Infectious Disease and Immune - Faculty Sites
advertisement

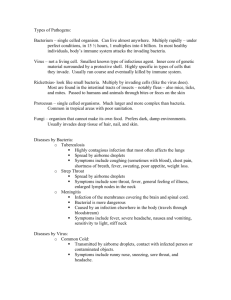
Infectious Disease and Immune By: Diana Blum MSN Metropolitan Community College NURS 2150 History • http://www.youtube.com/watch?v=TteIB1oo4C0&f eature=related Immune System • Protects the body against infection and cancer development • Stimulates tissue growth and repair after injury • Inflammation causes damage • Are able to fail to recognize self and launch a defense against own cells= autoimmune response • Those compromised include but are limited to: cancer pts, HIV patients, etc. Anatomy Parts • Bone Marrow • Granulocytes o Neutrophils o Basophils o Eosinophils • NonGranulocytes o Monocytes o Lymphocytes • Lymph System o Nodes o Tonsils and adenoids o spleen Natural Immunity • Body provides its own protection • Includes o Skin o MM o Gastric pH Acquired Immunity • After birth includes: o o o o Antibodies Tcells Bcells cytokines • Active o Production of antibodies in response to foreign antigen. o Get by getting disease or vaccine o Involves lymphocytes Hypersensitivity • Aka: Allergy o Responds to antigen that we have been exposed too; ex. Cat dander o s/s: itchy, watery eyes, sneezing..to more life threatening like asthma, anaphylaxis, bronchoconstriction, or circulatory collapse • Example: allergic rhinitis Contact can be: inhaled, ingested, injected, tactile Life threatening like anaphylaxis involve blood vessel and bronchial smooth muscle with systemic dilation, decreased cardiac output, and bronchoconstriction 5 types 1: rapid IgE hypersensitivity: most common, increase in IgE, causes release of histamine from basophils, eosinophils, and mast cells anaphylaxis, asthma, etc caused from hay fever, latex allergy, peanuts, bees, etc. 2: cytotoxic: rx of IgG w/ host cell membrane; ex. Myasthenia gravis, blood transfusions 3: immune complex: formation of immune complex in walls of blood vessels; ex lupus, rheumatoid arthritis 4: delayed or cell mediated: rx of sensitized T cells w/ antigen and release of lymphokines that induce inflammation; ex. Poison ivy, positive TB test, graft rejection 5: stimulated: rx of auto antibodies with normal cell surface receptors that cause an overreaction of the target cell; ex. Graves’ dx Immunocompromised Population assessment • Ask for onset, duration, and detailed history • Ask about, work, school, hobbies, home, sports • Ask about allergies of family members b/c some are inherited • Assess for rhinorrhea, itchy watery eyes, headache especially over sinuses, dry scratchy throat • Obtain CBC, Immunoglobin E level, scratch test, perform a food challenge interventions • Avoidance of allergen • Symptom relief • Medications: antihistamines, mast cell stabilizers, decongestants, corticosteroids, allergy shots Anaphylaxis Most life threatening Affects many organs within seconds Not that common Teach avoidance of allergen If food related instruct to ask if present in foods at restaurants • Epinephrine shots should be carried with them • • • • • • s/s: impending doom, weakness, apprehension, general itching, hives, angioedema (lips, eyes, tongue), audible wheezes, anxiety, stridor, respiratory failure may occur, may be hypotensive, may have rapid irregular pulse, confusion may occur • Eventually could lose consciousness and cardiac arrest • Treatment o o o o o o o o Assess respiratory function first This is an EMERGENCY, CALL 911 Establish airway if needed CPR may be needed Administer epinephrine 0.3 to 0.5ml of the 1:1000 concentration Benadryl given IV 25-100mg Oxygen as needed Monitor sats Latex Allergy • May be contact type • May be anaphylactic like • Healthcare workers, clients with spina bifida, and those that use latex condoms are most at risk • Tx: use non latex items Respiratory interventions for immunity Pneumonia Excess fluid in lungs from inflammatory process May be nosocomial in nature If untreated it can go to blood and cause sepsis s/s: atelectasis, hypoxemia, flushed cheeks, myalgia, chills, fever, cough, tachycardia, dyspnea, sputum production, pain, crackles • Causes: bacteria, virus, fungi, protozoa, helminths, etc. , toxic gases, smoke, aspiration • Tx: sputum culture, cbc, HIV, abg’s, cxr, bronchoscopy, biospy, antibiotics, • • • • TB • Highly infectious • Transmitted via airborne route when someone infected laughs, coughs, sneezes, whistles, or sings. • More are infected than have active version • Caseation Necrotic tissue can be turned into a granular mass in the center of the lesion..if found on xray it is called ghon