Prevention of Medical Errors
advertisement

Prevention of Medical Errors
KIMBERLY REED, O.D., FAAO
No financial disclosures
Welcome
• Goals
•
•
Fulfill obligation as licensed optometrists
Promote wellness as individuals
• Course Overview and Format
•
Medical Errors
•
Statistics
•
Types/definitions
•
•
•
Hospital based errors
•
Medication errors
Root cause analysis and prevention
EMR/EHR
•
Help or hindrance?
Florida’s requirements
• Florida Rule 64B13-5.001 (8)
•
Last updated 2006
• “Must include a study of root-cause analysis,
error reduction and prevention, and patient
safety”
Errors made by our
colleagues
Dilated with 1% tropicamide?
Samples of artificial tears?
Expired samples
IOM, 1999: To Err Is Human: Building a Safer Health System
•
Between 44,000 and 98,000 people
die every year due to preventable
errors in U.S. hospitals
Responses to IOM Report
• CE requirements
• Mandatory or voluntary systems for reporting
medical errors (National Quality Forum, 2007)
• Joint Commission (JCAHO) requires healthcare
institutions to analyze errors using root cause
analysis
Responses to IOM Report
• Patient Safety and Quality Improvement Act
(database)
• Centers for Medicare and Medicaid Services –
will not reimburse hospitals for treatment of 8
preventable errors
•
Medicaid, Aetna, BCBS, etc. following suit
Healthcare Associated Infections (HAI)
• 100,000 deaths per year
• Leading complication of hospital care
Agency for Healthcare Research
and Quality
AHRQ.GOV
• $50 million annually to research patient safety
•
Grants ranging from $400 – 1.2M to study HAI prevention
Postoperative sepsis per 1000
elective-surgery
Based on income….postoperative sepsis
• Lowest income
• Highest income
• Self pay
• Medicaid
Children who needed care right
away who didn’t get it
• White
• Hispanic
• Black
• English speaking
• Non-English speaking
Responses to IOM report
• President Clinton tried to implement mandatory reporting
system for medical errors
• Lobbied
• 81
against by AMA and AHA
million dollars
• “If medical errors and infections were better tracked, they
would easily top the list {of cause of death in the U.S.}. In
fact, a visit to your doctor or a hospital is twice as likely to
result in your death [than] a drive on America’s highways.”
Where are we now?
• IOM set a goal of 50% reduction in errors by
2004
HealthGrades Patient Safety (2004)
• Study of 37 million patient records, all Medicare,
in 50 states + DC.
•
Medicare 45% of all hospital admissions excluding OB
• 195,000 deaths annually due to in-hospital
medical errors (2000-2002)
• Since the original report in 1999:
• 1 - 2 million more people have died due to
preventable medical errors or hospital-acquired
infection
January 2012 report
• Reported January 6 in NY Times
• Department of Health and Human Services
• Medicare patients
•
Hospitals are required to track medical errors and adverse
patient events and conduct a root cause analysis
• Records review by independent doctors
• How many medical errors are reported?
Recalculating…….recalculating…..
• 130,000 Medicare beneficiaries experience one
or more adverse events in hospitals
• EVERY MONTH
Raleigh General Hospital, W.Va.
• Anesthetic Awareness
• Patients can feel all the pain, pressure, discomfort
during surgery…but cannot move or communicate
with doctors
• Occurs between 20,000 and 40,000 patients
every year
• Attributed to physician error or faculty equipment
•
Sometimes only part of the drugs are administered
• W.Va. Patient committed suicide
Who makes the IV bags?
• Two year old girl receiving IV chemo
• Saline base prepared before adding chemo
agents
•
Saline was 20 times stronger than ordered
• High concentration of sodium caused brain
edema and coma
• Child died 3 days later
Who makes the IV bags?
• Pharmacy tech
• High school diploma
• Pharmacist overseeing the work was fired,
convinced of involuntary manslaughter
•
Jail time
•
House arrest
•
Loss of license, career
•
Fined
Who makes the IV bags?
