Bronchiolitis Guidelines and Evidence
advertisement

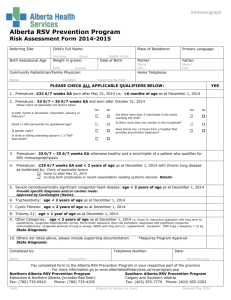
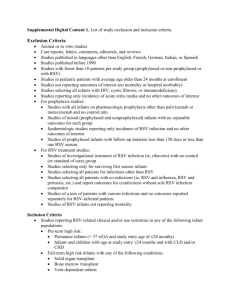
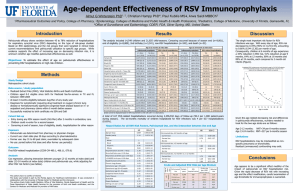
RSV Bronchiolitis Mark A. Brown, M.D. Professor of Clinical Pediatrics Pediatric Pulmonary Section University of Arizona Bronchiolitis: Definition Viral infection of the lower respiratory tract characterized by acute inflammation, edema, and necrosis of epithelial cells lining small airways, increased mucus production, and bronchospasm AHRQ Evidence Report Epidemiology • Bronchiolitis statistics – 90% of children 0-2 yrs. are infected with RSV – 20% have lower respiratory infection – 3% hospitalized – 0.002% mortality • Age at presentation – Peak age 2-5 months – Rare in 1st month of life Viral causes of bronchiolitis • Respiratory syncytial virus (RSV): • Metapneumovirus – Newly identified paramyxovirus – Similar seasonality and course to RSV • Parainfluenza • Influenza • Adenovirus • Bocavirus } 70% 10-20% 10-20% ? Seasonality Bronchiolitis RSV Isolates Year Hall, NEJM 2001 RSV Prime Cause of LRTI in Young Child Hospitalization for RSV Bronchiolitis: • 38% of all LRTI in first year of life • 22% of all LRTI in 5 years of age • 31 / 1,000 children < 12 mos each year Shay ’99 Economic Burden Costs for LRTI hospitalizations: • $2.25 billion for infants, 14 to 26% from RSV • $3.73 billion for first 5 years of life, 1016% from RSV Stang ’01 Clinical course of bronchiolitis Incubation period: Upper respiratory infection: Worsening lower airway disease: Full recovery: Percent • • • • 2-8 days 1-3 days 3-5 days 2-8 weeks 100 80 60 40 20 0 0 5 10 15 20 25 Days of symptoms 30 35 Swingler et al. 2000 Severity Clinical course 0 0 5 10 15 5 20 25 10 15 Days 20 25 30 35 Risk Factors for Hospitalization with RSV 1708 Hospitalized Infants in Rochester, NY 80 70 1 or more Risk Factors Percent with: 60 50 40 30 20 10 0 Prematurity Chronic Disease Age < 6 wks RSV Roentgenographic Findings • Diffuse interstitial pneumonitis most common in all lobes • Hyperaeration > 50% • Peribronchial thickening • Lobar or segmental consolidation 2050%; RUL, RML most common Therapy for RSV Oxygen, administered by means of a small tent, gives these patients with cyanosis definite relief, and is the treatment upon which we have to rely for the most severely ill infants. J. Adams, Lancet 1945 Therapies • Supportive care – Airway clearance – Hydration – Oxygen • Bronchodilators Supportive Care • Administer humidified oxygen • Nasal suctioning to clear upper airway • Monitor for apnea, hypoxemia, and impending respiratory failure • Normalize body temperature • Rehydrate with oral or intravenous fluids • Monitor hydration status Supportive Care • Chest Physiotherapy (CPT) – Little evidence to confirm enhancement of mucociliary clearance Quittell LM, et al. Am Rev Respir Dis. 1988;137:406A; QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. Bronchodilators • Multiple studies of bronchodilators – Albuterol • Beta2 adrenergic effects – Racemic epinephrine • Beta2 adrenergic effects • Alpha adrenergic effects - ? vasoconstriction – Anticholinergics • No evidence for benefit in bronchiolitis Effect on clinical score: Cochrane meta-analysis Hartling et al. Cochrane Review 2004 Odds of improvement Hartling et al. Cochrane Review 2004 Effect on hospitalization Hartling et al. Cochrane Review 2004 Bronchodilators • Evidence for modest short-term improvement – Overall, 57% improved vs. 43% for placebo – 1 infant will benefit for every 7 treated • Mild side effects common: tachycardia, hypoxemia • No impact on overall course of disease in inpatients Albuterol Dobson et al. Pediatrics. 