tubercle or prime lesion • The lesions then calcify or liquefy • Greatest risk: frequent contact, immune suppressed, HIV, those that live in crowded areas, homeless, drug users, low social class, foreign immigrants • Assess: country of origin, travels, previous hx, anyone with BCG vaccine will test positive • s/s: fatigue, lethargy, nausea, anorexia, wt loss, irregular menses, fever, night sweats, cough, bloody purulent sputum, chest tightness, local wheezing • Diagnostics: culture, gram stain, TB tine, cxr Once positive always positive Place in negative pressure room. Airborne precautions Wear n95 mask when working with client Teach prevention Vitamin c, iron , and protein are important for those infected • Watch client swallow meds • Tx: meds • • • • • • Sinusitis • Inflamed mucous membranes • Causes: deviated septum, polyps, tumors, cocaine, facial trauma, nasal intubation, dental infection, decreased immune response • s/s: obstructive swelling, facial pressure, pain, fever, headache, congestion, cough, tenderness, drainage • Complications: meningitis, abcesses, cellulitis • Most common in frontal and maxillary sinuses • Tx: broad spectrum antibx, analgesics, humidity, saline irrigation, lavage, removal of infection by way of surgery Pharyngitis • Sore throat • Causes: group a strep or virus • Highest incidence b/w late fall and spring in colder climates • s/s: dry sore throat, pain w/ swallowing, dysphagia, fever, hypermia (redness), may or may not have enlarged tonsils, drainage can be thin or thick and even purulent • Tx: throat cultures, cbc, lozenges, antibiotics • Instruct client to complete full course of antibx tx • If it does not improve, the client should check on getting HIV testing or the client could be immunosuppressed HIV/AIDS By: Diana Blum RN BSN Metropolitan Community College Nursing 2150 Immune System • Helps prevent infection • Failure is caused by 1 of 2 things o Congenital abnormalities • Present at birth o Acquired after birth • Infection, toxin, medical therapy HIV/AIDs HIV Found In 1981 Death is Result of Opportunistic infection Poor prognosis Class= Retrovirus Aids Attacks CD4/ T cell • http://video.google.com/videoplay?docid=5219920342681496180&q=hiv+%22aids%22+educ ational+duration%3Amedium+is%3Afree&pr=go og-sl 3 categories A 1. HIV positive 2. Asymptomatic Or 3. Persistent Lymphadenopathy 4. Prone to Acute infections B 1. Bacterial Endocarditis, pneumonia or sepsis 2. Candidiasis for 1 or more months 3. Severe cervical dysplasia or carcinoma 4. Fever or diarrhea x 1month or more 5.Oral hairy leukoplakia 6.Shingles (Herpes Zoster) 7.Idiopathic thrombocytopenic purpura 8. Pelvic inflammatory disease 9.Peripheral neuropathy C • • • • • • • • • • • • 1. Pulmonary candidiasis 2. Invasive cervical cancer 3. Cytomegaly virus 4. HIV related encephalopathy 5.Herpes simplex 6.Kaposi’s Sarcoma 7. Lymphoma 8. Tuberculosis 9. Pneumocystis Carinii pneumonia 10. Toxoplasmosis 11. Wasting syndrome 12.Salmonella Septicemia Pictures of cell with HIV/AIDS Causes • Sexual: genital, anal, or oral sex with exposure of the mucous membranes to infected semen or vaginal secretions • Parenteral: sharing of needles or equipment contaminated with infected blood or receiving contaminated blood products • Perinatal: from the placenta. from contact with maternal blood and body fluids during birth or from breast milk from infected mother to the child HIV and the Healthcare Worker • # 1 transmission between healthcare worker and client is NEEDLE STICKS • ALWAYS use standard precautions • Page 1926 Staging • Initial: lasts 4-8 weeks o High levels in blood o Flulike symptoms • Latent: inactive until a virus presents than replication begins o Lasts 2-12 years o Asymptomatic • Third stage=opportunistic infections o 2-3 years • • • • • • • • • • Flu like symptoms Fever Night sweats Swollen lymph nodes Headache Skin lesions that don’t heal Sore throat Dyspnea Burning with urination diarrhea S/S • Fatigue • Weight loss Complications Opportunistic Infections • These occur because Aids patients are immune suppressed • More than one can occur at the same time • Can be o o o o Protozoan Fungal Bacterial Viral Protozoan • Pneumocystitis carinii pneumonia o DOE, tachypnea, persistent dry cough, fever, fatigue, wt loss • Toxoplasmosis encephalitis o Caused by toxoplasma gondii contact w/ cat feces or undercooked meat o Change in mental status, neurological deficits, HA, fever, diff speaking, vision and gait problems, seizures, lethargy, confusion • Cryptosporidiosis o Intestinal infection