Pneumonia - Creighton University
advertisement

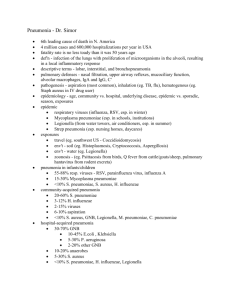
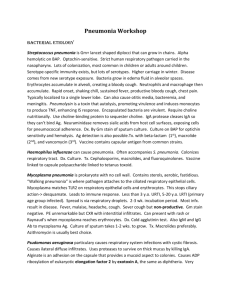
Pneumonia Tammy Wichman MD Assistant Professor of Medicine Pulmonary-Critical Care Creighton University Medical Center The #1 cause of death in the United States from infectious disease is: A. Meningitis B. Pneumonia C. Gastroenteritis D. Urinary Tract Infections E. Toe fungus Pneumonia Most deadly infectious disease in the U.S. 6th leading cause of death Average mortality 14% $20 billion/year in U.S.1 Community acquired pneumonia affects ~4 million patients and results in 10 million physician visits, 1 million hospitalizations, and >50,000 deaths annually 1 File Chest 2004; 125:1888-1901 Defense Mechanisms 80% of cells lining central airways are ciliated, pseudostratified, columnar epithelial cells Each ciliated cell contains about 200 cilia that beat in coordinated waves about 1000x/minute So the lower respiratory tract is normally sterile Pneumonia Pathophysiology Microbial pathogens enter the lung by: Aspiration of organisms from oropharynx More common in patients with impaired level of consciousness: alcoholics, IVDA, seizures, stroke, anesthesia, swallowing disorders, NG tubes, ETT Gram positive and anaerobes: Strep pneumo, H flu, Mycoplasma, Moraxella, Actinomyces Gram negatives: • more likely with hospitalization, debility, alcoholism, DM, and advanced age • Source may be stomach which can become colonized with these organisms with use of H2blockers Inhalation of Infectious Aerosols Hematogenous Dissemination Influenza, Legionella, Psittacosis, Histoplasmosis, TB Staph aureus Fusobacterium infections of the retropharyngeal tissues: Lemierre’s syndrome Direct inoculation and Contiguous Spread Tracheal intubation, stab wounds At the left the alveoli are filled with a neutrophilic exudate that corresponds to the areas of consolidation seen grossly with the bronchopneumonia. This contrasts with the aerated lung on the right of this photomicrograph. What is pneumonia? Infection of the lower respiratory tract Which of the following is NOT a symptom of pneumonia? A. Cough B. Shortness of breath C. Fever D. Abdominal pain E. Chest tightness F. Confusion G. Hot, erythematous 1st toe Clinical presentation Pneumonia should be considered in any patient who has newly acquired respiratory symptoms: cough, sputum production, dyspnea, especially if accompanied by fever and abnormal breath sounds and crackles In elderly or immunocompromised, pneumonia may present with confusion, failure to thrive, worsening of underlying chronic illness, falling Pneumonia Symptoms “Typical” pneumonia: sudden onset of fever, cough productive of purulent sputum, pleuritic chest pain “Atypical”: gradual onset, dry cough, prominence of extrapulmonary symptoms: headache, myalgias, fatigue, sore throat, nausea, vomiting Includes diverse entities and has limited clinical value Pneumonia Which of the following is NOT a sign of pneumonia? A. Dullness to percussion B. Tracheal deviation C. Bronchial breath sounds D. Egophany, increased tactile fremitus E. Late inspiratory crackles Pneumonia Diagnosis Radiography: CXR confirm the presence and location of the pulmonary infiltrate assess the extent of the infection detect pleural involvement, pulmonary cavitation, or lymphadenopathy May be normal when the patient is unable to mount an inflammatory response (immunocompromised) or is in the early stage of an infiltrative process (hematogenous S. aureus pneumonia) A 64 year old female with DM and HTN is admitted to 4600 with RLL pneumonia. T 39.3 HR 118 R 28 BP 110/60 Sats 92% on 4 L NC. She has crackles in her RLL. You should: A. Order a sputum gram stain and culture. Wait for the results before ordering antibiotics. B. Order a sputum gram stain and culture. Empirically start Ceftriaxone and Azithromycin. C. Order a sputum gram stain and culture. Empirically start Vancomycin and Zosyn. D. Start Ceftriaxone and Azithromycin. Pneumonia Diagnosis Sputum gram stain and culture: Controversial: no rapid, easily done, accurate, cost-effective