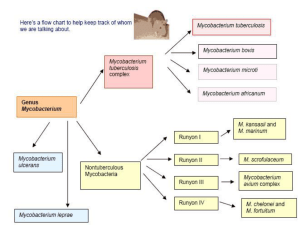
Mycobacterium
advertisement

THE FOLLOWING SLIDE SHOW HAS BEEN RATED PG PRETTY GROSS STUFF SOME MATERIAL MAY NOT BE SUITABLE FOR CHILDREN Mycobacterium: Physiology & Structure • Name from Myces and Bakterion, Fungus-like Rod • Gram + • Bacillus • Aerobic • Nonmotile • Acid-Fast Staining • Mycolic Acid in Cell Wall • Complex Cell Wall • Intracellular Parasite • Diseases From Immune Cell Wall • Complex • Contains Mycolic Acid – Lipids account for 60% of Cell Wall Weight • Responsible for Many Characteristics – – – – – – Acid Fastness Slow Growth Resistance to Detergents Antibiotic Resistance Antigenicity Clumping The Cell Wall • Figure 29-1 Mycobacterial cell wall structure. The components include the (A) plasma membrane, (B) peptidoglycans, (C) arabinogalactan, (D) mannose-capped lipoarabinomannan, (E) plasma-associated and cell wall-associated proteins, (F) mycolic acids, and (G) glycolipid surface molecules associated with the mycolic acids. (Redrawn from Karakousis et al: Cell Microbiol 6:105-116, 2004.) Really Important Mycobacteria Organism Historical Derivation M. tuberculosis tuberculum, a small swelling or tubercle; osis, characterized by (characterized by tubercles; refers to the formation of tubercles in the lungs of infected patients) M. leprae lepra, of leprosy (the cause of leprosy) M. avium avis, of birds (causes tuberculosis-like illness in birds) M. intracellulare intra, within, cella, small room (within cells; refers to the intracellular location of mycobacteria) BOX 29-1. Important Mycobacteria Mycobacterium tuberculosis Pathogenesis & Immunity • • • 1. 2. 3. Intracellular Pathogen Lifelong Infection Pulmonary Infection Arrives at Alveoli Phagocytized by Alveolar Macrophages M. tuberculosis Blocks Phagosome From Fusing With lysosome (not nutrient containing vesicles, though) 4. Other Phagocytes Are Attracted 5. Forms Multinucleated Giant Cells (Langhans Cells) Pathogenesis & Immunity • Infected Macrophages May Spread Infection 6. Stimulates TH Cells and TC Cells 7. Formation of Granulomas – – Can Lead to Elimination of Bacteria If Larger Than 3mm Become Encapsulated • M. tuberculosis can remain dormant for years in this state Pathogenesis & Immunity Epidemiology • 2 Billion People Infected World Wide – ONE-THIRD of the human population • 8.8 Million New Cases / Year • 2 Million Deaths / Year • 14,517 Cases in US in 2004 (11 in Idaho) Mycobacterium leprae Pathogenesis & Immunity • Causes Leprosy – Hansen’s Disease • Affects Skin and Peripheral Nerves Different Immune Responses Cause Different Forms • Tuberculoid • Lepromatous – Abundance of Bacteria in Two Types of Cells • Dermal Macrophages • Schwann Cells Figure 29-7 Lepromatous leprosy. Diffuse infiltration of the skin by multiple nodules of varying size, each with many bacteria. (From Cohen J, Powderly WB: Infectious diseases, ed 2, St Louis, 2004, Mosby.) Pathogenesis & Immunity Features Tuberculoid Leprosy Lepromatous Leprosy Skin lesions Few erythematous or hypopigmented plaques with flat centers and raised, demarcated borders; peripheral nerve damage with complete sensory loss; visible enlargement of nerves Many erythematous macules, papules, or nodules; extensive tissue destruction (e.g., nasal cartilage, bones, ears); diffuse nerve involvement with patchy sensory loss; lack of nerve enlargement Histopathology Infiltration of lymphocytes around center of of epithelial cells; presence of Langhans cells; few or no acid-fast rods observed Predominantly "foamy" macrophages with few lymphocytes; lack of Langhans cells; numerous acid-fast rods in skin lesions and internal organs Infectivity Low High Delayed hypersensitivity Reactivity to lepromin Nonreactivity to lepromin Immunoglobulin levels Normal Hypergammaglobulinemia Erythema nodosum Absent Usually present Immune response Table 29-2. Clinical and Immunologic Manifestations of Leprosy Pathogenesis & Immunity Figure 29-6 Tuberculoid leprosy. Early tuberculoid lesions are characterized by anesthetic macules with hypopigmentation. (From Cohen J, Powderly WB: Infectious diseases, ed 2, St Louis, 2004, Mosby.) Pathogenesis & Immunity • Figure 29-5 Acid-fast stains of skin biopsies from patients with (A) tuberculoid leprosy, (B) borderline tuberculoid leprosy, (C) borderline lepromatous leprosy, and (D) lepromatous leprosy. Note that there is a progressive increase in bacteria going from the tuberculoid form to the lepromatous form of the disease. Epidemiology • 286,063 New Cases in Early 2005 • 21% Decrease Between 2004 and 2003 • ~20% Reduction in New Cases For The Last Three Years • Prevalence Has Fallen By 90% Since 1985 • 105 Cases in The US in 2004 • 16 countries -- Bangladesh, Brazil, Cambodia, Democratic Republic of the Congo, Ethiopia, Guinea, India, Indonesia, Madagascar, Mozambique, Myanmar, Nepal, Niger, Nigeria, Philippines, and Sudan -- reported more the 90% of the world's leprosy cases. • Listed By CDC In “CANDIDATE DISEASES FOR ELIMINATION OR ERADICATION” • Suseptability Gene found in 2003 by Canadian Team (http://www.cbc.ca/stories/2003/02/10/leprosy030210) Global distribution of leprosy, showing prevalence rates: 2.0–4.1 per 10,000 (9 countries) 1.0–2.0 per 10,000 (3 countries) 0.0–1.0 per 10,000 (data from only 73 countries) Epidemiology • Endemic in Texas and Louisiana… In Armadillos Lab Diagnosis • Box 29-5 • Detection – Acid-Fast Stain – Lung X-rays – Tuberculin skin test • Intradermal injection of mycobacterial antigens • Antigens used in skin test come from protein derivative of the cell wall • Inoculated into the intradermal layer • Measured 48 hours later • Positive test develops 3-4 weeks after exposure to M. tuberculosis Table 29-3 for Results Skin test Induration~ Increase inflammation and marked by loss of elasticity and pliability Reaction is measured Treatment, Prevention, & Control • Treatment – Slow growing and hard to treat (resistance) – Must be taken over long periods of time with multiple other antibiotics (6-9 months) – Regimens start with isoniazed (INH), ethambutol, pyrazinamide, and rifampin (2 months) – Followed with 4-6 months of INH, rifampin, and other combination drugs Treatment, Prevention, & Control • Prevention – Treatment regimens are working and reducing the overall occurrence – Vaccinations are used in prevalent areas • (Can’t be used for immunocompromized patients) • Control – Elimination is highly unlikely, however, it can be controlled – Active surveillance and monitoring with therapeutic intervention – 44% decrease in (drug-resistant) tuberculosis in New York from 1991-1996