2006-2007 Reference Costs Guidance presentation.
advertisement

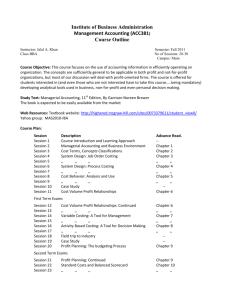
Reference Costs 2006-07 Afternoon Workshop Richard Russell, DH Ali Connell, DH PbR – Finance and Costing Team Contents • Purpose of Reference Costs • Organisational Roles and Responsibilities • Key changes since 2005-06 – HRG4 – FCE and Spells – Unbundling – Data Definitions – Collection System • Known areas of difficulty • Timetable • Resources • Patient Level Costing Purpose of Reference Costs • Annual national benchmark exercise of average unit costs from providers in England • Also serves to inform – Payment by Results: Tariff Development – Programme Budgeting – Efficiency measures – Organisational Performance Management • So whilst some changes are to inform an improved benchmark we also need to take account of its other uses Roles and Responsibilities (1) • DH, Policy and Strategy, PbR, Operations – Responsible for developing reference costs guidance, costing manual, collection system – Secretariat for the National Costing Development Group who are responsible for quality of costing in the NHS – Responsible for producing, national schedules and RCIs • Information Centre for Health and Social Care (IC) – DH commission trim points, OPCS/ICD10 to HRG mapping, HRG grouper Roles and Responsibilities (2) • Connecting for Health (CfH) – Data Dictionary – Coding Guidance • Strategic Health Authorities – Coordinating the exercise locally and answers queries from Trusts and PCTs (with support from DH as required) • Your own Finance Department – First source of advice on reference costs Reference Costs 2006-07 Communications • • • • • SHA Reference Costs Leads IC Roadshows FAQs Website Mailbox – (Diagram – next slide) What does the query relate to? What organisation? Where should I send? (Including specific subject header) PbR technical guidance NHS Trusts PbR development / policy PCT FT SHA (If SHA cannot answer) DH pbrcomms@dh.gsi.gov.uk Reference Costs collection guidance Reference Costs data returns/results Costing manual NHS Trusts SHA PCT FT (If SHA cannot answer) DH pbrdatacollection@dh.gsi.gov.uk If query is a mixture of PbR and Reference Costs questions then should go to pbrcomms@dh.gsi.gov.uk Key changes since 2005-06 HRG4 • HRG4 (note no word “version” or “vn” or “v”) – Designed by clinicians – Increased number of lines from approx 560 to over 1200 – Setting independent (APC, Outpatients, A&E, Adult Critical Care, Paediatric Critical Care, Neonatal Critical Care) – Apply equally to Admitted Patient Care and Outpatients i.e. Outpatients grouped by HRG Key changes since 2005-06 FCE and Spells (1) • Providers are paid on a Spells basis and need to measure their costs on the same basis • HRG4 is designed to be Iso-Resource at Spell level, not FCE level • So the future of Reference Costs is Spells level costs by HRG • For year on year comparability need a collection of both FCE and Spell costs Key changes since 2005-06 FCE and Spells (2) • DH issued guidance on how to get from FCE costs to Spell based costs • Point to note: – FCE collection – count FCE’s that are part of a Spell that finishes in the 2006-07 financial year – Spell level collection, group Spells that finish in the year • HRG4 Grouper assigns each FCE record the relevant FCE HRG and subsequent Spell HRG on same output file Key changes since 2005-06 Unbundling • For reference cost purposes this means services separately identified (by HRG4 Grouper) from FCE: –Chemotherapy –High Cost Drugs –Diagnostic Imaging (Radiology) –Interventianal Radiology –Renal Dialysis –Radiotherapy –Specialist Palliative Care –Rehabilitation Services • At a Spell level grouper also separately identifies these activities and does not group them within the main Spell Key changes since 2005-06 Collection System • Incorrect Trimpoints used will now ‘fail’ loading process - Vital to use correct ones • Workbook structures have been made more consistent with Guidance • Software providers • Mid May – Live testing week Key changes since 2005-06 Data Definitions and Collection structures • The reference cost guidance now links to the