method to allow immediate results Expectorated sputum is frequently contaminated by oropharyngeal flora Low power magnification to assess squamous epithelial cells Culture and sensitivity are only accurate if there are <10 epi’s per low power field Best results if the specimen contains >25 WBCs per LPF If patient has a productive cough, send sputum for gram stain and culture: could be of use in directing treatment if patient fails to respond to empiric therapy Same patient. What other tests do you want? Blood cultures. Urine cultures. Urine for Legionella antigen. Urine for pneumococcal antigen. Urine for chlamydia antigen. HIV test. Bronchoscopy with culture of respiratory secretions. Pneumonia Diagnosis Blood cultures are positive in 11% of patients with CAP, more commonly in patients with severe illness Urine antigen assays for L pneumophila serogroup 1 can be done easily and rapidly. Sensitivity 70% Specificity >90% Assay for pneumococcal urinary antigen : sensitivity 50-80% and specificity 90% Responsible pathogen is not defined in as many as 50% of patients In February, a 55yo F with rheumatoid arthritis and chronic bronchitis presents to the office with a cough productive of green sputum, a fever and generalized myalgias x 2 days. T 101.6 HR 110 R 24 BP 125/80. On exam, she has crackles in her LLL and dullness to percussion. You should A. Give her a presciption for Azithromycin B. Check her O2 sats and order a CXR C. Check her for Influenzae A D. Order a CBC, BMP, LFTs E. A, B, and C F. B, C, and D G. B and C Pneumonia Diagnosis Routine laboratory tests: CBC, electrolytes, hepatic enzymes) are of little value in determining the etiology of pneumonia, but may have prognostic significance and influence the decision to hospitalization. Should be considered in patients who may need hospitalization, >65 yr, or with coexisting illness. All admitted patients should have oxygen saturation assessed by oximetry Pneumonia Diagnosis Invasive testing: percutaneous transthoracic needle aspiration or bronchoscopy are not routinely recommended. May be helpful in: • immunocompromised hosts • suspected tuberculosis in the absence of productive cough • non-resolving pneumonia • pneumonia associated with suspected neoplasm or foreign body • suspected Pneumocystis carinii Which of the following findings would indicate an increased risk of death in patients with community-acquired pneumonia? A. BUN <8 mmol/L B. Diastolic blood pressure >70 mm Hg C. Respiratory rate >30 breaths per minute D. Unilobar lung infiltrate E. PO2 = 65 mm Hg while breathing room air Pneumonia Severity Index Pneumonia Severity Index Site of Treatment Class I or II: Outpatient treatment Class III: Potential outpatient or brief inpatient observation Class IV and V: Inpatient Physician decision making: medical and psychosocial comorbidities, ability to take po, substance abuse, ability to do ADLs CURB 65 Confusion Urea level (>19) Respiratory rate (>30) Blood Pressure SBP< 90 or DBP <60 Age Excellent indicator for mortality All of the following are reasons to admit a patient with pneumonia to the ICU EXCEPT: A. Need for mechanical ventilation B. Shock requiring pressors C. High WBC count with bandemia D. Decreased urine output ICU Admission Minor Criteria RR>30/min PaO2/FiO2 <250 Multilobar pneumonia Systolic BP <90 Diastolic BP <60 Major Criteria Need for mechanical ventilation Increase in the size of infiltrates by >50% within 48hrs Septic shock Acute renal failure (uop <80ml in 4 h or serum Cr>2.0) In April, a 45yo F with HTN presents to the office with fever x 3 days and a cough. T 102.5 HR 95 R 22 BP 130/80 Sats 94% on RA. CXR shows RUL infiltrate. A. You should check a CBC, BMP, and LFTs and consider admitting her based on the results B. You should admit her for 24 hour observation C. You should check for Influenzae A D. The most likely organisms are Strep pneumonia, Mycoplasma, Chlamydia, and H. flu and she should be treated with Azithromycin or Doxycycline Group I: Outpatients No cardiopulmonary disease No modifying factors Organism: