Introduction trigger point dry needling
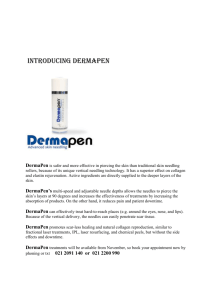
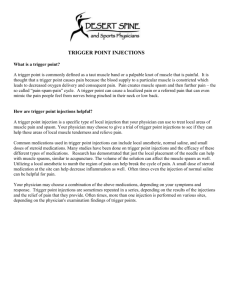
advertisement

Nichole Bluemle PT, DPT, MS, CSCS, OCS Objectives Define Dry Needling Define Trigger Point Causes of Trigger Points Goals of Dry Needling Mechanism of Dry Needling Contraindications Risks/Complications/Adverse Reactions Technique Post Treatment Reasons for failure APTA Stance NM PT State board Summary Recommended Resources Video overview http://www.youtube.com/watch?v=1bsteDCjwg Trigger Point Dry Needling TDN, Functional Dry Needling (FDN), Intramuscular Stimulation (IMS), Intramuscular Manual Therapy (IMT) Invasive procedure where a monofilament needle is inserted into a trigger point Called dry needling because it does not involve injection of a “wet” substance like trigger point injections Myofascial Trigger Point “Hyperirritable spots in skeletal muscle associated with hypersensitive palpable nodules in a taught band.” (Travell and Simons 1992) Characteristics of Myofascial Trigger Points Localized tenderness upon palpation of a taut band of muscle LTR to cross-fiber stimulation of a taut band Pain to deep palpation that is recognized pain Referred pain to a characteristic region based on myofascial referral maps Autonomic phenomena (sweating, piloerction, vasomotor) Referral Maps Causes of Trigger Points Repetitive movements/low level muscle contractions Compressive forces Trauma (contusion/strain) Unaccustomed eccentric contractions/ eccentric contractions in untrained muscles (DOMS) Emotional stress Postural stress Dehydration Goal of Dry Needling Illicit a local twitch response (LTR) in involved muscle Desensitize hypersensitive musculoskeletal structures while restoring motion and function Mechanisms of Dry Needling Releasing shortened muscles Removing irritation of spinal nerve roots by relieving short paraspinal muscles Promote healing through local inflammation response (increased blood flow to include platelet derived growth factor) Decrease spontaneous electrical activity and biochemicals in myofascial trigger points Decrease pain associated with myofascial trigger points Mechanical Effects (Dommerholt J. 2004) Disrupts the integrity of dysfunctional motor end plates Cause a LTR Alter muscle fiber length Neurophysiological Effects (Baldry PE. 2001) Suggests that dry needling stimulates Adelta nerve fibers (type III) for 72 hours post-needling Prolonged stimulation of A-delta fibers may activate enkephalinergic inhibitory dorsal interneurons Activate descending inhibitory systems which would block noxious stimulus into the dorsal horn Chemical Effects (Shah J. et al. 2005) Decrease in chemicals at the active trigger point location immediately after a local twitch response Bradykinin CGRP (calcitonin gene related peptide) Substance P Contraindications Denial of consent High level patient fear/apprehension Bleeding disorders or on anti-coagulants Pregnancy Directly over joint replacement/breast implant/pacemaker Infection/illness Unstable bone injury Malignant tumor Risks/Adverse Reactions Pneumothorax Vasovagal reaction Muscle soreness Fatigue Bruising Pain during insertion Infection Always a possibility but reduced likelihood by adhering to sterile guidelines Minimize Infection Risk Always wash hands between patients Treatment area well lit and clear of clutter Sterile, one time use individually packaged needles Clean treatment field (alcohol pad) Sharps container closed between patients Single use firm fitting gloves Needle Technique Identify anatomical landmarks, taut band, and the trigger point Clean the area with alcohol pad Place the needle over the trigger point and tap into skin at a 90deg angle (angle may need to be altered based on anatomy) Advance the needle into the trigger point Piston (redirect the needle, pull the needle up to the subcutaneous layer, redirect, again advance into muscle) Remove needle and apply direct pressure Post-treatment Re-evaluate Stretch/PROM/AROM Instruct patient in self mobilization techniques Heat Movement facilitation tape Hydration Reasons for Failure Diagnostic error Incomplete management of perpetuating factors Trigger point missed or inadequately treated Referred zone treated Inadequate post care Scope of Practice Determined by individual state board if in scope of practice and if/what training requirements must be met Many states determine dry needling to be in the scope of practice for Physical Therapists, Acupuncturists, Chiropractors Summary Dry needling performed by a trained clinician (PT, DO, DC, L.Ac) can relieve myofascial pain caused by trigger points commonly involved in orthopedic conditions Release shortened muscles Reduce spontaneous electrical activity at the neuromuscular junction Return biochemicals that cause hypersensitization to normal levels Promote self healing Recommended Resources Questions? Contact Info: Nichole Bluemle PT, DPT, MS, CSCS, OCS www.durangophysicaltherapy.com durangoPT@gmail.com