caused by cryptosporidium organisms o Mild diarrhea to severe wasting with electrolyte imbalances Fungal • Candida albicanspart of natural flora in GI tract (Stomatitis or esophagitits is common in the AIDS pt.) o Overgrowth in AIDS clients • Cottage cheese like yellow/white plaques and inflammation (mouth), pruritis, perineal irritation, thick white vaginal discharge • Frequent yeast infections is common in the female AIDS pt. • Cryptococcosis mengititis o Fever, HA, blurred vision, N/V, nuchal rigidity, confusion, seizures • Histoplasmosisbegins as respiratory infection then to systemic infection o Dyspnea, fever, cough weight loss, enlarged lymph nodes spleen and liver Bacterial • Recurrent Pneumonia o CP, productive cough, fever, dyspnea • Mycobacterium avium complex is most common o Affects respiratory and GI tract o + cultures are found in blood, bone marrow, and lymph nodes o s/sfever, debility, wt loss, malaise, swollen lymph glands and/or organs • TB o Fever, chills, night sweats, wt loss, anorexia, cough dyspnea, CP, Viral • CMV (cytomegaly virus) can be in eyes, lungs, GI tract, and CNS o Fever, malaise, wt loss, fatigue, swollen lymph glands, blindness, colitis, diarrhea, abd bloating, discomfort, encephalitis, pneumonitis, adrenalitis, hepatitis, etc. • Herpes Simplex Virusoccurs in perirectal, oral, and genital areas o Longer lasting o Numbness/tingling at site of infection, lesions that are painful, fever, bleeding, lymph node enlargement, headache, myalgia, malaise • Varicella Zoster (shingles)(chicken pox) o HA, fever, pain, rash,fluid filled blisters sometimes Malignancies • Kaposi’s Sarcomamost common o Related to herpes virus o Small purplish brown raised lesion that are not usually painful or itchy o Lesions found in lymph nodes, intestinal tract, lungs o Diagnosed by biopsy o Assess #, size, and location of lesions and monitor progression • Lymphomas non Hodgkin’s B cell lymphoma, immunoblastic lymphoma (Burkitt’s) and primary brain lymphoma o Weight loss, fever, night sweats Endocrine Complications • Gonadal dysfunction change in libido • Body shape changes buffalo humps or abd fat, other areas of body appear to be wasting away • Adrenal insufficiency manifests as fatigue, wt loss, N/V, hypotension, electrolyte imbalances • DM • Hypercholesterolemia • Men with AIDS tend to have low testosterone levels • Women with AIDS tend to have irregular menstrual cycles OTHER Complications • Dementia may be from infection, medication o Neuropathies, pain, gait disturbance, confusion • Wasting Syndrome not because of any one problem, usually from metabolism issue o Diarrhea, malabsorption, anorexia, oral and esophageal lesions • Skin changes dry, itchy skin with possible rashes o Low platelet level can mean petechiae or bleeding gums may also be present • • • • • • • • • TESTING Positive ELIZA test Positive Western Blot test Lymphocyte Counts CD4/CD8 Counts Antibody tests Viral Culture Viral Loading Test Quantitative RNA Assays P24 Assay • See pages 1934-1935 Treatment • • • • • • • • • • No cure Treat symptoms Prevent infections Encourage to eat balanced diet Exercise regularly Maintain good dental hygiene Smoking/illegal drug cessation Limit alcohol Minimize stress Practice safe sex Nursing Care • Early stages- usually treated outpatient • Late stages- more intensive in nature • Infection is the leading cause of death in those with HIV • Education! • Education! • Education! • This is the key!!! • The higher the blood level of HIV (Viremia) the greater risk of transmission!!! • • • • • • • • Client education Use latex condoms Store condoms in a cool dry place DON’T use condoms from a damaged package Handle condoms with care so as to not puncture them Teach clients how to properly apply condoms and to use adequate water based lubricant Replace a broken condom immediately Follow recommended drug regimens Encourage ways to maintain immune function o Diet • Avoid raw or rare fish fowl or meat • Thoroughly was fruit and veggies o Adequate rest o Exercise o Stress reduction Nursing Diagnosis • • • • • • • Ineffective therapeutic regimen Anxiety Infection Impaired oral mucosa Imbalanced nutrition less than body requirements Disturbed thought process pain • • • • • • • • • • • Interventions Provide education Offer support group Encourage questions Encourage them to express self Anti infectives Medication education Encourage regular dental hygiene Have dietician see Appetite stimulants Saftey precautions Monitor pain • Your client is a 32 year old white male who is new to the