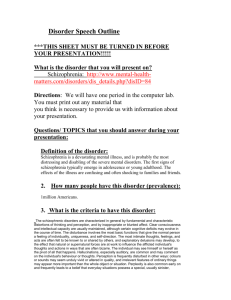
Schizophrenia
advertisement

SCHIZOPHRENIA SPECTRUM and OTHER PSYCHOTIC DISORDERS Dr. Hakan Atalay Yeditepe Üniversitesi Tip Fakültesi Psikiyatri AD Reference: DSM-V. APA, 2013 Kaplan & Sadock's Comprehensive Textbook of Psychiatry. Editors: Sadock, Benjamin J.; Sadock, Virginia A. 8th Edition, Lippincott Williams & Wilkins, 2009 HISTORY Written descriptions of symptoms commonly observed today in patients with schizophrenia are found throughout recorded history. Early Greek physicians described delusions of grandeur, paranoia, and deterioration in cognitive functions and personality. However, since these symptoms are not necessarily unique to schizophrenia, one cannot be certain whether these behaviors were actually associated with what today would be called schizophrenia. Indeed, several scholars have argued that schizophrenia is of relatively recent origin. A major impediment to distinguishing schizophrenia from other forms of psychoses was the existence of another common type of insanity, general paresis. The symptom manifestations of general paresis were quite diverse and overlapped extensively with those of schizophrenia. The cause of syphilitic insanity was subsequently traced to a spirochetal infestation, and antibiotics were eventually found to be effective in treatment and prevention. The identification of syphilitic insanity enabled Emil Kraepelin to delineate the two other major patterns of insanity: • manic-depressive psychosis and • dementia praecox (or dementia of the young), • and to group together under the diagnostic category of dementia precox the previously disparate categories of insanity, such as hebephrenia, paranoia, and catatonia. In differentiating dementia precox from manic-depressive disorder, Kraepelin emphasized what he believed to be the characteristic poor long-term prognosis of dementia precox, as compared to the relatively nondeteriorating course of manic-depressive illness. In 1911 Eugen Bleuler, recognizing that dementia was not a usual characteristic of dementia precox, suggested the term schizophrenia (splitting of the mind) for the disorder. Bleuler introduced the concept of primary and secondary schizophrenic symptoms; his four primary symptoms (the four As) were abnormal Associations, Autistic behavior and thinking, Abnormal affect, and Ambivalence. T The major alternative etiopathophysiological model conceptualizes schizophrenia as a clinical syndrome rather than a single disease entity. T This view holds that although patients with schizophrenia share a sufficient commonality of signs and symptoms to validly differentiate them from patients with other forms of psychosis (e.g., mood disorder with psychotic features, substance-induced psychotic disorder), more than one disease entity will eventually be found within this syndrome. EPIDEMIOLOGY Schizophrenia affects just under 1 percent of the world's population (approximately 0.85 percent). The number of affected individuals increases if schizophrenia spectrum disorders are included in prevalence estimates. The concept of schizophrenia spectrum disorders is derived from observations of psychopathological manifestations in the biological relatives of patients with schizophrenia. Diagnoses and approximate lifetime prevalence rates (percentage of population) for spectrum disorders are: • * schizoid personality disorder (fractional), • * schizotypal personality disorder (1 to 4 percent), • * schizoaffective psychosis (0.7 percent), and • * atypical psychoses and delusional disorder (0.7 percent). The relation of these disorders to schizophrenia in the general population is unclear, but in family pedigree studies the presence of a proband with schizophrenia significantly increases the prevalence of these disorders among biological relatives. Schizophrenia is found in all societies and geographical areas. Although comparable data are difficult to obtain, incidence and lifetime prevalence rates are roughly equal worldwide. The positive symptom component of the disorder usually becomes manifest during late adolescence and early adulthood, although there is a difference in onset associated with gender. In males, the incidence of the onset of positive symptoms peaks during years 17 to 27, whereas in females the peak incidence is a lengthy plateau between the years 17 to 37. Rural and urban incidence figures are probably similar, but there is a greater prevalence of schizophrenia among urban and lower socioeconomic populations. Deinstitutionalization has dramatically reduced the number of beds in custodial facilities, but an overall evaluation of the consequences of deinstitutionalization is disheartening. Many patients have simply been transferred