Streptococcus pneumonia Mycoplasma pneumonia Chlamydia pneumonia Hemophilus influenzae Miscellaneous Legionella Mycobacterium Fungi Treatment: Advanced generation macrolide(azithromycin or clarithromycin) OR doxycycline All of the following have been identified as risk factors for community-acquired Legionella pneumonia EXCEPT: A. Cigarette smoking B. Chronic pulmonary disease C. Acquired immunodeficiency syndrome D. Advanced age E. Chronic illness, including diabetes, liver disease, and renal disease A 68 yo M with DM, HTN, CAD, is admitted to the hospital with community acquired pneumonia. He is recently retired from the insurance industry and has been caring for his grandson several mornings a week. He doesn’t smoke but he does drink 2-3 cocktails every night. T 101.6 HR 85 R 22 BP 95/60 Sats 92% on 3L NC. CXR shows an infiltrate in the lingula. He is at risk for A. Penicillin resistant pneumococus B. Pseudomonas C. MRSA D. Enteric gram negatives Modifying Factors that Increase the Risk of infection with Specific Pathogens Penicillin-resistant pneumococci Enteric gram negatives Age >65 B-lactam therapy within the past 3 months Alcoholism Immune suppressive illness (including tx with corticosteroids) Multiple medical comorbidities: DM, CRI, CHF, CAD, malignancy, chronic liver disease Exposure to a child in a day care center Residence in a nursing home Underlying cardiopulmonary disease Multiple medical comorbidities Recent antibiotic therapy Pseudomonas aeruginosa Structural lung disease (bronchiectasis) Corticosteroid therapy (>10mg prednisone/day) Broad spectrum antibiotic therapy for > 7 days in past month Malnutrition The mortality rate for patients with nursing home-acquired pneumonia is: A. 10% B. 20% C. 40% D. 60% E. 80% Group II: Outpatient, with cardiopulmonary disease, and/or other modifying factors Organism: Strep pneumonia Mycoplasma Chlamydia Mixed infection Hemophilus influenzae Enteric gram-negatives Viruses Miscellaneous Moraxella, Legionella, anaerobes, TB, fungi Therapy: B -lactam (oral cefpodoxime, cefuroxime, high-dose amoxicillin, amoxicillin/clavulanate or parenteral ceftriaxone PLUS Macrolide or doxycycline OR Antipneumococcal fluoroquinolone Group III: Inpatients Organism Strep pneumonia Hemophilus influenzae Mycoplasma Chlamydia Mixed infection Enteric gram-negatives Aspiration Virus Miscellaneous Therapy: 1. Intravenous B -lactam: cefotaxime, ceftriaxone, ampicillin/sulbactam, high-dose amipicillin PLUS Intravenous or oral macrolide or doxycycline OR 2. Antipneumococcal fluoroquinolone A 45 year old female with lupus is admitted to the ICU with community acquired pneumonia and septic shock. She was intubated in the ER due to hypoxemic respiratory failure. Currently, T 102 HR 125 R 28 BP 90/60 on Dopamine. She should be started on: A. Vancomycin and Zosyn B. Levofloxacin C. Ceftriaxone and Levofloxacin D. Doxycycline and Gentamicin ICU Patients Organisms: Strep pneumonia Legionella Hemophilus influenzae Enteric gram-negative bacilli Staphylococcus aureus Mycoplasma Respiratory Viruses Miscellaneous Therapy: 1. Intravenous B -lactam: cefotaxime, ceftriaxone, ampicillin/sulbactam, high-dose amipicillin PLUS either Intravenous or oral macrolide or doxycycline or Antipneumococcal fluoroquinolone ICU Patients with Risks for Pseudomonas aeruginosa 1. Selected iv antipseudomonal B -lactam (cefepime, imipenem, meropenem, piperacillin/tazobactam) PLUS iv antipseudomonal quinolone OR 2. Selected iv antipseudomonal B -lactam PLUS iv aminoglycoside PLUS either iv macrolide or iv nonpseudomonal fluoroquinolone The organism(s) most commonly found in patients with nosocomial pneumonia is (are): A. Aerobic Gram-negative rods B. Staphylococcus aureus C. Legionella species D. Streptococcus pneumoniae E. Haemophilus influenzae Hospital-Acquired Pneumonia Enteric aerobic gram negative bacilli Pseudomonas aeruginosa Staphylococcus aureus Oral anaerobes Antipseudomonal cephalosporin (cefepime, ceftazidime) OR Antipseudomonal carbepenem OR B lactam/B -lactamase inhibitor PLUS Antipseudomonal fluoroquinolone OR