs • Produce: surfactant collagen + elastin mucus (mucopolysacharides + IgA) • Activate: angiotensin (ACE in luminal surface of the • Inactivate: ROS pulmonary endothelium) kinins (hydrolysis of peptide bonds in bradykinin) serotonin (from mast cells, from blood - MAO) acetylcholin detoxication of foreign components (cytochrom P450 in microsomes)lbiochemistry of lungs Pulmonary Surfactant • • • • • • surface-active lipoprotein complex formed by type II alveolar cells complex of proteins and lipids with a hydrophilic and a hydrophobic region the hydrophilic head groups facing towards the water and the hydrophobic tails facing towards the air reduces surface tension surface tension is an effect within the surface layer of a liquid that causes that layer to behave as an elastic sheet increases pulmonary complience (the ability of the lungs to stretch in a change in volume relative to an applied change in pressure). Properties of Surfactant • Once secreted to alveolar space, surfactant absorbs rapidly to the air-liquid interface (a newborn baby´s first breath). • Once in the interface, surfactant films reduces surface tension when compressed during expiration (lungs don´t collapse). • Surfactant proteins recognize and opsonize bacterial, fungal, viral surface oligosaccharides. Lyra, P.P.R.; de Albuquerque Diniz, E.M. Clinics 62: 181, 2007 Structure of Alveolus http://herkules.oulu.fi/isbn9514270584/html/c273.html Phospholipides Nonpolar tail Polar head Proteins Synthesis - epitelial cells SP-A and SP-D large glykosylated proteins ( SP-D has 355 AA) water-soluble members of calcium-dependent carbohydrate-binding collectin family SP-B and SP-C small peptides (35 AA), highly hydrophobic confer surface tension-lowering properties important for spreading of the surfactant Proteins SP-A is responsible for: • • • • • • formation of tubular myelin regulation of phospholipid insertion into the monolayer modulation of uptake and secretion of phospholipids by type II cells activation of alveolar macrophages binding and clearance of bacteria and viruses chemotactic stimulation of alveolar macrophages SP-D plays important role in pathogen defence SP-B and SP-C: • • enhance the biophysical properties of surfactant assist in rapid insertion of phospholipids into the monolayer and molecular ordering of the monolayer Surfactant Metabolism DPPC is synthesized in rER. Transferred to the lamellar bodies together with SP-B and SP-C (the lamellar bodies are the storage and secreting granules surrounded by a limiting membrane that fuses with the plasma membrane). Surfactant secretion can be stimulated by the stretching of the type II epithelial cells, by the action of beta-agonists, and purinergic agonists, such as ATP Lyra,P.P. R.; de Albuquerque Diniz, E.M. Clinics 62: 181, 2007 • • Lamellar bodies and tubular myelin Lamellar bodies have an acidic internal environment and have high calcium content. Control of Surfactant Release Distortion of cells Hyperventilation - deep breath, yawn acetylcholine (large doses) beta-agonists purinoreceptors corticoids (maturity after pre-term birth) thyroxin Synthesis glycerol glucose from circulation (glykogen) polar heads cholin, inositol from circulation fatty acids endogenous from lactate exogenous Synthesis of DPPC de novo Glucose NAD+ glycerol-3-phosphate Glycogen NADH DHAP palmitoyl-CoA CoASH Choline palmitoyl-G3P palmitoyl-CoA ATP CoASH ADP dipalmitoylphosphatidic acid phosphocholine H2O CTP Pi PPi dipalmitoylglycerol CDP-choline CMP DPPC Function of Surfactant • surfactant reduces tension of the air/liquid interface to near zero surfactant aids the oxygen to perfuse from the atmosphere into the pulmonary capillaries • • • • During the breathing cycle : DPPC is insert into the monolayer, lowers the surface tension of air/liquid interface PG is effective in spreading surfactant Proteins accelerate the process to lower tension Reactive Oxygen Species ROS . O - + e + H+ 2 . HO2 . O2- + 2H+ + e H2O2 + e .OH + e + H+ . HO hydroperoxid radical 2 H+ . +O 2 hydrogen peroxide H2 O2 . OH- + OH H2 O superoxid radical hydroxyl radical Reactive Oxygen Species ROS O2 + 2H2 2H2O Cu,Zn-SOD O2 e . O2 - e 2H H2O2 Fe3+ + Cu . e H . OH e H MPO OH H2O Px H 2O HClO peroxidation of lipids (phospholipids) aldehydes (malonaldehyde) O3, NO, NOx, SiO2, smoking, infection, radiation, hypoxia/reoxygenation, ischemia/reperfusion Reactive Nitrogen Species - RNS L-arginine NOS L-citrulline + NO HbO2 O2 O2- nitrate NO3- + metHb nitrite NO2- peroxinitrite HOCl + MPO ONOOH oxidation nitration nitrosation thiyl radical S-nitrosothiol nitrotyrosine Antioxidant Defence Free radical scavenging enzymes Components of antioxidant protection Enzymatic Antioxidative Defence tetravalent reduction (ROS generated during oxidative phosphorylation) acceleration of monovalent reduction: SOD cytosolic (Cu-Zn) 5 mitochondrial (Mn) 1 extracellular (Cu-Zn) catalase (heme-containing) glutathione system GPx (Se) 2 cytosolic, membrane-ass., extracellular 2GSH NADPH Rib-6-P 2H2O GPx H2O2 GR reductase GSSG NADP+ Glucose Nonenzymatic Scavengers vitamin E - lipid peroxyl radicals vitamin C - O2-, .OH , Fe3+ Fe2+ β-carotene (O2-), uric acid (O2-), glucose (OH), bilirubin (LOO.) Fe sekvestration – lactoferrin and transferrin – ferric ions ceruloplasmin utilize H2O2 for reoxidation of copper Lung: intracellular enzymes epithelial lining fluid (GSH 100x higher than in plasma, catalase, SOD, GPx) Collagen 90% I and III, type II, V, VIII Synthesis Degradation Deposition Fibrosis Emphysema Degradation – specific MMP´s TIMP´s – tissue inhibitors of MMP´s