to alternative forms of custodial care (instead of to treatment or rehabilitative services), including nursing home care and poorly supervised shelter arrangements. Others have been released to communities often unable or unwilling to provide the minimal requirements for clinical care or humane support. For the more fortunate patients the burden of care has shifted to the family, creating an extreme hardship for large numbers of families in this country. The less fortunate patient may either have no place to live, be forced to live in circumstances of isolation and hopelessness, or end up in jail. Patients with a diagnosis of schizophrenia are reported to account for 33 to 50 percent of homeless Americans. ETIOLOGY Neurobiological Model Psychoanalytical Model Stress-Diathesis Family, twin, and adoptive studies have long since documented a robust contribution of genetic factors to the etiology of schizophrenia, with genetic factors established as relevant to some, perhaps all, cases. However, it is not yet known which genes are involved or how the proteins they produce contribute to the pathophysiology of schizophrenia. Genetics Risk for development of sch in one of the children; •when a parent has sch: % 10-14 •when both of parents have sch: % 40-50 •when one of siblings has sch: % 10-14 •when both a sibling and a parent have sch: % 20 •Concordance for sch in monozygotic twins: % 40-50 •in dizygotic twins: % 10-14 Sch prevalence is the same in children with a biological mother who is sch and are adopted by “heathy” families as those who are raised by “insane” mother: % 10 The rate is %1 both in healthy mothers and general population. A central conceptual issue in the investigation of the etiology of schizophrenia is whether schizophrenia is a neurodevelopmental or a neurodegenerative disorder. Is the cause of schizophrenia to be found in the failure of the normal development of the brain, or is it to be found in a disease process that alters a normally developed brain? Both these options, or a combination of these options, may be true because the schizophrenia syndrome probably represents more than one disease process, or a developmental abnormality may increase the risk for the subsequent occurrence of the disorder. The explosion of information on the neurobiology of brain development has led to considerable new knowledge on the potential mechanisms of pathogenic influences. It is now clear that subtle deviations in the development of the brain could create dysfunctions associated with specific behaviors. Postmortem findings of abnormalities in neural plate formation, which suggest a deviation in programmed cell migration or reduced cell density, provide intriguing support for the proposition that the developmental process that establishes normal brain cytoarchitecture may have gone awry in schizophrenia. A Another view is that the brain has established extensive redundancy during the developing years, and that the fine-tuning necessary for efficient functioning involves eliminating certain nerve cells and many of the synapses connecting cells. A A failure to adequately prune nerve cells and synapses, or to err in selection for pruning could, in theory, underlie dysfunctions that later lead to schizophrenia symptoms. T The natural evolution of pathophysiological hypotheses of schizophrenia is the development of comprehensive models that integrate both neuroanatomical and biochemical hypotheses. T The superimposition of the neurotransmitters involved in the connections among cortical, basal ganglia, and thalamic structures that comprise the basal ganglia-thalamocortical neural circuits is a prime example of this approach. T Through glutamate projections from the cortex to the basal ganglia, the cerebral cortex facilitates the performance of selected behaviors while inhibiting others. The excitatory glutamatergic neurons terminate on GABAergic and cholinergic neurons, which in turn suppress or excite dopaminergic and other neurons. This regulatory activity can enable the cortex to protect itself from overstimulation from thalamocortical neurons. The integrative models provide a framework for identifying potential neurotransmitter targets for drug development, as well as providing explanatory models for the observed effects of pharmacological agents in patients with schizophrenia (e.g., PCP-induced psychotic symptoms mediated through the interactions of glutamate and other neurotransmitter systems in the neocortex, basal ganglia, or limbic system structures). DIAGNOSIS and CLASSIFICATION Classification Systems Post-Warld War II * use of common language * preventing chaos in decisions of disability Veterans Administration Manual (1952) DSM-II (1968) DSM-III (1980) Development