aminoglycoside PLUS Vancomycin or Linezolid The mechanism thought to account for most cases of nosocomial pneumonia includes: A. Inhalation of infected aerosols from respiratory equipment B. Hematogenous spread from another infected site outside the lung C. Spread from a contiguous infected site D. Aspiration of pathogen-laden oropharyngeal secretions E. Inhalation of infected droplet nuclei from other patients in the area Which of the following has been demonstrated to reduce the incidence of nosocomial pneumonia? A. Nasogastric tubes B. Enteral feedings C. Hand washing D. Isolation of patients with pneumonia E. Antacids Metastasis to skin and CNS Hyponatremia, AMS, renal and hepatic dysfunction Night sweats, weight loss Erythema multiforme, hemolytic anemia, encephalitis, transverse myelitis Erythema nodosum Increased risk after Influenzae pneumonia Staph aureus Histoplasma Legionella Mycoplasma Nocardia TB The organism most commonly associated with life-threatening community acquired pneumonia is: A. Streptococcus pneumoniae B. Legionella pneumophila C. Klebsiella pneumoniae D. Pseudomonas aeruginosa E. Staphylococcus aureus Strep pneumonia Encapsulated lancet shaped diplococcus Causes up to 50% of community acquired pneumonia Patients present with acute onset of hard, shaking chills and pleuritic chest pain Usually have high WBC, however may have very low WBC if overwhelming infection Sputum may be rusty colored CXR often shows lobar consolidation If bacteremic, mortality is 30% Drug Resistant Strep pneumonia Prevalence continues to increase worldwide: PCN resistant 18-22% macrolide resistant 24-32% Patients with high level resistance (penicillin MCI >4mg/mL) showed an increased risk of suppurative complications Most common mechanisms of resistance to macrolides are methylation of a ribosomal target encoded by erm gene and efflux of the macrolides by cell membrane protein transporter, encoded by mef gene Predicting Antimicrobial Resistance in Invasive Pneumococcal Infections Clinical Infectious Diseases 2005;40:1288-97 3339 patients Risk factors for penicillin-resistance or macrolide resistance: antibiotic use (PCN, TMP-SMX, and azithro) in last 3 months Risk factors for fluoroquinolone resistance: previous use of fluoroquinolones, residence in a NH; nosocomial acquisition Percentage of Pneumococcal Isolates That Were Nonsusceptible to Various Antibiotics from Children under Two Years of Age (Panel A) and Adults 65 Years of Age or Older (Panel B) with Invasive Disease, 1999 to 2004 Kyaw, M. H. et al. N Engl J Med 2006;354:1455-1463 Clinical Course Target time for appropriate initiation of antimicrobials within 4 hours of admission Fever x 2-4 days Leukocytosis usually resolves by Day 4 Abnormal physical findings (crackles) persist beyond 7 d in 20-40% CXR clears by 4 weeks in 60% patients Delayed resolution with increasing age, multiple coexisting illness, alcoholism, bacteremia When to switch to oral therapy Oral = iv: doxycycline, linezolid, quinolones Improvement in cough and dyspnea Afebrile WBC decreasing Functioning GI tract Patient can be discharged home the same day that clinical stability occurs and oral therapy is initiated. Prevention Recommendations by CDC: Pneumococcal vaccine: age >65 or if chronically ill: CHF, COPD, DM, ETOH, cirrhosis, asplenia, long-term care facilities. Revaccinate after 5 years. Influenzae vaccine: age >65, residents of long-term care facilities, chronic pulmonary or cardiovascular disease, hospitalization in the preceding year, immunosuppression, pregnant women in 2nd or 3rd trimester during flu season Patients should be counseled during hospitalization regarding smoking cessation Annual Incidence of Invasive Disease Caused by Penicillin-Susceptible and PenicillinNonsusceptible Pneumococci among Children under Two Years of Age, 1996 to 2004 Kyaw, M. H. et al. N Engl J Med 2006;354:1455-1463 Annual Incidence of Invasive Disease Caused by Penicillin-Nonsusceptible Pneumococci in Persons Two Years of Age or Older, 1996 to 2004 Kyaw, M. H. et al. N Engl J Med 2006;354:1455-1463 