File - Lynette Barnhart BSN, RNC-
advertisement

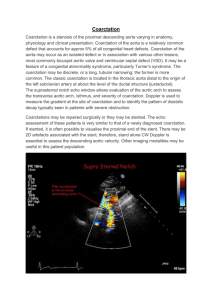
Presented by: Lynette Barnhart RNC, BSN, SNNP June 9, 2014 University of Texas Medical Branch at Galveston NNP Concepts and Practicum II GNRS 5632 Dr. Debra Armentrout PhD, RN, MSN, NNP-BC Dr. Leigh Ann Cates PhD, APRN, NNP-BC,RRT-NPS,CHSE Maternal History Maternal and Fetal Risks and Complications Delivery and Stabilization Admission exam and diagnostics Primary admission diagnoses Etiology and Pathophysiology of Primary Admission Diagnoses Initial Plan of Care Hospital Course by Symptoms Medications Pertinent Theories and Evidence Based Practice Family Interactions Discharge Plan and Follow Up 37 yo, married Hispanic G6 now P5 1 SAB 1994-39 weeks 1997-40 weeks 2004-39 weeks 2009-39 weeks EDD 6/10/14 A+, GBS-, RPR NR, Rubella Immune, HIV NR, HBUnremarkable Medical history Denies alcohol, tobacco, and illicit drug use Advanced maternal age 37 year old U/S 12/16/14 Nuchal thickness of 3.1 Low AFP 12/31/14 + Trisomy 21 U/S 2/28/14 Suspected Coarctation of the aorta Scheduled induction at 39 weeks Due to suspected Coarctation of the aorta Spontaneous labor 38 1/7 weeks GA SROM 2 ½ hours prior to delivery Clear fluid Vertex presentation NSVD No maternal medications prior to delivery Apgars 8 at 1 minute 8 at 5 minutes Delivery summary Lusty cry at delivery, cord clamped and cut. Infant taken to radiant warmer. Dried and stimulated. Infant dusky, BBO2 (40%) provided at 5 minutes of life for preductal saturations below 85%. Continued to dry and stimulate. Improvement in color and saturations noted. O2 discontinued at 8 minutes of life. Infant placed skin to skin with mother prior to transfer to NICU for transition. Gestational age 38 1/7 weeks Measurements Birth weight: 3078gms (10th-50th %tile) Length: 48.5 cm (10th-50th %tile) OFC: 32 cm (10th %tile) Vital signs Temperature 36.9 C Heart rate 120 bpm Respiratory rate 40 br/min Pre-ductal SpO2 94% Post-ductal SpO2 89% Physical Exam General: Habitus of Trisomy 21, No acute distress, active with exam, sucking on pacifier Eye: Normal conjunctiva, bilateral red reflexes. HENT: Normocephalic, nares patent, oral mucosa moist with intact palate, anterior fontanelle soft and flat, ears normally set and rotated, flat facial profile. Respiratory: Unlabored respirations with appropriate chest excursion, lung sounds clear and equal bilaterally. Cardiovascular: Heart rate and rhythm regular without murmur, pulses equal in all four extremities, capillary refill less than 3 seconds, pink with acrocyanosis to hands and feet. Gastrointestinal: Soft, non-tender, non distended with active bowel sounds, no organomegaly, 3 vessel umbilical cord, anus appears patent. Genitourinary: Normal male genitalia for age/gestation, testes descended, void at delivery Lymphatic: Fat pad to nape of neck Musculoskeletal: Moves all extremities, no hip clicks, normal Barlow’s and Ortolani’s. Simian creases to both hands, wide gap between first and second toes. Integumentary: Warm, dry, pink, without rash Neurologic: Alert, moves all extremities appropriately. Echocardiogram 5/28/2014- 1 hour of life FISH chromosomes 5/29/2014- results pending High resolution chromosomes 5/29/2014- results pending Bedside chemstrip 51 @ 1426 (admit) 38.1 week AGA male infant, 3078gms Suspected Coarctation of the aorta Suspected Trisomy 21 Narrowing of the aorta Constricted segment of the aorta that comprises localized medial thickening. 