of diagnostic criteria DSM-IV (2000) Simplification of criteria * Agreement between clinicians * Increase in reliability * Progress in research •Making easy for patients to obtain information DSM-V (2013) B. For a significant portion of the time since the onset of the disturbance, level of functioning in one or more major areas, such as work, interpersonal relations, or self-care, is markedly below the level achieved prior to the onset (or when the onset is in childhood or adolescence, there is failure to achieve expected level of interpersonal, academic, or occupational functioning). C. Continuous signs of the disturbance persist for at least 6 months. This 6month period must include at least 1 month of symptoms (or less if successfully treated) that meet criterion A (ie, active-phase symptoms) and may include periods of prodromal or residual symptoms. During these prodromal or residual periods, the signs of the disturbance may be manifested by only negative symptoms or two or more symptoms listed in criterion A present in an attenuated form (e.g., odd beliefs, unusual perceptual experiences). • D. Schizoaffective disorder and depressive or bipolar disorder with psychotic features have been ruled out because either: (1) no major depressive or manic episodes have occurred concurrently with the active-phase symptoms; or (2) if mood episodes have occurred during active-phase symptoms, they have been present for a minority of the total duration of the active and residual periods of the illness. • E. The disturbance is not due to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition. • F. If there is a history of autism spectrum disorder or a communication disorder of childhood onset, the additional diagnosis of schizophrenia is made only if prominent delusions or hallucinations, in addition to the other required symptoms of schizophrenia, are also present for at least a month (or less if successfully treated). Specify if: •The following course specifiers are only to be used after a 1-year duration of the disorder and if they are not in contradiction to the diagnostic course criteria. •First episode, currently in acute episode: First manifestation of the disorder meeting the defining diagnostic symptom and time criteria. An acute episode is a time period in which the symptom criteria are fulfilled. •First episode, currently in partial remission: Partial remission is a period of time during which an improvement after a previous episode are only partially fulfilled. •First episode, currently in full remission: Full remission is a period of time after a previous episode during which no disorder-specific symptoms are present. •Multiple episodes, currently acute episode: Multiple episodes may be determined after a minimum of two episodes (i.e., after first episode, a remission and a minimum of one relapse). •Multiple episodes, currently in partial remission •Multiple episodes, currently in full remission •Continous: Symptoms fulfilling the diagnostic symptom criteria of the disorder are remaining fort he majority of the illness course, with subtreshold symptom periods being very brief relative to the overall course. •Unspecified Specify if: •With catatonia (refer to the catatonia associated with another mental disorder). Specify current severity: •Severity is rated by a quantitative assessment of the primary symptoms of psychosis, including delusions, hallucinations, disorganized speech, abnormal psychomotor behavior, and negative symptoms. Each of these symptoms may be rated for its current severity (most severe in the last 7 days) on a 5-point scale ranging from 0 (not present) to 4 (present and severe). Note: Diagnosis of schizophrenia can be made without using this severity specifier. TREATMENT Treatment of Schizophrenia The somatic treatment of schizophrenia has changed substantially during the 1990s. Until 1990 when clozapine (Clozaril) was introduced in the United States, all available antipsychotic drugs had a similar range of efficacy and were associated with neurological side effects that seriously interfered with their effectiveness. Clozapine was the first of a new generation of antipsychotics that are associated with far fewer extrapyramidal side effects than older drugs and perhaps have better efficacy. Although clozapine's association with agranulocytosis has limited the number of patients who receive it, this agent plays an important role in the treatment of severe psychosis. The introduction of risperidone (Risperdal) in 1994, olanzapine (Zyprexa) in 1996, quetiapine (Seroquel) in 1997, and ziprasidone (Zeldex) in 1998 have given clinicians new alternatives for treating a large number of patients with schizophrenia. (The overall impact of these changes