In immunocompetent adults for whom the pneumococcal vaccine is indicated, the protection efficacy is: A. 0% B. 10% C. 30% D. 60% E. 80% A 34yo F with JRA presents to the office with a 3 day history of a cough productive of yellow sputum, fever, and myalgias. On physical exam, she is mildly tachypneic but not in distress T 104 HR 115 R 28 BP 105/60 Saturations 94% RA. Physical exam reveals rales in her LLL. She has dullness to percussion at her left base and increased tactile fremitus. The next step in her management is: A. Sputum gram stain B. Chest radiograph C. Give her a prescription for Augmentin D. Admit her to the hospital What A. B. C. D. E. should she be treated with? Vancomycin and Imepenem Keflex Azithromycin Ceftriaxone Levofloxacin A 55yo with CHF presents to the ER with a 1 day history of cough, fever, shaking chills, and weakness. She is obviously uncomfortable, with mildly increased work of breathing. T 100.8 HR 125 R 32 BP 100/55 Saturations 86% on RA. Lungs have crackles in her right upper lobe. She has 1+ edema bilaterally. She is alert and oriented. You should now obtain all of the following labs EXCEPT: A. CBC B. Electrolytes C. PT, PTT D. ABG E. Sputum culture F. Blood cultures ABG: pH 7.36 pCO2 42 pO2 50 Na 134 K 4.3 Cl 95 HCO3 20 BUN 42 Cr 1.4 glucose 145 WBC 18.3 Hgb 10.3 Hct 32 Plt 130 She should be: A. Given a prescription for Azithromycin and sent home B. Admitted to the hospital. Start Ceftriaxone and Azithromycin after she coughs up a sputum sample. C. Admitted to the hospital. Start Levofloxacin immediately D. Admitted to the ICU and started on mechanical ventilation PORT Score Age 55-10=45 CHF +10 RR +20 HR 124 +10 BUN +20 pO2 +10 115 Class IV Mortality 8-9% A 70yo F resident of a nursing home is evaluated in the ER due to decreased mental status and hypothermia. She has a history of stroke and is currently taking only aspirin. She has been able to eat on her own and there have been no witnessed aspirations. She has not been treated recently with antibiotics. WBC 12 Hgb 12 Electrolytes are normal and she has mild chronic renal insufficiency. CXR shows small interstitial infiltrate in RLL. She receives empiric treatment for communityacquired pneumonia. Therapy for which of the following should also be considered? A. Pseudomonas aeruginosa B. Anaerobic bacteria C. Enteric gram-negative organisms D. Aspergillus fumigatus E. Mycobacterium tuberculosis A 28yo M presents to the ER with increasing shortness of breath and subjective fever and chills. In the ER, patient is in moderate respiratory distress. T 102 HR 140 R 38 BP 85/55 Sats 80% on RA. Lungs have rales throughout. He has no peripheral edema. He knows his name and knows he is in the ER but he is unsure of the date (thinks it is 2003). You should do all of the following EXCEPT: A. Start IVF wide open B. Get an ABG C. Wait on ABG before starting oxygen D. Order a CXR E. Admit to the ICU In carefully performed prospective studies on the etiology of community-acquired pneumonia, the organism most often identified in patients ill enough to require hospitalization is: A. Streptococcus pneumoniae B. Unknown C. Chlamydia pneumoniae D. Mycoplasma pneumoniae E. Haemophilus influenzae In patients with bacteremic pneumonia the organism most likely to be found is: A. Staphylococcus aureus B. Klebsiella pneumoniae C. Haemophilus influenzae D. Streptococcus pneumoniae E. Pseudomonas aeruginosa A 65 yo M develops bilateral lower lobe pneumonia and is treated as an outpatient with amoxicillin/clavulanic acid for 72hours. Despite this treatment, he deteriorates and is admitted to the hospital. Within 12 hours of admission, he develops respiratory failure requiring admission to the ICU, intubation, and mechanical ventilation. The organism most likely to account for the severity of disease despite treatment with Augmentin is: A. Moraxella catarrhalis B. Chlamydia pneumoniae C. Klebsiella pneumoniae D. Legionella pneumophila E. Streptococcus pneumoniae Pneumonia Common infection Pathophysiology Clinical presentation Risk factors for mortality Treatment