5-8% of all congenital heart defects May also occur with bicuspid aortic valve and VSD (Cates, 2009) Increased afterload on the left ventricle Increased wall stress resulting in ventricular hypertrophy As the PDA closes (may cause rapid CHF and shock) Causes increased left ventricular pressures, increased left atrial pressure, and opening of the foramen ovale Resulting in left-to-right shunting and dilation of the right atrium and right ventricle When the foramen ovale doesn’t open the pulmonary venous and artery pressures increase Resulting in right ventricular dilation (Gholampour, et al., 2006) Clinical findings Systolic ejection murmur that radiates to the apex and is often loudest in the back Xray finidngs Generalized cardiomegaly with normal pulmonary vascular density (Pre-ductal Coarctation) Enlarges left ventricle and left atrium and dilated ascending aorta (Post-ductal Coarctation) Pre-ductal and post-ductal SpO2 saturation discrepancy Upper and lower extremity BP discrepancy Absent or decreased lower extremity pulses Tachypnea Lethargy Poor feeding Shock (Gomella, 2013) Cyanotic lower extremities (Syamasundar, 2012) Medical Treatment Prostaglandin E 0.05-0.15 mcg/kg/min Ventilatory assistance To support increased work of breathing Inotropic drugs Dopamine, Dobutamine, Epinepherine Diuretics Used for infants with CHF Foley Catheter Strict monitoring of urine output and renal perfusion UAC ABGs (Cates, 2009) Surgical Treatment Goal is to bypass the narrowed section of the aorta Left subclavian aortoplasty Resection and end-to-end anastomosis Angioplasty with Dacron patch Stenting Balloon angioplasty (Gholampour, et al, 2004). Down Syndrome Presence of an extra 21st chromosome Most common of all multiple congenital anomaly (MCA) syndromes Occurs in ~ 1 in 650 births Neonatal mortality is related to severe cardiac anomalies Maternal nondisjunction Occurring in the first meiotic division accounts for ~65% of cases Occurring in the second meiotic division accounts for ~23% of cases (Blackburn, 2007) (Gomella, 2013) 1st trimester screening Ultrasound between 10 4/7 and 13 4/7 weeks gestation Measurement of the nuchal translucency (increased in Trisomy 21) Detects 70% of Trisomy 21 2nd trimester screening Serum screening between 15 and 20 6/7 weeks gestation Alpha fetoprotein (AFP), hCG, and unconjugated estriol (Triple Screen) Alpha fetoprotein (AFP), hCG, unconjugated estriol, and inhibin-A (Quad screen) results in 80% detection Decreased AFP, increased hCG, decreased PAPP-A, and increased Inhibin A (Bajaj & Gross, 2011) Physical findings Hypotonia, poor or absent moro reflex, flat facial profile, protruding tongue, up slanting palperbral fissures, Brushfield spots, anomalous auricles, joint hyperextensibility, excess nuchal skin, fifth-digit brachydactyly/clinodactyly, and single transverse palmar crease. Associated Anomalies Congenital heart defects in 40% of infants (most common ASD or VSD), PDA, endocardial cushion defect, aberrant subclavian artery. Hirschsprung disease, duodenal or esphageal atresia, imperforate anus, hearing loss (66%), mental deficiency, and renal and urinary tract (Gomella, 2013) anomalies. (Jones, 2006) Treatment There is no cure for Down’s syndrome Supportive care Early intervention is essential to assist in the progression of developmental milestones. (Heyn & Perlstein, 2014) Admit to NICU, place on continuous cardio/resp monitoring Daily weight, OFC and Length Q Sunday Erythromycin ointment to eyes bilaterally within 1 hour of birth Vitamin K 1mg IM x1 within 1 hour of birth Place PIV Infuse D10W at 10cc/hr (80ml/kg/day) Strict Intake and Output Cardiac ECHO stat to evaluate fetal diagnosis of suspected Coarctation of the Aorta Pre and post-ductal SpO2 monitoring Obtain 4 point Blood pressures Chemstick on admission and then per policy Obtain Metabolic Screen at 24-48 hours Obtain Metabolic screen #2 at 5-10 days of age May breast feed ad lib on demand Social service consult Respiratory: Mild respiratory insufficiency At 3 hours of life infant noted to have frequent desaturations (75-85%) Nasal Cannula started at 1 L @ 21% Discontinued on DOL 1 (24 hours after start) Intermittent nasal stuffiness without increase work of breathing On DOL 4 Treated with little noses Q 4 hours x 24 hours with some