on the course of schizophrenia remains to be seen.) The Drug-Induced Extrapyramidal Syndromes (Acute) Drug-induced parkinsonism A generally mild parkinsonian syndrome that can recapitulate virtually every aspect of the idiopathic form. The most common manifestations are bradykinesia, an increase in muscular tone (appendicular musculature affected more than axial), and a resting tremor. Although the tremor is present less frequently than in the idiopathic variety (about 10–25% of afflicted population), it is indistinguishable from its idiopathic counterpart. It has a regular frequency (3–6 cps), is usually suppressed during volitional action of the involved body part, is exacerbated by stress and anxiety, and classically involves alternating contractions of opposing muscular groups (e.g., pronators and supinators of the forearm). Sialorrhea, seborrhea, and altered righting reflexes also can be present. D Dystonia T This is a sudden-onset, intense, sustained, and uncontrollable muscular contraction. T The cephalic musculature is most often affected (jaw, tongue, eyes, and neck) but other areas can be involved (upper extremities and back). I It generally develops shortly after the initiation (or reinitiation) of high-potency neuroleptics and occurs during falling plasma neuroleptic levels (8–12 hours after oral dosing). A Akathisia T This neuromotor syndrome consists of an unusual, generally intense, and uniformly uncomfortable sense of internal restlessness most commonly localized to the lower half of the body coupled with pacing behaviors or stereotyped restless movements. It is relieved somewhat during ambulation and is made worse when the patient lies down or is required to sit still. It can occur at any time during neuroleptic treatment (minutes to years after initiating treatment) and follows a waxing and waning course. L Late (tardive) T Tardive dyskinesia T This is an irregular, choreiform movement disorder that can be suppressed volitionally for variable periods by the patient, is generally beyond their awareness, and is exacerbated during distracting maneuvers (e.g., rapid alternating movements of the upper extremities worsen the involuntary bucco-oral choreic movements). Orobuccolingual structures and the distal upper extremities are the most commonly affected, but virtually any voluntary muscle group can be involved. Ninety-five percent of subjects with some type of tardive syndrome will manifest a choreic component. T Tardive dystonia T This is the second most common type of the tardive syndromes. D Dystonic movements are slow, variably sustained, and involuntary and may affect the limbs, trunk, neck (e.g., torticollis, spasmodic dysphonia) or face (e.g., Meige's syndrome). U Unlike the purely choreic form, tardive dystonia impairs function, is less likely to remit even if the neuroleptics are discontinued (90% still present several years after discontinuation), and can be progressive. Tardive akathisia This tardive syndrome is objectively similar to the acute form but exhibits a different treatment response profile (e.g., may be made worse by anticholinergic agents) and is less likely to be coupled with the intense internal sense of restlessness. Tardive tics Multiple tic syndromes, ranging from simple invariant motor tics to complex tics with involuntary vocalizations (tardive Gilles de la Tourette's syndrome), can develop after chronic neuroleptic treatment. Tardive myoclonus These are brief, nonstereotyped, generally asynchronous muscular jerks. This is the least common of the tardive syndromes. N Neuroleptic malignant syndrome T This unusual but potentially fatal syndrome afflicts less than 1% of subjects chronically treated with neuroleptics. Its protean features are dense muscular rigidity (axial musculature affected more than appendicular and not associated with a parkinsonian tremor), a depressed sensorium, elevated temperature (sometimes to malignant levels), elevated creatinine kinase, and myoglobinuria. Early reports suggested that it had a mortality of 10% to 30%, but with prompt neuroleptic withdrawal and proper supportive care more than 95% now survive. Subsequent rechallenge with neuroleptics is not contraindicated. OTHER TYPES OF TREATMENT PSYCHOSOCIAL TREATMENT PSYCHOTHERAPIES: INDIVIDUAL - Supportive - Dynamic - Interpersonal - CBT FAMILY GROUP - Social skills training REHABILITATION ECT OTHER PSYCHOSES DSM-V DIAGNOSTIC CRITERIA FOR SCHIZOAFFECTIVE DISORDER A. An uninterrupted period of illness during which there is a major mood episode (major depressive or manic) concurrent with Criterion A of schizophrenia. Note: The major depressive episode must include Criterion A: Depressed mood. B. Delusions or hallucinations for 2 or more weeks