Digestion: What Happens to the Food We Eat
advertisement
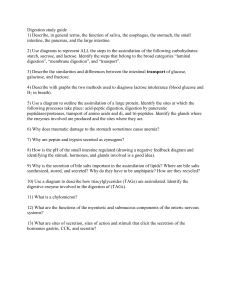
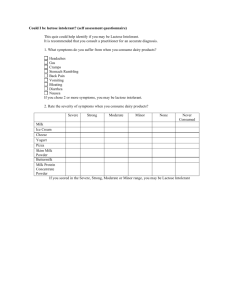
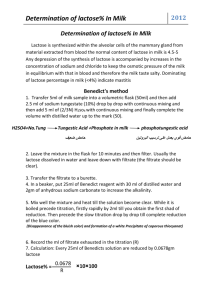
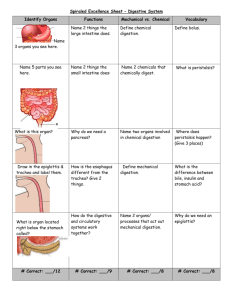
DIGESTION: WHAT HAPPENS TO THE FOOD WE EAT INGRID ADAMS, PHD, RD, LD MATTHEW SAULNIER,RD,LD HOW DO YOU MAKE FOOD DECISIONS? • What did you eat yesterday? • Why? • What will you eat for the rest of your life? • How will you decide? • Is it important to make wise food decisions? Why or why not? • What role do you have to play in this situation? The Digestive Organs DIGESTION: THE ENZYMES • Digestive enzymes are produced in the salivary glands, mouth, stomach, small intestine, and pancreas. • The pancreas produces digestive enzymes and secretes them into the duodenum via the pancreatic duct. • Most digestive enzymes are inactive until they are secreted into the GI tract – protects our cells from self-digestion. DIGESTION • Digestion occurs along the gatrointestinal (GI) tract. • Digestion requires enzymes and other chemical and physical factors. MOUTH Carbs Fats Protein Food is chewed Salivary glands: Amylase Lipase CARBOHYDRATE DIGESTION • Mouth • Starch digestion begins in the mouth. Salivary glands secrete salivary amylase. • Salivary amylase is an enzyme that breaks down starch into smaller polysaccharides and disaccharides. CARBOHYDRATES – WHAT IS DIGESTED? • Starch is the most common carbohydrate in the American diet. It is a large molecule composed of linked glucose units. • Digestion breaks starch down into single glucose molecules. STOMACH HCl Pepsin Lipase CARBOHYDRATE DIGESTION • Stomach • Starch digestion stops in the stomach where it is to acidic for salivary amylase to work. • Small Intestine • The majority of carbohydrate digestion occurs in the small intestine. • The pancreas produces pancreatic amylase, which is secreted into the small intestine once food enters from the stomach and breaks down food into very small chains of glucose • The cells that line the small intestine break down carbohydrates into simple sugars, which are absorbed directly into the blood stream. SMALL INTESTINE Duodenum Liver – produce bile which is stored in the gall bladder Pancreas Amylase Lipase Trypsin Chymotrypsin Dietary fibers, other large molecules (undigested proteins, triglycerides, starches, etc…) LARGE INTESTINE CARBOHYDRATE DIGESTION • Absorption • Glucose units are absorbed into the intestinal wall and pass into the bloodstream. • Dietary fibers: NOT DIGESTED OR ABSORBED in the small intestine PROTEIN DIGESTION • Mouth • No digestion of protein occurs here. • Stomach • Stomach acid, hydrochloric acid, beings to break down protein molecules. • Hydrochloric acid activates an enzyme called pepsin, which breaks down protein into small polypeptides. PROTEIN DIGESTION • Small Intestine • Once these polypeptides enter the small intestine, enzymes form the pancreas and intestine break down these chains into amino acids. • Intestinal cells absorbed amino acids just like carbohydrates. • Absorption • Amino acids enter the intestinal cells and pass into the bloodstream. FAT DIGESTION • Digestion of fat is slightly different from carbohydrates and protein. • Mouth • Lingual lipase mixes with food. Lingual lipase plays a more prominent role in children. • Stomach • Lingual lipase acts in the stomach where it prefers a more acidic environment. FAT DIGESTION • Small Intestine • Triglycerides mix with the bile from the gallbladder and form micelles. The water soluble lipases from the pancreas and intestine act on the triglycerides in the suspended micelles. • The main products of triglyceride digestion are fatty acids and monoglycerides. • Absorption • Fatty acids, glycerol, and monoglycerides pass into the intestinal cells and are reassembled into triglycerides. They are then packaged into chylomicrons and enter the lacteals of the lymphatic system. WHAT IS NOT ABSORBED IN THE SMALL INTESTINE? • Dietary fibers, other large molecules (undigested proteins, triglycerides, starches, etc…) • Many food additives are digested to be unobservable, for safety and to reduce caloric content of the diet. AFTER ABSORPTION, THEN WHAT? • Fats, cholesterol, and fat soluble vitamins are repackaged in the intestinal cell, sent through the lacteal (lymphatic system), enter the general circulation through the thoracic duct. • Most other nutrients are sent through capillaries from the small intestine to the portal vein and go directly to the liver. • Liver processes sugars to glucose; amino acids to whatever amino acids are needed. PROBLEMS WITH DIGESTION HIATAL HERNIA • Portion of stomach pressed into chest cavity through esophageal hiatus (passageway for esophagus) of diaphragm • Symptoms: GERD, dysphagia (swallowing difficulty), heartburn, and epigastric pain. • Rx: weight control and methods used to control GERD DISEASES OF THE STOMACH AND SMALL INTESTINE—PEPTIC ULCER DISEASE (PUD) PUD: Ulceration of the gastric or duodenal mucosa penetrating the submucosa with potential for perforation Antrum Duodenum LACTOSE INTOLERANCE • Insufficient lactase production in brush border • Poor digestion of lactose PRIMARY LACTASE NON-PERSISTENCE PREVALENCE IN US