• Pharm techs have something to do with
approximately 96% of pharmacy prescriptions
• “Culture of Silence”
Who is “attending” you?
• Medical Model Education
• Student/intern?
• Resident?
• Chief resident?
• Attending?
Who is “attending” you?
• Fatal oversight:
•
Second year student doing “rounds” at UPenn
•
71 year old patient recovering from hip replacement surgery
•
SOB, sweating
•
Classic signs of pulmonary embolism
•
“I hadn’t read that chapter yet”
•
Patient died
Adding to the problem
• Most people feel that medical errors are the
failures of individual providers
•
Delays in diagnosis and treatment?
But…
• IOM showed most medical errors are “systems
related”
Why do medical errors occur?
• “Systems” errors
• Fatigue*
•
•
•
Brigham and Women’s & Harvard
3x higher error rate with 1x/ month 24 hour shift
7x higher error rate with 5x/month 24 hour shifts
• Lack of knowledge
•
•
6000 known diagnoses
4000 available drugs
• Lack of communication
*www.plosmedicine.org
Why do medical errors occur?
• Poor charting
• Impaired care providers
•
•
•
Survey of 1662 respondents
46% failed to report at least one serious medical error
45% failed to report an incompetent or impaired colleague
*www.plosmedicine.org
Root Cause Analysis
• “A process for identifying the basic factors that
underlie variation in performance, including the
possible occurrence of a sentinel event.”
• Focuses on systems and processes, not on
individual performances
Type of Event
Total events 2004-2011
Wrong patient, wrong site, wrong
procedure
782
Unintended retention of FB
606
Op/postop complication
604
Delay in treatment
646
Fall
439
Suicide
568
Medication error
319
A Case with a Bit More Relevance
• “The fiasco which left seven veterans blinded”
•
Vawatchdog.org
• 62 year old male veteran suffered “significant
visual loss in one eye as a result of poorly
controlled glaucoma”
•
January 2009
A Case with a Bit More Relevance
• In June 2005, the patient was diagnosed as a
“glaucoma suspect”
•
Allegedly, treatment wasn’t initiated
• Prompted a review of 381 charts
•
23 glaucoma patients experienced “progressive visual loss” while
receiving treatment in the Optometry department
• Root Cause Analysis:
•
Patients were not being sent to ophthalmology for treatment
(required by hospital)
•
Some OD’s did not hold additional certification to treat glaucoma
Reality Check – August 9 2010 Archives of Internal Medicine
• Do patients know the name of the doctor
overseeing their care?
How many patients know their diagnosis?
• Doctors said
• Patients said
Adverse effects of drugs were discussed with
patients?
• Doctors said
• Patients said
Fears and anxieties
• “At least sometimes I discussed patients’ fears and
anxieties with them” (doctors)
• “I had fears/anxieties but I didn’t discuss them with
my physician.” (patients)
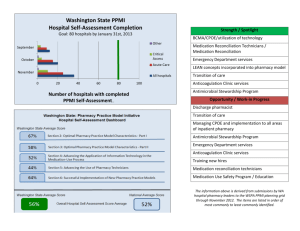
Preventing Medical Errors
Partnership for Patients
• Coalition between 2,900 hospitals and federal
administration
• Goal: Reduce medical errors and save 60,000
lives in three years
Reporting Errors
• 27 states have laws that require hospitals to
report publicly on infections that are developed
in the hospital
• In 2005, only 5 states participated
• Obama administration not proposing new
federal requirements for reporting
What can the patient/consumer do to help reduce
errors?
• Appoint a patient advocate!
•
Verify patient’s identity every time a care provider interacts with
patient
•
Keep a log of doctor and nurse visits and instructions
•
Get results of all tests and labs
•
Write down all information pertinent to diagnosis, treatment, and
care
•
•
ESPECIALLY medications ordered and dispensed
•
Keep a medication log of at-home and hospital-prescribed medications
Infection Control!
