Pressure Ulcer - Clinical Departments
advertisement

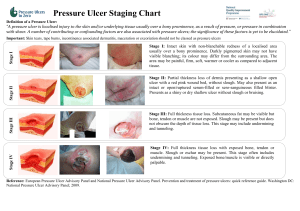
Keri Holmes-Maybank, MD Medical University of South Carolina 2.5 million hospitalized patients/yr 60,000 die/yr from pressure ulcer complications ◦ 1 in 25 if pressure ulcer reason for admit ◦ 1 in 8 if pressure ulcer secondary diagnosis 10-18% acute care patients 0.4-38% acute care new ulcers 80% increase pressure ulcer related hospitalizations 1993-2006 Length of Stay 13-14 days (average LOS 5 days) $9.2-15.6 billion in 2008 1999-2002 awards avg $13.5 million $312 million in one case Reduces quality of life Interfere with basic activities of daily living Increased pain Decrease functional ability Infection – OM and septicemia Increase length of stay Premature mortality Deformity Localized injury to the skin and/or underlying tissue 0ver a bony prominence Result of pressure, or pressure in combination with shear. Pressure is the force that is applied perpendicular to the surface of the skin. Compresses underlying tissue and small blood vessels hindering blood flow and nutrient supply. Tissues become ischemic and are damaged or die. Shear occurs when one layer of tissue slides horizontally over another, deforming adipose and muscle tissue, and disrupting blood flow. Ex: when the head of the bed is raised > 30 degrees. Occiput Ear Scapula Spinous Process Shoulder Elbow Iliac Crest Sacrum/Coccyx Ischial Tuberosity Trochanter Knee Malleolus Heel Toe Any skin surface subjected to excess pressure ◦ ◦ ◦ ◦ Oxygen tubing Drainage tubing Casts Cervical collars Bed bound individuals form a pressure ulcer in as little as 1-2 hours. Those in chairs may form a pressure ulcer in even less times because of greater relative force on skin. Expert panels recommend use of risk assessment tools. Tool is better than clinical judgment alone. Scores are predictive of pressure ulcer formation. Patients with a risk assessment have better documentation and more likely to have prevention initiated. Braden Scale Limited ability to reposition self in bed or chair ◦ ◦ ◦ ◦ ◦ ◦ Stroke with residual deficits Post-surgical Paraplegic Quadraplegic Wheelchair bound Bed bound Sensory perception Moisture Activity - degree of physical activity Mobility – ability to change body position Nutrition Friction and Shear Ability to respond meaningfully to pressurerelated discomfort. Completely Limited ◦ No moan/flinch, cannot feel pain most of body Very Limited – ◦ Responds only to pain, cannot feel pain ½ body Slightly Limited – ◦ Responds to command, cannot feel pain 1-2 limbs No Impairment Degree to which skin is exposed to moisture. Constantly Moist Very Moist ◦ Often but not always, change sheets each shift Occasionally Moist ◦ Extra linen change a day Rarely Moist ◦ Only routine linen change Degree of physical activity. Bedfast Chairfast ◦ Assisted into chair, cannot or barely walk Walks Occasionally ◦ Very short distance, most shift in bed Walks Frequently ◦ Walks outside room or in room every 2 hours Ability to change and control body position. Completely Immobile Very Limited ◦ Unable to make frequent or significant changes Slightly Limited ◦ Makes frequent but small changes No Limitation Usual food intake pattern. Very Poor ◦ 1/3 meal, <2 servings protein, NPO w IVF Probably Inadequate ◦ ½ meal, 3 servings protein, poor tube feeds Adequate ◦ >1/2 meals, 4 servings protein, supps, TF or TPN Excellent Sliding, rubbing against sheets, bed, chair, etc. Problem ◦ Mod-max assist, slides, cannot move without slide against sheets, spasticity, contractures, agitation Potential Problem ◦ Feeble, min assist, occ slides, indep moves with slide No Apparent Problem Braden Scale score of 18 or less initiate prevention. Score of 1 or 2 initiate specialty bed. Partial thickness wound involves ONLY the epidermis and dermis – Stage II. Full thickness wound involves the epidermis and dermis and extends into deeper tissues (subcutaneous fat, muscle) – Stages III and IV. The ulcer appears as a defined area of redness that does not blanch (become pale) under applied light pressure – Stage I. Tissue destruction underneath intact skin at the wound edge. Wound edges are not attached to the wound base. Edges overhang the periphery of the wound. Pressure ulcer may be larger in area