improvement No further intervention required Discharged on room air on DOL 6 Pre and post ductal saturation monitoring continued until discharge Respiratory rate 23-77 during stay Cardiovascular: Suspected Coarctation of the Aorta Hemodynamically stable without murmur. Peripheral pulses equal x 4 DOL 0 @ 1 hour of life ECHO obtained Study limited by technical limitations. Atrial level shunt, quantitatively normal biventricular size and systolic function. Ventricular level shunting cannot be excluded. Greater than ½ systemic right ventricular systolic pressures. Tapering of the transverse aorta without evidence of discrete narrowing or stenosis; coarctation cannot be excluded in the presence of a ductus. DOL 1 Pre ductal sats 94-99% Post ductal sats 94-97% Left upper extremity BP 81/45 (58) Left lower extremity BP 70/41 (51) Heart rate 108-138 bpm Cardiovascular continued DOL 2 repeat ECHO Small superior atrial level communication with left-to-right flow. Mild to moderate right heart enlargement as well as right ventricular hypertrophy with normal right ventricular systolic function. Structurally normal-appearing mitral valve with mild mitral regurgitation. Normal left ventricular size and systolic function in the presence of flattened interventricular septal wall motion. Moderate sized patent ductus arteriosus with bidirectional flow. This is a left arch with a common brachiocephalic trunk as the first arch vessel. The transverse aortic arch is diffusely narrowed measuring approximately 3.5mmfor a Z-score of negative 2.5. There is mildly turbulent color low through the transverse aortic arch and there is a peak gradient of 8mmHg in the descending aorta. There does not appear to be a further discrete narrowing of the aortic isthmus. However, cannot completely rule out coarctation in the presence of a PDA. Normal left coronary artery origin. Right coronary artery origin not well visualized. Systemic to supersystemic RV pressure by septal position, TR jet, and PDA flow. DOL 6 Discharge home with parents. Follow up with Cardiologist in 1-2 weeks. FEN/GI: DOL 0 PIV with D10W @ 80ml/kg/day DOL 1 PIV continues @ 80ml/kg/day BF or Similac Advance 20 Infant directed Q 2-4 hours DOL 2 PIV at 117ml/kg/day BF or Similac Advance 20 15cc Q 3 hours Nipple or gavage DOL 3 PIV at 125ml/kg/day BF of Similac Advance 20 15cc Q 3 hours DOL 4 PIV D10W with lytes at 125ml/kg/day BF/EBM/Similac Advance 20 Ad lib minimum 15cc Q 3 hours DOL 5 Discontinue PIV BF/EBM/Similac Advance 20 Ad lib Q 2-4 hours Heme Physiologic Jaundice of the newborn Mother A+, ABS negative Infant blood type unknown At 49 hours-Transcutaneous Bilirubin 12.4 DOL 3 - Total Bilirubin 12.8, Direct 0.2 Bili blanket started DOL 5 - Bili blanket discontinued DOL 6 - Transcutaneous Bilirubin 10.5 Neuro Suspected Trisomy 21 (Intrauterine Diagnosis) DOL 1 –FISH probe sent Confirmed Trisomy 21 DOL 5 DOL 1- High resolution chromosomes sent Pending results at discharge on DOL 6 Discharge Information given on Sharing Down Syndrome AZ Infectious Disease No issues. Mom GBS -, ROM at delivery Vitamin K IM injection, 1 mg x 1 within 1 hour of birth Erythromycin ophthalmic eye ointment to both eyes x 1 within 1 hour of birth D10W @ 10cc/hr (80ml/kg/day) Hepatitis B vaccine 5mcg IM x 1 Little noses Q 4 hours x 24 hours COARCTATION OF THE AORTA Until surgery can be performed PGE is needed. Surgical correction has the lowest risk of restenosis then any other treatment. Although surgical correction reduces the morbidity and mortality rate. These infant’s still have a decreased life expectancy related to poor blood pressure control. Outcome is worse when there is also a hypoplastic arch present. If the ECHO is performed by someone whom is not experienced in neonates and small children a CT or cardiac MRI should be performed to officially adequately assess the aortic arch. Surgical intervention is the