in the absence of a major mood episode (depressive or manic) during lifetime duration of the illness. C. Symptoms that meet criteria for a major mood episode are present for the majority of the total duration of the active and residual portions of the illness. D. The disturbance is not attributable to the effects of a substance (e.g., a drug of abuse or a medication) or another medical condition. Specify if: •Bipolar subtype: This type applies if a manic episode is a part of the presentation. Major depressive disorder may also occur. •Depressive subtype: This subtype applies if only major depressive episodes are part of the presentation. Specify if: •With catatonia Specify if: •The following course specifiers are only to be used after a 1-year duration of the disorder and if they are not in contradiction to the diagnostic course criteria. •First episode, currently in acute episode: First manifestation of the disorder meeting the defining diagnostic symptom and time criteria. An acute episode is a time period in which the symptom criteria are fulfilled. •First episode, currently in partial remission: Partial remission is a time period during which an improvement after a previous episode is maintained and in which the defining criteria of the disorder are only partially fulfilled. •First episode, currently full remission: Full remission a period of time after a previous episode during which no disorder-specific symptoms are present. •Multiple episodes, currently in acute episode: Multiple episodes may be determined after a minimum of two episodes (i.e., after a first episode, a remission and a minimum of one relapse). •Multiple episodes, currently in partial remission •Multiple episodes, currently in full remission •Continuous: Symptoms fulfilling the diagnostic symptom criteria of the disorder are remaining for the majority of the illness course, with subtreshold symptom periods being very brief relative to the overall course. •Unspecified Specify current severity: •Severity is rated by a quantitative assessment of the primary symptoms of psychosis, including delusions, hallucinations, disorganized speech, abnormal psychomotor behavior, and negative symptoms. Each of these symptoms may be rated for its current severity (most severe in 7 days) on a 5-point scale ranging from 0 (not present) to 4 (present and severe). •Note: Diagnosis of schizoaffective disorder can be made without using this severity specifier. DSM-V DIAGNOSTIC CRITERIA FOR SCHIZOPHRENIFORM DISORDER A. Two (or more) of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated). At least one of these must be (1), (2), or (3): 1. Delusions 2. Hallucinations 3. Disorganized speech (e.g., frequent derailment or incoherence) 4. Grossly disorganized or catatonic behavior 5. Negative symptoms (i.e., diminished emotional expression or avolition). B. An episode of the disorder lasts at least 1 month but less than 6 months. When the diagnosis must be made without waiting for recovery, it should be qualified as "provisional". C. Schizoaffective disorder and depressive or bipolar disorder with psychotic features have been ruled out because either (1) no major depressive or manic episode have occurred concurrently with the active-phase symptoms, or (2) if mood episodes have occurred during active-phase symptoms, they have been present for a minority of the total duration of the active and residual periods of the illness. D. The disturbance is not attributable to the physiological effects of a substance (e.g., a drug of abuse, or a medication) or another medical condition. Specify if: •With good prognostic features: This specifier requires the presence of at least two of the following features: onset of prominent psychotic symptoms within 4 weeks of the first noticeable change in usual behavior or functioning; confusion or perplexity; good premorbid social and occupational functioning; and absence of blunted or flat affect •Without good prognostic features: This specifier is applied if two or more of the above features have not been present. Specify if: •With catatonia Specify current severity: Severity is rated by a quantitative assessment of the primary symptoms of psychosis, including delusions, hallucinations, disorganized speech, abnormal psychomotor behavior, and negative symptoms. Each of these symptoms may be rated for its current severity (most severe in 7 days) on a 5-point scale ranging from 0 (not present) to 4 (present and severe). Note: Diagnosis of schizophreniform disorder can be made without using this severity specifier. DSM-V DIAGNOSTIC CRITERIA FOR BRIEF PSYCHOTIC DISORDER A. Presence of one (or more) of the following symptoms. At least one of these symptoms must be (1), (2), or (3): (1) delusions (2) hallucinations (3) disorganized speech (e.g., frequent derailment or incoherence) (4) grossly disorganized or catatonic behavior •Note: Do not include a symptom if it is a culturally sanctioned response. • B. Duration of an episode of the disturbance is at least 1 day but less than 1 month, with eventual full return to premorbid level of functioning. • C. The disturbance is not better explained for by major depressive or bipolar disorder with psychotic features or another psychotic disorder such as schizophrenia or catatonia, and is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition. Specify if: •With marked stressor(s) (brief reactive psychosis): If symptoms occur in response to events that, singly or together, would be markedly stressful to almost anyone in similar circumstances in the individual’s culture. •Without marked stressor(s): If symptoms do not occur in response to events that, singly or together, would be markedly stressful to almost anyone in similar circumstances in the individual’s culture •With postpartum onset: If onset is during pregnancy or within 4 weeks postpartum. Specify if: •With catatonia Specify current severity: •Severity is rated by a quantitative assessment of the primary symptoms of psychosis, including delusions, hallucinations, disorganized speech, abnormal psychomotor behavior, and negative symptoms. Each of these symptoms may be rated for its current severity (most severe in 7 days) on a 5-point scale ranging from 0 (not present) to 4 (present and severe). Note: Diagnosis of brief psychotic disorder can be made without using this severity specifier. DSM-V DIAGNOSTIC CRITERIA FOR DELUSIONAL DISORDER A. The presence of one (or more) delusions with a duration of 1 month or longer. B. Criterion A for schizophrenia has never been met. Note: Hallucinations, if present, are not prominent and are related to the delusional theme (e.g., the sensation of being infested with insects associated with delusions of infestation). C. Apart from the impact of the delusion(s), or its ramifications, functioning is not markedly impaired and behavior is not obviously bizarre or odd. D. If manic or depressive episodes have occurred, these have been brief relative to the duration of the delusional periods. E. The disturbance is not attributable to the physiological effects of a substance or a another medical condition and is not better explained by another mental disorder, such as body dysmorphic disorder or obsessive-compulsive disorder. Specify whether: Erotomanic type: This subtype applies when the central theme of delusion is that another person is in love with the individual. Grandiose type: This subtype applies when the central theme of delusion is the conviction of having some great (but recognized) talent or insight or having made some important discovery. Jealous type: This subtype applies when the central theme of the individual’s delusion is that his or her spouse or lover is unfaithful. Persecutory type: This subtype applies when the central theme of the individual’s delusion involves the individual’s belief that he or she is being conspired against, cheated, spied on, followed, poisoned, or drugged, maliciously maligned, harassed, or obstructed in the pursuit of long-term goals. Somatic type: This subtype applies when the central theme of the delusion involves bodily functions and sensations. Mixed type: This subtype applies when no one delusional theme predominates. Unspecified type: This subtype applies when the dominant delusional belief cannot be clearly determined or is not described in the specific types (e.g., referential delusions without a prominent persecutory or grandiose component.) Specify if: •With bizarre content: Delusions are deemed bizarre if they are clearly implausible, not understandable, or are not derived from ordinary life experiences (e.g., an individual’s belief that a stranger has removed his or her internal organs and replaced them with someone’s else’s organs without any wounds or scars). Specify if: The following course specifiers are only to be used after a 1-year duration of the disorder. •First episode, currently in acute episode: First manifestation of the disorder meeting the defining diagnostic symptom and time criteria. An acute episode is a time period in which the symptom criteria are fulfilled. •First episode, currently in partial remission: Partial remission is a time period during which an improvement after a previous episode is maintained and in which the defining criteria of the disorder are only partially fulfilled. •First episode, currently full remission: Full remission a period of time after a previous episode during which no disorder-specific symptoms are present. •Multiple episodes, currently