under the skin surface. Tunnel is a narrow channel of tissue loss that can extend in any direction away from the wound through soft tissue and muscle. Tunnel may result in dead space which can complicate wound healing. Depth of the tunnel can be measured using a cotton-tipped applicator or gloved finger. INTACT SKIN. NON-BLANCHABLE redness of a localized area. Difficult to detect in individuals with dark skin tones - affected site is deeper in color. Surrounding skin will feel different than effected area. May indicate “at risk” persons. Partial thickness loss of dermis presenting as shallow open ulcer with a RED-PINK wound bed. Shiny or dry shallow ulcer. No slough or bruising. BLISTER - intact, open or ruptured serum or serosangineous-filled. Tissue surrounding the areas of epidermal loss are erythemic. FULL-THICKNESS tissue loss. Subcutaneous fat may be visible. Bone, tendon, or muscle is NOT visible or directly palpable. Slough may be present but does NOT obscure the depth of tissue loss. May include undermining and tunneling. The depth of a Stage III pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have subcutaneous tissue so Stage III ulcers can be shallow. Areas of significant adiposity can develop extremely deep Stage III pressure ulcers. FULL-THICKNESS tissue loss. BONE, TENDON, or MUSCLE is visible or directly palpable. Slough or eschar may be present but does NOT obscure wound bed. Often includes undermining and tunneling. Can extend into supporting structures (fascia, tendon or joint capsule) making osteomyelitis or osteitis likely . The depth of a Stage IV pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have subcutaneous tissue and these ulcers can be shallow. FULL-THICKNESS tissue loss in which SLOUGH (yellow, tan, gray, green, or brown), ESCHAR (tan, brown, or black), or both COVER the base of the ulcer. Cannot determine true depth of wound secondary to slough and/or eschar. Will be either a Stage III or IV. INTACT SKIN. PURPLE or MAROON. BLOOD FILLED BLISTER. May be difficult to detect in individuals with dark skin tones. Color and mechanical stiffness of the skin (firm, mushy, boggy) assist in differentiating between DTI and a Stage I pressure ulcer. Most common: ◦ Sacrum, buttocks and heels. Heel may look like a bruise or a blood blister. 1% resolve spontaneously. Evolution: ◦ ◦ ◦ ◦ Thin blister over a dark wound bed. Covered by thin eschar. May rapidly evolve. Likely become a Stage III or IV. Skin Tears Venous Ulcers Arterial Ulcers Diabetic Ulcers Perineal (Incontinence Associated) Dermatitis Separation of epidermis from the dermis or epidermis and dermis from underlying tissue. Thin skin, less elastic, purpura or ecchymosis. Epidermal flap. Impaired arterial flow to the lower leg and foot. Tissue ischemia, necrosis and loss WELL DEFINED MARGINS Toes, foot, malleolus Thin, shiny skin, cool skin temperature, decreased or absent hair Painful - increase with elevation Decreased pulse Minimal exudate Pale wound bed; necrotic tissue Decrease in blood return from leg and foot. Between the knee and the ankle. Thickened, brown discolored skin is noted around the lower calf, ankle and proximal foot. Skin proximal and distal to the wound is reddened. Ulcer that occurs in diabetics Metatarsal head, top of toes, and foot Neuropathy, poor microvascular circulation Repetitive trauma, unperceived pressure, or friction/shear Regular wound margins Callus around wound Dry, cracked, warm Skin irritation from incontinence. Erosion of epidermis and dermis from mechanical injury to macerated skin. Buttocks, perineum, and upper thighs. Secondary infection. Diffuse erythema. Scaling, papule and vesicle formation . Tissue “weeping”. National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel. (2009). Prevention and treatment of pressure ulcers: Clinical practice guideline. Washington DC: National Pressure Ulcer Advisory Panel. http://www.npuap.org https://www.nursingquality.org Panel for the Prediction and Prevention of Pressure Ulcers in Adults. Prediction and Prevention. Rockville MD. Agency for Health Care Policy and Research. 1992. May. AHCPR Clinical Practice Guidelines, No. 3. Bates-Jensen BM, MacLean CH. Quality Indicators for the Care of Pressure Ulcers in Vulnerable Elders. JAGS 55:S409-S416, 2007.