What can the patient/consumer do to help reduce
errors?
• Be your own advocate
•
Choose your hospital wisely
•
Most people choose based on doctor’s affiliations, location, or health
plan
•
Big differences in hospitals: Up to a 30% difference in central-line
infections from hospital to hospital
•
INFECTION CONTROL!
What can the patient/consumer do to help reduce
errors?
• Be mindful of your own medications
•
Drug errors are a leading cause of error
•
Bring a list of meds and dosages and keep one with you during
transfers, etc
•
•
Know side effects and potential interactions
Know where your advocate keeps your medication log
What can the patient/consumer do to help reduce errors?
• If you have a choice, choose a hospital using
bar-coding to verify patient identity, medication
instructions, etc.
• If permitted, label everything you can with
patient’s name
What can the patient/consumer do to help
reduce errors?
• Avoid wrong-site surgery
•
Write on your arm/leg/forehead “Operate here”
• INFECTION CONTROL!
•
Make sure everyone touching the patient washes their hands
•
Clean common items in the hospital room such as television
remotes, chair handles, door handles, etc.
•
Do not allow flowers to be near the patient
Hand washing
Video monitoring improved compliance by
40%
2011 study
57
• 63% of health care workers’ uniforms have CFU’s
• 11% multiple antibiotic resistance
• Neckties
Stethoscopes?
58
• 1997 study
• 100% of physicians’ stethoscopes had CFU’s
• Mostly staph, strep
• simple swabbing with alcohol pad reduced growth to
non-pathogenic
• 2011 study of ER workers’ stethoscopes
• 55% had CFU’s
• Mostly staph epi
EEWWWWW
59
• 2010 study
•
Culture-forming units on
•
66% pens
•
55% stethoscopes
•
48% cell phones
•
28% white coats
• 2011 study, U of Iowa
• 119/180 hospital curtains had CFU’s
• 26% MRSA, 44% resistant Enterobacteria
• Takes about a week to contaminate a new
curtain
Coordination of Care
Who is IN CHARGE of your health
care?
Do all doctors/surgeons agree on the
treatment plan?
Who will be responsible for your discharge
instructions?
“Guaranteed” outcomes
• Geisinger Health Systems in Pennsylvania
• Patients pay flat rate up-front
• 90 day guarantee for coronary artery bypass and
other surgeries
• If any avoidable complication occurs within 90
day period, no charge for “remedial care”
• 30-day readmission rate down by 44% since
2006
Bar Coding
• Drugs bar coded in pharmacy based on
electronic health record orders
• Patient wristbands scanned before
administering drugs
• Alarm sounds if mis-match occurs
• Errors cut in half
Improve training
• High-tech simulators
• Change the medical model
• Change the concept of 24-hour shifts
Lesser-known ways to protect yourself
• Don’t get your prescription filled the first week
of the month
•
Deaths due to Rx errors are 25% higher
•
20 year study
• Don’t get sick in July
Time your illness or accident well
• Babies born late at night 16% more likely to die
than those born in the daytime
•
California, 2005, 3.3 million babies
• Patients going into cardiac arrest at night more
likely to die than those having daytime events
Time your illness or accident well
• More medication errors made by hospital
pharmacy at night than during the day
• Kids admitted to pediatric ICU at night were
more likely to die within 48 hours
Lewis Blackman
Lewis Blackman
Safety Act
MAME
Medication Errors
IOM Report July 2006
• “When all types of errors are taken into account,
a hospital patient can expect on average to be
subjected to more than one medication error
each day.”
Massachusetts
• State Board of Registration in Pharmacy
estimates 2.4 million prescriptions are filled
improperly each year in Mass.
Common causes of medication errors
• Incorrect drug administration
• Name confusion
• Lack of appropriate patient education
•
•
•
•
Four times a day
Lid scrubs?
“I’m using that cream, but….”
“I’ve used the whole bottle but I still can’t GO!”