outpatient clinic. He presents with fatigue, abd pain, low grade fever, nausea, and anorexia. Upon assessment you notice yellowing eyes and darkening urine. He states, “I try to eat right, take vitamins, and get rest.” he feels like he is getting worse. He was in a monogamous gay relationship for 6 yrs that recently broke up. He had unprotected sex 2 weeks ago. His last HIV test was 1 year ago and it was negative. • He asks if his current symptoms are related to his recent sexual encounter. How do you respond? • Wound you counsel this man to have an HIV test? Why or why not? • Should you teach the client about safe sex practices? Why or why not? • You are the charge nurse on a busy med surg unit at the hospital. Right before change of shift, one of the new hires tell you that she was giving her 78/f client insulin and accidentally stuck herself when placing the needle in the sharps container…in talking with other nurses she doubts that this is a high risk needle stick and thinks she will be fine. She washes off the blood throroughly and applies betadine to her finger. She wants to fill out the incident report and go home. • How will you consel this nurse about needle stick injuries? • What rights and obligations does she have? • What other blood borne diseases could she have been exposed to? • Should the nurse notify her sexual partner(s) of this incident? Why or why not? Sjogren’s Dx • s/s: dry eyes, dry mm of nose and mouth, vaginal dryness, blurred vision, diff swallowing, epistaxis, enlarged lymph nodes, may have swollen painful joints, • Fibromyalagia can also occur with this • Insufficient tears cause corneal inflammation and ulcerations • Decrease in digestion of carbs, promotes tooth decay • Tx: no cure, chemo like drugs, immunosuppressives, tx symptoms MENIN GITIS • INFLAMMATION OF ARACHNOID AND PIA MATER OF THE BRAIN, CSF, AND SPINAL CORD • Can be bacterial or viral, fungal, or protozoal o Bacterial and viral are the more common types o Viral is self limiting (not life threatening) • Organism enters via bloodstream Viral Most common May occur with herpes simplex or zoster No organisms present in CSF Tx: treat symptoms, acyclovir if genital lesions S/S: ◦ ◦ ◦ ◦ ◦ ◦ ◦ Fever Photophobia Headache Myalgias Nausea Poss. Genital lesions Rash Fungal • Cryptococcus is most common fugus o Especially in AIDS patients • S/S: vary but can include fungal sinusitis, fever, headache, nausea, vomiting, decrease LOC • Tx: treat symptoms, IV antifungal agents Bacterial Medical emergency Mortality rate of 25% Most in fall/winter Culprits: streptococcus pneumoniae and neisseria meningitidis • Approx. 17,500 new cases each year in the USA • Meningococcal meningitis is the only bacterial type that has outbreaks • • • • Bacterial • S/S o o o o o o o o o Headache N/V Fever Photphobia Increased ICP that causes hydrocephalus Nuchal rigidity (neck stiffness) Seizure Decreased LOC Poss. gangrene bacterial • Diagnostics o o o o o o o Lumbar puncture w/ broad spectrum antibx prior Counterimmunoelectrophoresis- looks for virus/protozoa C&S of blood,urine, throat, and nose CBC BMP Chest, sinus,mastoid xrays MRI and/or CT to look for increased ICP Treatment ◦ ◦ ◦ ◦ ◦ Bacterial Neuro checks q 4 hours Isolation Broad spectrum antibx til cultures back Possible to be on steroids Monitor for complications Septic emboli Temp, color, pulse,cap refill Hand circulation is the most affected Shock Coag disorders Bacterial endocarditis Prolonged fever Encephalitis • Inflammation of the brain parenchyma and meninges • Affects brainstem, cerebrum, and cerebellum • Virus invades brain tissue and reproduces causing and inflammatory process • Demyelination of axons occur • Widespread edema leads to increased ICP types • Arboviruses: example west nile o o o o o Transmitted by infected tick or mosquito Usually asymptomatic otherwise flu like symptoms Has IGM antibody affected Incubation 3-12 days after bite Transmitted thru breast milk , blood, organ trasplant • enterovirus: examples:chickenpox, herpes zoster, mumps are most common causes. • Amebae: virus found in warm fresh water o Enters nasal mucosa when swimming • • • • • • • • • • Assessment/interventions Fever n/v Stiff neck Changes in LOC Fatigue Motor dysfunction Increased ICP Weakness Hemiplegia Seizure activity • • • • • Monitor vitals TCDB q2 hrs Suction as ordered Neuro check q 2 hrs Meds Brain Abcess Pus like Infection of the brain Organisms come from ear, sinus, mastoid Can occur with septic emboli Can be from penetrating trauma Usually occurs deep within