in acute episode: Multiple episodes may be determined after a minimum of two episodes (i.e., after a first episode, a remission and a minimum of one relapse). •Multiple episodes, currently in partial remission •Multiple episodes, currently in full remission •Continuous: Symptoms fulfilling the diagnostic symptom criteria of the disorder are remaining for the majority of the illness course, with subtreshold symptom periods being very brief relative to the overall course. •Unspecified Specify current severity: • Severity is rated by a quantitative assessment of the primary symptoms of psychosis, including delusions, hallucinations, disorganized speech, abnormal psychomotor behavior, and negative symptoms. Each of these symptoms may be rated for its current severity (most severe in 7 days) on a 5-point scale ranging from 0 (not present) to 4 (present and severe). Note: Diagnosis of delusional disorder can be made without using this severity specifier. DSM-V Diagnostic Criteria for Substance/Medication-Induced Psychotic Disorder A. Presence of one or both of the following symptoms: •Delusions •Hallucinations B. There is evidence from the history, physical examination, or laboratory findings of both (1) and (2): •(1) The symptoms in Criterion A developed during or soon after substance intoxication or withdrawal or after exposure to a medication. •(2) The involved substance/medication is capable of producing the symptoms in Criterion A. C. The disturbance is not better explained by a psychotic disorder that is not substance/medication- induced. Such evidence of an independent psychotic disorder could include following: D. The symptoms preceded the onset of the substance/medication use; the symptoms persist for a substantial period of time (e.g., about 1 month) after the cessation of acute withdrawal or secere intoxication; or there is evidence of an independent nonsubstance/medication-induced psychotic disorder (e.g., a history of recurrent non-substance/medication-related episodes). D. The disturbance does not occur exclusively during the course of a delirium. Note: This diagnosis should be made instead of a diagnosis of substance intoxication or substance withdrawal only when the symptoms in Criterion predominate A in the clinical picture and when they are sufficiently severe to warrant clinical attention. Specify if: •With onset during intoxication: If the criteria are met for intoxication with the substance and the symptoms develop during the intoxication. •With onset during withdrawal: If criteria are met for withdrawal from the substance and the symptoms develop during, or shortly after, withdrawal. Specify current severity: •Severity is rated by a quantitative assessment of the primary symptoms of psychosis, including delusions, hallucinations, disorganized speech, abnormal psychomotor behavior, and negative symptoms. Each of these symptoms may be rated for its current severity (most severe in 7 days) on a 5-point scale ranging from 0 (not present) to 4 (present and severe). •Note: Diagnosis of substance/medication-induced psychotic disorder can be made without using this severity specifier. DIAGNOSTIC CRITERIA FOR PSYCHOTIC DISORDER DUE TO ANOTHER MEDICAL CONDITION A. Prominent hallucinations or delusions B. There is evidence from the history, physical examination, or laboratory findings that the disturbance is the direct pathophysiological consequence of another medical condition. C. The disturbance is not better explained by another mental disorder. D. The disorder does not occur exclusively during the course of a delirium. E. The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. Specify if: •With delusions: If delusions are the predominant symptom. •With hallucinations: If hallucinations are the predominant symptom. Specify current severity: •Severity is rated by a quantitative assessment of the primary symptoms of psychosis, including delusions, hallucinations, disorganized speech, abnormal psychomotor behavior, and negative symptoms. Each of these symptoms may be rated for its current severity (most severe in 7 days) on a 5-point scale ranging from 0 (not present) to 4 (present and severe). Note: Diagnosis of psychotic disorder due to another medical condition can be made without using this severity specifier. CATATONIA ASSOCIATED WITH ANOTHER MENTAL DISORDER (CATATONIA SPECIFIER) The clinical picture is dominated by three (or more) of the following symptoms: 1.Stupor (i.e., no psychomotor activity; not actively relating to environment). 2.. Cataplexy (i.e., passive induction of a posture held against gravity). 3. Waxy flexibility (i.e., slight, even resistance to positioning by examiner). 4. Mutism (i.e., no, or very little, verbal response (exclude if known aphasia)). 