preferred method of treatment because those whom have a balloon dilation will almost always need a repeat dilation and/or surgery. (Shah, 2014) (Panzer & Dewolf, 2014) TRISOMY 21 Currently there is no cure for Down’s syndrome. Genetic studies are focuses on finding therapies to improve learning and potential therapies. Early intervention programs, physical therapy, occupational therapy, and speech therapy can improve outcomes. At greater risk for hearing, vision, and learning deficits. Leukemia is more common with Trisomy 21 patients then those without. (Heyn & Perlstein, 2014) Mother and father were concerned immediately after birth, questions answered and plan of care explained. Infant skin to skin with mother prior to transfer to NICU for further evaluation. Father accompanied infant to NICU and further questions answered. After recovery mother visited infant in the NICU, asked appropriate questions regarding suspected Coarctation and Trisomy 21. Discharge home with parents 6/3/14 DOL 6 Diet: EBM/ Similac Advance 20cal/oz ad lib q 2-4 hours 1st Newborn screen sent 5/29 results pending 2nd Newborn screen sent 6/1 results pending ABR hearing screen passed on 6/2/14 Hepatitis B Vaccine given on 6/1/14 Follow up with Primary Care Physician in 2days Follow up with Pediatric Cardiologist in 1-2 weeks Coarctation is a constricted segment of the aorta that comprises localized medial thickening and can be life threatening if not diagnosed and treated. A prenatal diagnosis of Coarctation of the aorta can assist the medical professionals in the preparation for treatment. Trisomy 21 is a genetic defect that may have multiple associated anomalies. Confirmation of a prenatal diagnosis is important to assist the family in the acceptance of a child with a chronic disorder and/or a genetic disorder. Although it is common for a Trisomy 21 infant to have an associated heat defect it is not commonly associated with coarctation of the aorta. Bajaj, K & Gross, S. (2011). Genetic aspects of perinatal disease and prenatal diagnosis. In R. J. Martin, A.A. Fanaroff, & M.C. Walsh. Neonatal-Perinatal medicine: Diseases of the fetus and infant (9th edition pp.129-145). Volume 1. St. Louis, Missouri: Elsevier Mosby Blackburn, S. (2007). Maternal, Fetal, & Neonatal Physiology (3rd edition). St. Louis, Missouri: Saunders Elsevier. Cates, L.A. (2009). The basics about acyanotic heart disease (Powerpoint presentation). Gholampour, D.M., Givtaj, N., Omrani, G.H., Sadeghpour, T.A., & Yaghoobi, A. (2006) Evaluation of results of surgical correction for coarctation of aorta by suclavian flap aortoplasty (SCFA) and other methods in Rajaee Heart Center. Retrieved May 31, 2014, from, http://www.plan.sid.ir/en/ViewPaper.asp?ID=40885&vRadif=17&vWriter=GHOLAMP OUR%20DEHAKI%20M.,GIVTAJ%20NADER,OMRANI%20GH.,SADEGHPOUR%20TABAEI %20A.,YAGHOOBI%20A.&vJournal=RAZI+JOURNAL+OF+MEDICAL+SCIENCES+%28JOU RNAL+OF+IRAN+UNIVERSITY+OF+MEDICAL+SCIENCES%29&vDate=Winter%202006&v Volume=12&vNo=49&vStart=0&vEnd=0 Gomella, T.L. (2013) Neonatology: Management, procedures, on-call problems, diseases, and drugs (7th edition). New York: McGraw Hill Education. Heyn, S.N. & Perlstein, D (2014). Down Syndrom. Retrieved June 6, 2014 , from http://www.onhealth.com/down_syndrome/article.htm Jones, K.L. (2006) Smith’s recognizable patterns of human malformation. (5th edition) Philadelphia, Pennyslvania: Saunders Elsevier. Panzar, J. & Dewolf, D. (2014) Hypertension after Coarctation repair. Retrieved June 6, 2014, from, http://cardiologyacademicpress.com/soap/pdf/delme_427_535c2c62225e71.976001 42.pdf Shah, S. N. (2014). Aortic coarctation treatment & management. Retrieved June 6, 2014, from, http://emedicine.medscape.com/article/150369-overview Syamasundar Rao, P. (2012, February 1) Coarctation of the aorta. Medscape. Retrieved May 31, 2014 from http://emedicine.medscape.com/article/895502overview