the cerebral hemisphere and involves white matter • Most occur in frontal and temporal lobes • • • • • Assessments/diagnostics • s/s: headache, fever, lethargy, confusion, increased ICP, decreased LOC, airway and respirations may be affected • Assess neuro function • Assess visual fields for blindness • Assess gait • CBC, CT, EEG, MRI, lumbar puncture Treatments • • • • Antibiotics Antiepileptics Burr hole surgery to relieve pressure and drain Crainiotomy Lyme Disease • • • • • • • • Reportable infection 85% seen in new England, mid Atlantic, and upper Midwest, and northern California Caused by spirochete borrelia burgdorfori From bite of deer tick s/s:stage 1 o bulls eye rash is tell tale sign o Malaise, fever, headache, muscle, joint ache/stiffness Stage 2: 2-12 weeks after tick bite o Carditis, dysrythmias, dizzy, palpitations, meningitis, facial paralysis Stage 3: weeks to yrs after bite o Arthritis, permanent damage to joints Tx: antibx Rocky Mountain Spotted Fever • a tickborne disease caused by the bacterium Rickettsia rickettsii. o o is a cause of potentially fatal human illness in North and South America, and is transmitted to humans by the bite of infected tick species. In the United States, these include the American dog tick (Dermacentor variabilis), Rocky Mountain wood tick (Dermacentor andersoni), and brown dog tick (Rhipicephalus sanguineus). • Symptoms: fever, headache, abdominal pain, vomiting, and muscle pain. A rash may also develop, but is often absent in the first few days, and in some patients, never develops. • can be a severe or even fatal illness if not treated in the first few days of symptoms. • Tx: Doxycycline is the first line treatment for adults and children of all ages, and is most effective if started before the fifth day of symptoms • Info from cdc Conjunctivitis • Inflammation of the conjuctiva • Related to allergen exposure • Is not contagious unless from virus or bacteria o Pink eye: blood shot eyes, edema, tears, discharge • Get cultures • s/s: burning, engorged blood vessels, excessive tears, itching • Tx: o o o o Corticosteroids gtts Prevent spread if infectious Anti infectives if needed Handwashing • 3 types Otitis Media o Acute: r/t infection, sudden onset o Chronic: r/t infection, reoccuring o serous • s/s: inflammation, swelling, irritation, possible purulent drainage, may cause permanent hearing loss if left untreated, ear pain, headaches, vertigo, may lead to perforated ear drum • Tx: cultures, needle aspiration, cold therapy, heat therapy, antibiotics, analgesics, antihistamines, decongestants, surgery to place tubes Mastoiditis • Infection of the mastoid air cells caused by otitis media • May be acute or chronic • s/s: swelling behind the ear, pain, cellulitis, poss perforated ear drum that is also red, and thick, tender enlarged lymph nodes behind the ear, fever, malaise, drainage, anorexia • Tx: IV antibx, cultures, surgical removal of infected tissure • Complications from surgery: damage to cranial nerves, decreased ability to look lateral, drooping mouth on affected side, vertigo, meningitis, brain abcess, wound infection Labyrinthitis • Infection of the labyrinth which could be a result of otitis media. • Infection is from erosion of bony capsule • May follow inner or middle ear surgery • May be viral in nature or related to mono • s/s: hearing loss, tinnitis, vertigo, nystagmus to affected side, n/v • Meningitis is common complication • Tx: systemic antibx, antiemetics, stay in bed in dark room until manifestations subside, gait training, PT • Hearing loss may be permanent..provide support, Meniere’s Disease • Tinnitus, one sided hearing loss, and vertigo • Attacks last several days • Unknown cause except that too much or too little endolymphatic fluid is produced • Eventually hearing loss is permanant • Often occurs with infections, allergic reactions, and fluid imbalance Cancer • • • • Neutropenic precautions Thrombocytopenic precautions Bleeding precautions Protect from infections Skin Infection Management • Contact---gown and gloves • Parasite---gown, gloves, cap, shoe covers, isolation, hygiene, insecticide ointments, special shampoos, beding and clothes washed daily on hot water, dried in hot dryer • Fungal— antifungals, culture, cool compress, skin off skin, • Viral--- antiviral agents,treat symptoms, cryotherapy if warts, or duct tape for 2 months if wart • Bacterial—antibiotics, potential debridement and drainage, cultures and senstivities, no sharing towels etc. Pain meds, rest contact precautions Any Questions?