5.Negativism (i.e., opposition or no response to instructions or external stimuli). 6.Posturing (i.e., spontaneous and active maintenance of a posture against gravitiy). 7.Mannerism (i.e., odd, circumstantial caricature of normal actions). 8.Stereotypy (i.e., repetitive, abnormally frequent, non-goal-directed movements). 9.Agitation, not influenced by external stimulation. 10.Grimacing. 11.Echolalia (i.e., mimicking another’s speech). 12.Echopraxia (i.e., mimicking another’s movements). CATATONIC DISORDER DUE TO ANOTHER MEDICAL CONDITION A. The clinical picture is dominated by three (or more) of the following symptoms: •1. Stupor (i.e., no psychomotor activity; not actively relating to environment) •2. Cataplexy (i.e., passive induction of a posture held against gravity). •3. Waxy flexibility (i.e., slight, even resistance to positioning by examiner) •4. Mutism (i.e., no, or very little, verbal response (exclude if known aphasia)). •5. Negativism (i.e., opposition or no response to instructions or external stimuli). •6. Posturing (i.e., spontaneous and active maintenance of a posture against gravitiy) •7. Mannerism (i.e., odd, circumstantial caricature of normal actions) •8. Stereotypy (i.e., repetitive, abnormally frequent, non-goal-directed movements) •9. Agitation, not influenced by external stimulation •10. Grimacing •11. Echolalia (i.e., mimicking another’s speech) •12. Echopraxia (i.e., mimicking another’s movements). B. There is evidence from the history, physical examination, or laboratory findings that the disturbance is the direct pathophysiological consequence of another medical condition. C. The disturbance is not better explained by another mental disorder (e.g., a manic episode). D. The disturbance does not occur exclusively during the course of a delirium. E. The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. UNSPECIFIED CATATONIA This category applies to presentations in which symptoms characteristic of catatonia cause clinically significant distress of impairment in social, occupational, or other important areas of functioning but either the nature of the underlying mental disorder or other medical condition is unclear, full criteria for catatonia are not met, or there is insufficient information to make a more specific diagnosis (e.g., in emergency room settings). OTHER SPECIFIED SCHIZOPHRENIA SPRECTRUM AND OTHER PSYCHOTIC DISORDERS 1. Persistent auditory hallucinations occurring in the absence of any other feature. 2. Delusions with significant overlapping mood episodes: This includes persistent delusions with the periods of overlapping mood episodes that are present for a substantial portion of the delusional disturbance (such that the criterion stipulating only brief mood disturbance in delusional disorder is not met). 3. Attenuated psychosis syndrome: This syndrome is characterized by psychotic-like symptoms that are below a threshold for full psychosis (e.g., the symptoms are less severe and more transient, and insight is relatively maintained. 4. Delusional symptoms in partner of individual with delusional disorder: In the context of a relationship, the delusional material from the dominant partner provides content for delusional belief by the individual who may not otherwise entirely meet criteria for delusional disorder. UNSPECIFIED SCHIZOPHRENIA SPECTRUM AND OTHER PSYCHOTIC DISORDER This category applies to presentations in which symptoms characteristic of a schizophrenia spectrum and other psychotic disorder that cause clinically significant distress or impairment in social, occupational, or other important areas of functioning predominate but do not meet the full criteria for any of the disorders in the schizophrenia and other psychotic disorders diagnostic class. The unspecified schizophrenia and other psychotic disorder category id used in situations in which the clinician chooses not to specify the reason that the criteria are not met for a specific schizophrenia spectrum and other psychotic disorder, and includes presentations in which there is insufficient information to make a more specific diagnosis (e.g., in emergency room settings). DSM-IV Diagnostic Criteria for Shared Psychotic Disorder A. A delusion develops in an individual in the context of a close relationship with another person(s), who has an already-established delusion. B. The delusion is similar in content to that of the person who already has the established delusion. C. The disturbance is not better accounted for by another psychotic disorder (e.g., schizophrenia) or a mood disorder with psychotic features and is not due to the direct physiological effects of a substance (e.g., a drug of abuse, a medication) or a general medical condition.