• Language issues
•
•
Antifungal cream:
Apply once every day
Common causes of medication errors
• Wrong diagnosis
• Prescribing errors
•
Illegibility
•
Improper dose (e.g. 5 mg vs 0.5 mg)
• Drug-drug interactions
• Dose miscalculations
Most common underlying causes
• Improper dose (40.9%; most are overdose)
• Wrong drug (19%)
• Wrong route of administration (9.5%)
•
e.g. Otic vs ophthalmic
•
Vosol vs Vexol
Look-alike, Sound-alike
• Lamictal (antiepileptic) vs. Lamisil (antifungal)
• Celebrex, Cerebyx (anticonvulsant), Celexa
(antidepressant)
• Taxol, Taxotere (chemo)
• Serzone (depression) and seroquel
(schizophrenia)
“Grievous Personal Injury”
• Durezol vs. Durasol
•
Salicylic acid wart remover
•
At least one case of blindness
•
•
Suit reportedly $1M against Walgreen’s in NY
Many other “near misses” reported
Look alike, sound alike
• Methadone (opiate dependence) vs Metadate ER
(ADHD)
•
8 year old boy died
Look alike, sound alike
• 4 week old infant
• MD ophthal prescribed tobrex
What happened?
• Tobradex instead of tobrex was dispensed….
• And then Refilled
• Infant developed steroid induced glaucoma
Reducing Medication Errors
WHAT STEPS CAN WE TAKE?
2006 report by IOM: Preventing Medication Errors
• 33% of medication errors are from
•
Naming
•
Labeling
•
Packaging
• Accounted for 30% of medication error deaths
IOM recommendations
• Legibility
• Avoid abbreviations
• Use metric system (not “grains”, e.g.)
• Provide patient age and weight when
appropriate
• Must include drug name, weight or
concentration, and DOSAGE FORM
• Use leading zeros but never trailing zeros
Mind your decimals….
• 0.5 mg NOT .5 mg (leading zero)
• 1 mg
NOT 1.0 mg (trailing zero)
Johns Hopkins University
• 2006 study
• Discharge prescriptions for children requiring
“potent, opioid analgesic drugs” for pain
management
• How many prescriptions contained errors?
Hopkins
• Most common:
•
Missing or wrong patient weight
•
Incomplete dispensing information
• 2.9% with potential to cause significant injury
• All prescriptions studied written by residents and
fellows without oversight or consultation
Hopkins
• CPOE with decision support
• Computerized provider order entry
• Reduced med errors in hospitalized children by
40% - 97%
What about EHR?
March 2010 study, Kaushal et al
• Compared prescribing errors from Sept
2005 through June 2007 for 15
providers who adopted e-prescribing,
and 15 who didn’t
• Nearly 4000 prescriptions reviewed
• Two in 5 handwritten prescriptions had
errors
March 2010 study, Kaushal et al
• Error rates decreased nearly 7-fold with e-Rx
Down from 42.5% to 6.6%
• Error rates remained the same with paper Rx
• 37.3% to 38.4%
• Most errors would not cause serious harm to patients, but
could result in pharmacy
callbacks/delays/nuisances/inconveniences
• Some errors would have been harmful or fatal
•
EHR / HIT positives:
• Legibility issues
• Dosing errors
• Drug-drug interactions
• Contraindications
• “Pick lists” allow extensive prescription
information with a few clicks
EHR potential pitfalls
• “TMI”
•
Important data gets buried
•
Auto-fill even when not appropriate
•
A & O x 3???
•
Patient history obtained from self??
•
Patient denies use of tobacco, alcohol
EHR potential pitfalls
• The “Ignore” Factor
• 75% of physicians admit to ignoring reminder
or alert icons
• More than half never acted on information
presented in alerts/reminders
Six “Rights”
• Right patient
• Right drug
• Right dose
• Right dosage form
• Right route of administration
• Right time
• “Are you allergic to any medications?”