African Americans
advertisement

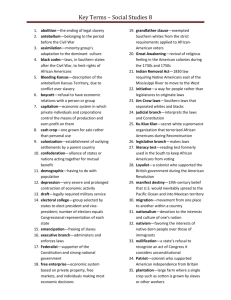
Factors associated with racial disparities in maternal-infant bed-sharing: Findings from Wisconsin Trina C. Salm Ward, PhD, MSW1,2,3; Emmanuel Ngui, DrPH, MSc2;4; Mary K. Madsen, PhD, RN3; Ron A. Cisler, PhD2,3,4 1The University of Georgia School of Social Work and the College of Public Health; 2Center for Urban Population Health; 3University of Wisconsin-Milwaukee College of Health Sciences; 4University of Wisconsin-Milwaukee Joseph J. Zilber School of Public Health BACKGROUND • Bed-sharing is associated with an increased risk of sleep-related infant deaths.2 • Disproportionately higher rates of sleep-related infant deaths occur for African Americans.3 • “Separate but proximate sleep surface” for infants recommended by 1 American Academy of Pediatrics (AAP). • Maternal-infant bed-sharing remains a common practice, especially among African Americans. Table 1: Distribution of Characteristics by Bed-Sharing for Non-Hispanic African Americans and Whites Table 2: Logistic Regression Results for Bed-Sharing for Non-Hispanic African Americans and Whites Study Purpose To examine factors associated with bed-sharing among African American and White mothers in Wisconsin. METHODS • Data: Wisconsin Pregnancy Risk Assessment Monitoring System (PRAMS) dataset (2007-2010). o Stratified sample of linked survey and birth certificate data. o N = 2,486 (806 non-Hispanic African Americans; 1,680 non-Hispanic Whites). • Bed-sharing: “How often does your new baby sleep in the same bed as you or anyone else?” o Yes: “Always,” “Often,” “Sometimes,” “Rarely” o No: “Never” • Separate logistic regression models run for African Americans and Whites using weight variable. • Review by UW-Milwaukee and UGA Institutional Review Boards. Source: http://www.dhs.wisconsin.gov/births/prams/ RESULTS • Overall, more African Americans (70.6%) bed-shared than Whites (53.4%), p < 0.001. • As show in Table 1: o African Americans: Higher proportion of bed-sharing mothers had >12 years of education, did not use Medicaid, and experienced partner-related stress. o Whites: Higher proportion of bed-sharing mothers experienced abuse, breastfed, earned <$50,000, were unmarried, had <16 years of education, used Medicaid for delivery, experienced emotional, financial, partner-related, and traumatic stress, and placed infants non-supine to sleep. o Both groups: Significant differences between non-bed-sharing and bed-sharing sub-groups. • Logistic regression (Table 2): o African Americans: Partner stress and education >12 years associated with significantly greater odds of bed-sharing. o Whites: Partner stress, breastfeeding, earning $35,000-$49,999, being unmarried, needing money for food, and placing infant nonsupine to sleep significantly associated with increased odds of bed-sharing. o Both groups: Partner-related stress significantly associated with bed-sharing, but no significant difference between groups. CONCLUSIONS DISCUSSION • Study found significant racial differences in factors associated with bed-sharing. • Findings suggest that for: o African Americans, higher education had greater odds of bedsharing; other socio-economic factors (income, insurance status, money for food, financial stress) were not significant. o Whites, bed-sharing appears more strongly linked to socioeconomic factors and stress; non-supine sleep combined with bed-sharing is a particularly high-risk sub-group. • Partner-related stress: Bed-sharing might interfere with partner intimacy or be a result of partner stress (e.g., separation). Limitations • Reasons for bed-sharing not included in Wisconsin PRAMS. • Bed-sharing question refers to “bed” only. • Potential for under-reporting. Findings suggest the need: • For more research on context and reasons for bed-sharing: o Sources of information about infant sleep. o Decision-making process about sleep location (influences on decisions and how risks and benefits are weighed). • To engage fathers/partners in bed-sharing discussions and in the postnatal period.4 • To tailor culturally-salient safe sleep interventions to subpopulations at higher risk of sleep-related infant death. • When speaking with families, providers should: o Discuss specific context of infant sleep (environment, motivations and reasons). o Working within that context, help family increase safety of infant’s sleep environment (for example, sharing AAP recommendations).5 References 1 American Academy of Pediatrics (AAP). The changing concept of Sudden Infant Death Syndrome (SIDS): Diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider. Pediatrics. 2005;116(5):1245-55. 2Carpenter R, et al. Bed-sharing when parents do not smoke: Is there a risk of SIDS? An individual level analysis of five case-control studies. BMJ Open. 2013;3(5):e002299. 3Mathews TJ, MacDorman MF. Infant mortality statistics from the 2009 linked birth/infant death data set. NVSR. 2013;61(8). 4Alio AP, Mbah AK, Kornosky JL, Wathington D, Marty PJ, Salihu HM. Assessing the impact of paternal involvement on racial/ethnic disparities in infant mortality rates. J Community Health. 2011;36(1):63-8. 5AAP. SIDS and other sleep-related infant deaths: Expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011;128(5):1030-9. Acknowledgements We gratefully acknowledge Wisconsin PRAMS mothers; Jennifer Doering, PhD, RN and Paul Florsheim, PhD (Dissertation Committee Members); the Center for Urban Population Health; a Dissertation Grant from the College of Health Sciences, University of Wisconsin-Milwaukee; and statistical support from the University of Georgia Statistical Consulting Center. Wisconsin Pregnancy Risk Assessment Monitoring System (PRAMS) data were collected and provided by the PRAMS Project in the Division of Public Health, Wisconsin Department of Health Services. The Centers for Disease Control and Prevention Cooperative Agreement grant number UR6/DP000492 provided funding for data collection and some staff support. The PRAMS Working Group is also acknowledged.