Nutrition Therapy for Clients with Disordered Eating
advertisement

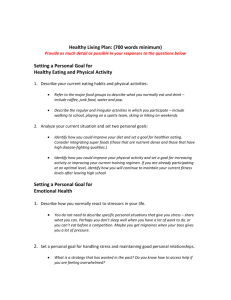
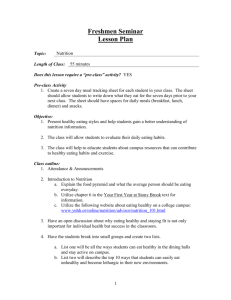
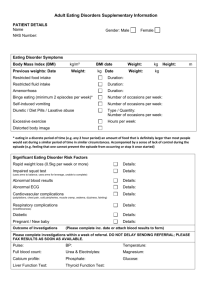
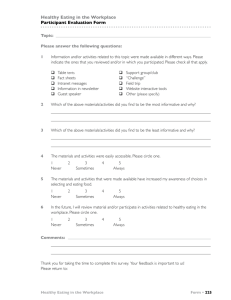
Nutrition Therapy for Clients with Disordered Eating By: Megan Holt, MPH, RD REVIEW OF ED CRITERIA for AN (DSM-IV) Refusal to maintain body weight at or above a minimally normal weight for age and height (or failure to make expected weight gain during period of growth) Intense fear of gaining weight or becoming fat, even though underweight. Disturbance in the way in which one's body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or denial of the seriousness of the current low body weight. In postmenarchal females, amenorrhea ie, the absence of at least three consecutive cycles. (A woman is considered to have amenorrhea if her periods occur only following hormone administration.) Specify type: Restricting Type: During the current episode of AN, the person has not regularly engaged in binge-eating or purging behavior Binge-Eating/Purging Type: During the current episode of AN, the person has regularly engaged in binge-eating or purging behavior REVIEW OF ED CRITERIA for BN (DSM-IV) Recurrent episodes of binge eating characterized by both of the following:(1) Eating, in a discrete period of time (eg, within any 2-hour period), an amount of food that is larger than most would eat during a similar period of time and under similar circumstances.(2) A sense of lack of control over eating during the episode Recurrent inappropriate compensatory behavior in order to prevent weight gain, such as self-induced vomiting, misuse of laxatives, diuretics, enemas or other medications, fasting or excessive exercise. The binge eating and compensatory behaviors both occur, on average, at least twice/week for 3 months. Self-evaluation is unduly influenced by body shape and weight. The disturbance does not occur exclusively during episodes of AN. Specify type: Purging type: During the current episode of BN, the person has regularly engaged in self-induced vomiting or the misuse of laxatives, diuretics or enemas. Nonpurging type: During the current episode of BN, the person has used inappropriate compensatory behaviors, such as fasting or excessive exercise, but has not regularly engaged in self-induced vomiting or the misuse of laxatives, diuretics or enemas. REVIEW OF ED CRITERIA for ED-NOS (DSM-IV) For females, all AN criteria are met except that the individual has regular menses. All AN criteria are met except that, despite significant weight loss the current weight is in the normal range. All BN criteria are met except that the binge eating and inappropriate compensatory mechanisms occur at a frequency of less than twice a week or for duration of less than 3 months. The regular use of inappropriate compensatory behavior by an individual of normal body weight after eating small amounts of food (eg, selfinduced vomiting after the consumption of two cookies). Repeatedly chewing and spitting out, but not swallowing, large amounts of food. Binge-eating disorder (falls under DSM-IV for now): recurrent episodes of binge eating in the absence of inappropriate compensatory behaviors characteristic of BN. AN: Pathophysiology Depleted fat stores; muscle wasting Amenorrhea Cheilosis Postural hypotension; dehydration or edema Sleep disturbances Low body temperature/cold intolerance Lower metabolism: low thyroid hormone Bone marrow hypoplasia (50% of AN patients) results in leukopenia, anemia, thrombocytopenia Iron deficiency anemia Increased infections Dry skin, hair and hair loss Yellow skin due to hypercarotenemia Lanugo: fine body hairs AN: Pathophysiology T-Score Osteopenia/Osteoporosis Reduced bone mineral density May result in vertebral compression, fractures Caused by estrogen deficiency, elevated glucocorticoid levels, malnutrition, reduced body mass Affects males and females AN: Pathophysiology GI Bloating, abnormal fullness after eating Constipation Diarrhea Digestive enzymes low (i.e. lactase) AN: Pathophysiology Cardiovascular Decreased heart rate <60 bpm Decreased blood pressure <70 mm/Hg systolic; orthostatic hypotension Reduction in heart mass Mitral valve prolapse related to hypovolemia or cardiomyopathy Fatigue, fainting Death from CHF Electrolyte imbalance → heart failure, death Low intake potassium Loss in vomiting, diuretics Refeeding syndrome: electrolyte imbalances caused by rapid refeeding BN: Pathophysiology Vomiting Dehydration Alkalosis Hypokalemia (low potassium) Sore throat, esophagitis, mild hematemesis Abdominal pain Subconjunctival hemorrhage Esophageal tears/ruptures (rare) Acute gastric dilatation or rupture Salivary gland infections Cardiac arrhythmias related to electrolyte and acid-base imbalance caused by vomiting, laxative, and diuretic abuse Ipecac may cause irreversible myocardial damage and sudden death Menstrual irregularities BN: Pathophysiology Laxative Abuse Dehydration Elevation of serum aldosterone and vasopressin levels Rectal bleeding Intestinal atony Abdominal cramps Diuretic Abuse Dehydration Hypokalemia Role of the dietitian in a treatment team and goals of nutrition therapy AN: weight gain/prevention of further loss and correction of malnutrition induced disorders; normalization of eating patterns and behaviors BN: weight maintenance in the short term even if patient is overweight until eating habits are stabilized Increase food intake to raise the BMR (basal metabolic rate) Some weight restoration and treatment of malnutrition may make psychotherapy more effective due to improved cognition (Nutritional intervention must support psychological strategy) Role of the dietitian in a treatment team and goals of nutrition therapy Often require hospitalization to begin refeeding Some require enteral feedings, but most can be rehabbed with oral feedings Goal is increase in energy intake with weight gain Energy intake must be increased gradually while minimizing caloric expenditure Hospitalized patients: goal is 2-3 lb/week Outpatients: 1 pound/week (APA Practice Guidelines for the Treatment of Eating Disorders, January, 2006) Part I: Nutrition Assessment Calories compared with DRI (dietary reference intake) Evaluate macronutrient mix (carbohydrate, protein, fat) Evaluate micronutrient intake compared with DRI Estimate fluids and compare with needs Evaluate alcohol, caffeine, drugs, dietary supplements (www.usda.gov) for DRI’s (The Eating Disorders Clinical Pocket Guide by Jessica Setnick) Nutrition Assessment Pertinent medical history Ex: diabetes, hypertension, high cholesterol, kidney disease, etc . Pertinent family history (parents, siblings) ED, heart disease, etc. Eating habits, weight and stature, relationship with food Nutrition Assessment Height (verify- particularly in adolescents) ED history bingeing, purging, relationship with food/shape/exercise Weight history lifetime highest, lowest during ED Conditions around extreme weights Nutrition Assessment Current ED behaviors How often does the client weight at home? Binge Purge (33-75% kcals still absorbed) Fluid intake (caffeinated and decaf) Food Rituals Eating foods in certain orders (ex: veggies first) Excessive chewing (or counting chews) Rearranging food on a plate (ex: 8 peas) Eating finger foods with fork and knife Wiping fork after each use Not allowing foods to touch One food per meal (ex: blueberries) Nutrition Assessment Medical changes related to ED Constipation, diarrhea, lactose intolerance, dental problems, bone health? Last period and when stopped if amenorrhea Medications and supplements BCP, calcium, MVI, herbal supplements, miralax, etc. Nutrition Assessment Methods to suppress hunger Gum, diet soda/products, coffee, condiments Vegetarianism How long? Does this coincide with start of ED? Honoring vegetarianism and level of care (later) Food Allergies? Gluten Lactose Other? Nutrition Assessment Blood values and nutritional significance: Albumin Total protein Blood Urea Nitrogen (BUN) Creatinine Mangnesium Phosphorus Sodium Potassium Hemoglobin/Hematocrit