data dictionary wherever possible • Biggest change is Outpatients, it is now a “pre-booked appointment at a clinic” i.e. setting independent – NB possibly big impact for PCTs? • Other key changes are: – Outpatients by Staff Type – Observation wards/assessment units clarification – Critical Care counting, Periods and ACP – Renal – now HRG4 – Digital Hearing Aids – Mental Health – Mental Health Specialist Teams (Child/Adult/Elderly) – Pre-processing of data - Annex 1 – Accounts reconciliation in reconciliation statement Known areas of difficulty (1) • With the new definition PCTs are now doing Outpatients, but generally do not using OPCS/ICD10 coding • A number of organisations have not collected OPCS 4.3 since the start of the year (1 April 2006) • Collection files are larger due to HRG4 introduction • Data Collection issues for some of the areas of unbundling Known areas of difficulty (2) • Updated definitions in line with data dictionary and PbR requirements may require more local solutions than normal • PAS systems not able to fully utilise all HRG groups at this time • PCT’s post reconfiguration need to include activity and costs relating to pre configuration organisations Timetable Tools…… • Ref Costs Final guidance available – 16th Feb (DH) • Costing Manual updates – March • Final Collection Files - March • ICD10/OPCS to HRG code to HRG mapping available Feb (IC) • Toolkit documentation available March (IC) • Grouper available end April (IC) • Trim Points available early May (IC) Deadlines….. • First submission to DH – 29th June, Noon • Final submission to DH – 31st July, Noon • RCIs produced before end 2007 (DH) Resources and useful links • Reference Cost Guidance: www.dh.gov.uk/refcosts • NHS Costing Manual: www.dh.gov.uk/refcosts • HRG4 Toolkit: www.ic.nhs.uk/casemix • HRG4 Documentation: www.ic.nhs.uk/casemix • OPCS/ICD10 to HRG Mapping (code to group in excel): www.ic.nhs.uk/casemix • SHA leads contacts (details In pack and at www.dh.gov.uk/refcosts) • Reference Cost Discussion Forum (this is a users resource and whilst promoted by DH it is not used by the DH as a way of receiving queries – the route for queries is via SHA Reference Cost Leads) The Future of Costing • Response to Lawlor Review • National Costing Development Group Support • Patient Level Costing Patient Level Costing (PLC) 1 • Historically reference costs tend to be calculated by finance, on a top down basis, with little clinical validation – one hospital provided 1526 Diabetic Adult Face to Face Contacts for a total cost of £1,678 (avg of £1.10 each) – another provided 16 Intermediate Pain Procedures for a total cost of 80 pence - 5 pence each • As reference costs have been used to calculate tariff then this undermines the credibility of the tariff Patient Level Costing (PLC) 2 • PLC is a change in costing methodology to a bottom up approach. • Will allow for improved clinical engagement as discuss actual patients rather than averages • Will allow for better understanding of costs as will be able to compare cost buckets rather than just average costs • Will better support tariff development as allows for greater level of detail to be collected • Will support any future classification changes as simply sum up patient costs into whatever classification the organisation is using Patient Level Costing (PLC) 3 • There are already 5 sites implementing PLC • Up to a years implementation time and then a further year to properly bed in • Makes better use of the existing investment in place to support PbR implementation Will be supported by • Updated costing definitions and standards will be written by NHS experts • Process of peer review of quality of costing data in providers The short term • PLC is a forward looking medium to long term solution. • There is plenty that can be done now: – Service level costing – Clinical validation of costing results – Benchmarking groups – Other ideas? WRAP UP • Large scale change for 2006-07 to support HRG4 tariff and costing development – FCEs and Spells – Unbundling – OPCS4.3 • Organisations need to start planning for the reference cost collection now • Any Questions?