1998; 101:361-368. Epinephrine Wainwright et al, N Eng J Med 2003; 49:27-35. • Studies comparing epinephrine vs. albuterol mixed Hartling et al. Cochrane Review 2004 Bronchodilators and bronchiolitis Bronchodilators have variable effects on infants with bronchiolitis… Some improve…some get worse…and the rest stay the same Unknown Therapies Supportive Care • Suctioning/Airway Clearance – Upper airway congestion can contribute to symptoms – No evidence for role of deep suctioning – One RCT suggests benefit for using 3% saline with nebs Sarrell, et al. Chest 2002; 122:2015-2020. • Chest physiotherapy – One small RCT found no benefit of routine Chest PT Webb et al. Arch Dis Child 1985; 60:10781079. • Hydration – Assess and follow I/Os (potential for SIADH) Oxygen • Pulse oximetry detects hypoxemia not apparent on PE • Significance of mild hypoxemia (> 90%) unclear – Variability in saturation due to plugging / mismatch – Indication for starting oxygen unclear – Oxygen requirement associated with worse outcomes • Increased risk of need for ventilation Wang et al. J Peds 1995; 126:212-219. • 4 x increased inpatient LOS Wainwright et al. 2003 – ? Continuous pulse oximetry vs. spot checking Protection against lower respiratory infection Natural immunity to RSV • Antibody to F and G surface proteins protect against LRI • Humoral immunity controls and terminates infection Reinfections with RSV • Usually limited to URI • Healthcare workers at risk • Significant cause of illness in elderly Prevention • Non-Specific Measures – Avoidance – Hygiene – Nutrition • Passive Immunization – Palivizumab (Synagis®) RSV immunoprophylaxis Attempts to provide immunity to RSV • Vaccine in 1960s worsened course of infection • New intra-nasal vaccine undergoing trials • Passive immunity via hyperimmune globulin • Monoclonal antibody to F protein (palivizumab) – 55% hospitalizations for preterm/chronic lung disease – 45% hospitalizations for congenital heart disease Reduction in RSV Hospitalization Rate 1996-1997 IMpact-RSV Trial-Placebo 2000-2001 Synagis Outcomes Registry 2002-2003 Synagis Outcomes Registry 14 RSV Hosp Rate 12 1996-1997 IMpact-RSV Trial-Synagis 2001-2002 Synagis Outcomes Registry 12.8 11 10.6 9.8 10 8.1 7.9 8 6 4 2 5.8 4.8 5.8 4.5 2.9 1.8 2.1 1.5 1.1 1.7 1.6 1.2 1.2 2 2.2 1.6 1.3 1.9 0.7 0 All Patients Premature All <32 weeks All 32-35 Patients with w/o CLD GA weeks CLD IMpact-RSV study based on active collection of hospital data; Outcomes Registry based on passive reporting The IMpact-RSV Study Group. Pediatrics. 1998;102(3):531-7; Palivizumab Outcomes Study Group. Pediatric Pulm. 2003;35:484-9; Hudak et al. J Perinatol. 2002;22:619, abstract P32; Data on file, MedImmune Inc. Guidelines for RSV Prophylaxis Premature, no CLD, no CHD ≤28 wks GA Palivizumab if ≤12 months at start of RSV season 29-32 wks GA Palivizumab if ≤6 months at start of RSV season 32-35 wks GA Palivizumab if ≤6 months at start of RSV season with two risk factors present Hemodynamically Significant CHD Palivizumab if ≤2 years old at start of RSV season Chronic Lung Disease* (CLD) *Receiving medical therapy for CLD within 6 months Apnea and RSV • Apnea reported in 20% of hospitalized infants with RSV • Risk factors for apnea – Age < 2-3 months – Prematurity • May be presenting symptom but usually follows URI/LRI • Recurrence rate 50% • Mortality < 2% Levine et al. 2004 RSV and asthma link • 40-50% of hospitalized bronchiolitics will wheeze again – Increased risk if > 12 months, atopy, eosinophilia Reijonen 1997 Ehlenfield 2000 Martinez FD, Godfrey S, 2003 Otitis media • Otitis media a common complication – Cohort study of 42 infants with bronchiolitis • 62% acute OM (tympanocentesis confirmed) • 24% otitis media with effusion • 14% normal throughout course Andrade et al. 1998 – Usual guidelines for AOM and OME apply May there never develop in me the notion that my education is complete, but give me the strength and leisure and zeal continually to enlarge my knowledge. Moses Maimonides