Northern European American Mexican American African American Asian American Native American Vietnamese American 5% 62% 80% 90% 95% 100% LACTOSE INTOLERANCE—SYMPTOMS • Symptoms usually begin 30min to 2hrs after consuming lactose • Crampy pain • Bloating, flatulence • Fermentation of lactose by colonic bacteria (CO2, H2, methane) • diarrhea • Lactose draws water into gut by osmosis peristalsis fluid, electrolyte, nutrient losses • Nausea LACTOSE INTOLERANCE—SYMPTOMS • Severity of symptoms depend on • Degree of lactase insufficiency • Lactose load • Many lactase insufficient individuals can tolerate some lactose • Some enzyme activity often present to varying degrees • Fermentation of undigested lactose by colonic microorganisms • Up to 1 cup of milk (12g of lactose) WITH MEAL can be well tolerated without significant symptoms by those who are lactose maldigesters SOURCES OF LACTOSE • Lactose naturally present only in milk and products made from milk • 7% human milk • 5% cows milk • 4.5 % goat milk • Usually less lactose in milk products than in milk • Yogurts—less lactose than milk; may contain active bacterial cultures capable of metabolizing lactose • Ice cream—fair amount compared with milk • Cottage cheese—contains little lactose; can usually be eaten with no adverse effects • Hard cheeses—contain less than cottage cheese LACTOSE INTOLERANCE • Remove lactose to the level of tolerance • Consume lactose containing foods with meals • dilutes lactose and slows its movement • Elimination of lactose worsens tolerance less favorable mix of colonic microflora • Fermented milk products (yogurt with active cultures) • Non-fermented milk products (acidophilus milk or yogurt milk) may or may not be tolerated • Chocolate and whole milk better tolerated than skim • Aged cheese well tolerated • Cottage cheese and ice cream—lower lactose content than milk LACTOSE INTOLERANCE—MNT • Lactose free milk • Enzyme replacement—lactase tablets • Dairyease®, Lac-Dos®, Lactaid®, Lactrase®, RiteAid® Dairy Relief™, Surelac®, Walgreens® Dairy Digestive™ • Check medication labels • powder filler used in medication may contain lactose • Teach patients to read foods labels for hidden sources • Ca, vitamin D, vitamin B12, and riboflavin supplementation depending on milk intake CELIAC DISEASE Also known as: Gluten sensitive enteropathy Celiac sprue Nontropical sprue Prevalence: 1 in 133 Higher prevalence in females Underdiagnosed—symptoms resemble those of other diseases • Caused by an allergic reaction to protamine in certain grains • • • • • • • CELIAC DISEASE (CD) Also known as: Gluten sensitive enteropathy Celiac sprue Nontropical sprue Prevalence: 1 in 133 Higher prevalence in females Underdiagnosed—symptoms resemble those of other diseases Caused by an allergic reaction to protamine in certain grains OFFENDING GRAINS Grain Prolamin Wheat gliadin Rye secalin Barley hordein Oats? avenin Certain peptides from these proteins induce the celiac response in sensitive individuals. OFFENDING GRAINS • Triticale – hybrid of rye and wheat • Spelt – wheat • Kamut – wheat • Einkorn – wheat • Emmer – wheat • Wheat (bulgur, wheat bran or germ, wheat germ oil, wheat starch or food starch, couscous, pastas made from wheat, matza, seitan, semolina) • Barley (malt) “GLUTEN” • Protein found only in wheat • The main protein in wheat • Composed of glutenin and gliadin • The term “gluten” has come to mean any cereal peptides inducing a celiac response • What is the celiac response? • Both cellular and humoral • Lymphocyte infiltration of the intestinal epithelium • Flattening of the villi VILLUS ATROPHY The Internet Pathology Laboratory, University of Utah CLASSIC SYMPTOMS • Weight loss, wasting • Weakness, malaise • Failure to thrive (FTF), short stature • Dental enamel defects • Iron deficiency anemia (Fe malabsorption; occult blood loss) • Steatorrhea • Diarrhea due to malabsorption • Constipation in some cases • Irritability in children • Abdominal discomfort, bloating, flatus, belching, GERD • Physical signs of nutrient deficiency More on symptoms • Many celiacs do not exhibit the classic symptoms • Some have no clinical GI symptoms • Because of many and varied symptoms: – Average time to diagnosis CD: 11 years! Dermatitis herpetiformis (DH) medline plus Graphics: Microsoft Online, USDA Food and Nutrition Services Ingrid Adams, Ph.D., R.D. L.D. Associate Professor , Nutrition and Food Science, University of Kentucky Extension Specialist for Physical Activity and Weight Management Date: February 27, 2015 Policy The Cooperative Extension Service is federally mandated to take affirmative steps to ensure that its programs and services are available to all people. One step is public notification of its intention to serve all audiences. All Extension materials intended for public distribution must include the following statement: Educational programs of Kentucky Cooperative Extension serve all people regardless of race, color, age, sex, religion, disability, or national origin. Letterhead, enclosure slips, and newsletters must also include the following "cooperating" statement: UNIVERSITY OF KENTUCKY, KENTUCKY STATE UNIVERSITY, U.S. DEPARTMENT OF AGRICULTURE, AND KENTUCKY COUNTIES,