Estradiol Frequency of blood draws? Food Journal (see sample food journal) Keeps for three days prior to visit Continues until eating and B/P stable More useful with clients that are new to treatment/little knowledge of nutrition No judgment!!!! Plan of Care MVI/Supplement recommendations Calcium: Needs 1200mg/day Supplementation: 500-1000mg/day Calcium Carbonate most common MVI with Vitamin D Plan of Care MVI/Supplement recommendations Iron: Needs 15-18mg/day Supplementation: 50-60mg twice daily Frequent complaints: constipation, nausea Vitamin C, meat protein (heme iron) increases absorption Caffeine and phytates inhibit absorption Other supplements per MD (ex: B12) What’s wrong with this picture? Break up into groups Look at the 3 different sample menus How would you make this day more balanced? Mindful Eating! Synonymous words: Intuitive eating Conscious eating Thoughtful eating Characteristics of: Being connected and present Awareness Respecting body Being in-tune with physical hunger and fullness cues Being non-judgmental Mindful Eating Practice Take your time (slow down!) Use timer Put utensils down Push plate away Use your 4 senses Limit distractions Set environment to be calm Meditation or prayer Body Cues How to distinguish between emotional and physical hunger and fullness Use Hunger Scale (on food journal) Use inquiry When did I eat last? Did I have a balanced meal or snack? Was I fully satisfied when I finished? Are there any particular emotions present? Part II:Meal Planning Estimating needs for AN 30-40 kcals/kg body weight (1200-1600kcals daily to start) 200-300 kcal increases 2 times weekly 70-100 kcals/kg ultimately, with weight restoration goal of 1-2 lbs weekly (outpatient) or 2-3 lbs weekly (inpatient) Fluids 30-40ml/kg body weight or 64oz (APA Practice Guidelines for Treatment of ED’s 2006) Determining Goal Weight CDC Growth Charts (adolescents) http://www.cdc.gov/GROWTHCHARTS/ Hamwi Equation: Hamwi Formula for Men 106 lbs for first 5 feet + 6 lbs for each inch over 5 feet (med. frame) Small frame (- 10%), Large frame (+ 10%) Hamwi Formula for Women 100 lbs for first 5 feet + 5 lbs for each inch over 5 feet (med. frame) Small frame (- 10%), Large frame (+ 10%) Past History/ menstruation Genetics: parents build and eating habits Meal Planning-AN 3 meals and 3 snacks Liquids and use of supplements May need reglan due to delayed gastric emptying for comfort Meal Planning-BN Estimating needs for BN: 25-35 kcals/kg body weight, depending on current intake and exercise Primary goal: interuption of B/P Initial prescription typically around 1500 kcals Adjust for weight maintenance, and avoid weight reduction diet until eating is stable Expect impairment of hunger/satiety signals Ex: 5 ft 4 in., 128 lbs (58kg)=1450-2030 kcals (APA Practice Guidelines for Treatment of ED’s 2006) Meal Planning: Macronutrients 50-55% carbohydrate (25-30g fiber) 15-20% protein (0.8-1.0g/kg body wt) 25-30% fat (less than 10% total kcals from saturated/trans fatty acids) www.mypyramid.gov www.eatright.org www.americanheart.org Exchange System Exchanges versus Calories More flexible than Calorie counting Emphasizes balance and moderation Incorporates evidence based suggestions for macronutrients from ADA and AHA www.diabetes.org Exchange System Grains/Starches 6-11 Milk/Dairy 3-4 Fruit 2-4 Vegetables 3-5 Protein/Meat 4-6 Fats 4-6 Above guidelines may not be adequate for weight restoration!! See sample exchange lists Exchange System Starches/Grains: 15g Carb, 3g protein, 0-1g fat, 80 kcals Dairy/Milk: 12g Carb, 8g protein, 0-3g fat, 100 kcals Fruit: 15g Carb, 0g fat/protein, 60 kcals Veggies: 5g Carb, 0-2g protein, 0g fat, 25 kcals Meat/Protein (lean): 0 Carb, 7g protein, 0-3g fat, 45 kcals Fats: 0g Carb, 0g protein, 5g fat, 45 kcals Measuring food Discouraged!! Exceptions: First time with a new food and very distorted view of portions New to treatment/meal planning Assure client that exchanges consider balance and quality of diet GOAL: NORMALIZE EATING NO!!!! Portion Distortion Woman's fist or baseball - a serving of vegetables or fruit A rounded handful - about one half cup cooked or raw veggies or cut fruit, a piece of fruit, or ½ cup of cooked rice or pasta - this is a good measure for a snack serving, such as chips or pretzels Deck of cards - a serving of meat, fish or poultry or the palm of your hand (don't count your fingers!) – ex: one chicken breast, ¼ pound hamburger patty Golf ball or large egg - one quarter cup of dried fruit or nuts Tennis ball - about one half cup of ice cream Computer mouse - about the size of a small baked potato Compact disc - about the size of one serving of pancake or small waffle Thumb tip - about one teaspoon of peanut butter Six dice - a serving of cheese Check book - a serving of fish (approximately 3 oz.) No Weighing! Ask client to refrain from weighing at home Weight 1-2/week with practitioner, less if stable (ex: normal wt BN) Blind weight: challenge client to focus on other measures of health and remind them of past experiences with weighing (i.e. triggers ED behaviors) What’s the point? Where does exercise fit in? Restrict with AN until eating improves and client reaches 90% ideal body weight With normal weight BN, wait for improvement in B/P Monitor client for compensatory exercise (trading vomiting for exercise) Explain rationale and caution against exercising on purging days due to electrolyte disturbance Start with mindful activity: yoga Weight bearing exercise and osteoporosis Female Athlete Triad Characterized by disordered eating, amenorrhea, and osteoporosis. 50% of these athletes may have bone mineral densities that are 1 standard deviation below normal for age. Requires exercise restriction. Coaches must de-emphasize weight and are cautioned to stop weighing athletes continually/focus on strength and mental conditioning. Some highly motivated and competitive athletes may correct their eating disorder if they are told that malnutrition will affect their performance. Meal Planning Using Exchange System Case Study see assessment form, sample meal plan and sample menus Vegetarianism and Considerations Duration of vegetarianism and motivation Minor/Adult Lacto-ovo? Vegan? Level of care Able to meet needs through other foods? Food Allergies Often used in service of ED and learned in higher LOC Verify if feasible (parents, allergist) and if accommodating allergy will limit progress Ex: gluten, nuts, mayo Offer alternatives Ex: for lactose intolerance offer lactaid tablet, lactaid milk, soy milk/yogurt Play detective! If it sounds fishy, it probably is! Ex: pt states gluten intolerant, but eats oatmeal/bran muffins GOAL: help to normalize eating and making peace with fear foods! HAES Model: Health at Every Size Health enhancement—attention to emotional, physical and spiritual wellbeing without focus on weight loss or achieving a specific “ideal weight” Size and self-acceptance—respect and appreciation for the wonderful diversity of body shapes and sizes (including one's own!), rather than the pursuit of an idealized weight or shape The pleasure of eating well—eating based on internal cues of hunger, satiety, and appetite, rather than on external food plans or diets The joy of movement—encouraging all physical activities for the associated pleasure and health benefits, rather than following a specific routine of regimented exercise for the primary purpose of weight loss An end to weight bias—recognition that body shape, size and/or weight are not evidence of any particular way of eating, level of physical activity, personality, psychological issue or moral character Confirmation that there is beauty and worth in EVERYbody Nutrition Education Topics Calcium intake and Osteoporosis Set Point Theory (Key’s Study) Danger of Fad Diets Function of Foods: Carbohydrate, Fat, Protein Changes to Expect with Refeeding (constipation, bloating, fullness) Moderate vs. Compulsive/Compensatory Exercise HAES model (Health at Every Size) Laxative Abuse Consequences of Malnutrition (Client ready handouts can be found in Winning the War Within) Questions? Thank you!