Coastal Annual Meeting - PCMH - Patient
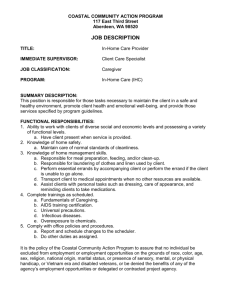
advertisement

A PCMH Journey Lessons Learned Al Kurose, MD President & CEO Meryl Moss, MPA Chief Operating Officer Coastal Medical 88 doctors, 25 NP’s/PA’s, 20 offices 102,351 patients Predominantly primary care Patient Centered Medical Home (PCMH) for 4 years Accountable care for almost 2 years Coastal Medical is Selected as 2012 Ambulatory HIMSS Davies Award Winner HIMSS Davies Award recognizes excellence in use of the EHR to successfully improve quality of care and patient safety. All Coastal Locations are Level III Recognized Patient Centered Medical Homes. All Coastal Locations Have Achieved Stage 2 Meaningful Use Patient Centered Care Thoughtful Execution Structure combined with flexibility Communication, information, conversation and feedback Allocation of correct staff resources Design workflow that support patient focused care You must care what patients, staff and physicians think. Leveraging Technology Coastal went live in 2006 with eClinicalWorks Registry reporting Requires structured data fields HIT for Patient Engagement & Education patient portal, social media, website, digital signage Workflow Changes Begin Structure data needs to be part of every day work flow. Structure data required for NCQA & Meaningful Use Technology can shift work to Physicians…need to shift it back to staff. Need to leverage technology to control office work. The PCMH Team Committed to PCMH model in 2009 Participation in CSI informed use of Nurse Care Managers as key to success Nurse Care Managers embedded in offices Expanded Pharmacy Services Pharmacists long time members of the team Extended PCMH team to hospitals, nursing Homes and skilled nursing facilities Shifting Established Roles Patient in the center of the team Strong roles for NCMs, pharmacists, nurse practitioners and physicians’ assistants Medical assistants working at a higher level All practice staff now part of patient centered team Lessons Learned Training, training and more training Needed to upgrade the quality of employees Standardization Required: Ways to greet patients Professional demeanor Uniformed dress Way to answer the phone Lessons Learned Monitoring and surveying everyone’s experience Concentrate on sickest and most costly patients (5%) Focus on Transitions Hospital (2 NCMs, now Pharmacy connection) Nursing homes and skilled nursing facilities Telephonic Pharmacy phone calls work too Improved Patient Experience Established 1-800 “New Patient Hotline” Uniform welcome packet for new patients Patient panels to population management Every patient is part of our PCMH Coastal community Coastal 365: Weekend, evening and holiday access Added Extenders ER Communication required new workflow Evaluate Progress Patient Satisfaction Surveys Employee Satisfaction Surveys Provider Satisfaction Surveys Brainstorming Sessions w/PCMH Teams Practice Assessments What Did We Learn? Highly Satisfied Patients: Few opportunities for improvement. Highly Satisfied Employees: Opportunities for improvement: Increase ability for Medical Assistants and Secretaries to contribute to the clinical team Improve staffing ratios to allow practice staff to spend additional time on patient care processes Practice Assessment Results What we Learned: Antiquated workflows Not enough support staff for patient centric processes. Need for new process maps for all visits Physician visit Medical Assistant/Nursing visit Laboratory visit Need new process for pre-visit planning: Emphasis on test and laboratory follow-up Physicians have too much work! Here are some comments: Biggest Challenge is: Finishing at a reasonable hour Time management and flow Time spent is arduous Trying to meet different requirements by different entities Too many more tasks required to care for patients Just completing the vast amount of work Too many data points to worry about Our Next Steps Redesign of office practice work flows Change in roles and responsibilities Increase and realignment of staff Roll out of new training and education Reduction in physician only tasks Patient Centered Programs Lessons Learned Al Kurose, MD President & CEO ER Communication Pilot: The Program At Miriam and RIH UEMF, Lifespan, BCBSRI, Coastal Wristband at registration ER calls MD about every patient Single 800 number for all Coastal patients On call doctor has access to EMR ER Communication Pilot: Lessons Learned It takes time for a pilot to gain traction It’s been good to work together Docs don’t like 3 AM calls for a sprained ankle Every Coastal office now holds open an 11 AM This program is improving patient care Pharmacy Management: The Program 4 Full time clinical pharmacists (PharmD’s) Telephonic Cardiac Risk Reduction In-person Medication Therapy Management Telephonic brand to generic: $1.2 M annualized savings in first 5 months URI College of Pharmacy residency training site Pharmacy Management: Lessons Learned Telephonic is effective Medication Therapy Management visits are great Brand to generic is low hanging fruit re: managing cost It is great to work together! Med Rec for MA’s: The Program Led by Sarah Thompson, PharmD at Coastal Curriculum development w URI College of Pharmacy Certificate program through CCRI Four two-hour sessions Med Reconciliation Curriculum 1. Recognition of top 100 Drugs 2. Basic pharmaceutical calculations 3. Common prescription abbreviations 4. Process for performing medication reconciliation 5. Understanding drug information resources 6. Assessing patients for medication adherence Med Rec for MA’s: Lessons Learned It was good to work with the College of Pharmacy Separate training for pediatrics and FM Focus more on EHR ‘basics’ More practical pharmacy calculations Less disease state education 3 sessions instead of 4 Palliative Care and Hospice: The Program VNHC and HHCRI Two in-service visits to every office Utilization: Q4 2011: 0 pts. in palliative care, 11 pts. in hospice Oct. 2012: 13 pts. in palliative care; 67 pts. in hospice Jun. 2013: 38 pts. in palliative care; 68 pts. in hospice Length of stay in hospice: 7 days when we started; 21 days now 25-30 days is optimal Palliative Care and Hospice: Lessons Learned We were underutilizing these services In-service visits to our offices were valuable Screening tool for palliative care is useful It’s been good to work together Streamlined process with a single organization beneficial Quality Measures: The Program 69 measures across 5 contracts Currently all amenable to automated queries Monthly exception reports to every practice “Sink or swim” as a group Compensation is tied to performance on quality BCBSRI Adult Quality Targets Quality Measures: Lessons Learned Standardization of documentation takes effort Closing gaps in care requires workflow and resources Perceived performance generally exceeds actual Full time EMR trainers are valuable assets Quality improvement requires more staff What is “Accountable Care”? It’s care in pursuit of the Triple Aim: Better population health Better care (Quality, experience of care) Lower per capita cost It’s usually care under a shared savings contract Accountability for total cost of care Risk adjusted budget Quality measures that impact payment +/- Infrastructure support ACO’s “Public” versus “private” ACO’s Public Pioneer ACO’s Medicare Shared Savings Program (MSSP) Private: BCBSRI Shared Savings UHC, others ACO Models: Hospital centric Multispecialty Primary care driven Coastal: A “Primary Care Driven ACO” Coastal is “all in”: Most ACO’s still single payer Coastal: 5 shared savings contracts Cover the majority of our patients Shared savings contract features Shared savings opportunity Quality targets that impact shared savings +/- Infrastructure support ACO Infrastructure Chief Medical Officer Directors: Analytics, Practice Management Staff: analytics, IT, communication, EMR trainers 17 Nurse Care Managers embedded in practices 2 Nurse Care Managers in hospitals, one in SNF’s 4 Clinical Pharmacists New Analytics and Care Registry Platform We are building a new set of core competencies ACO: Lessons Learned Autonomy vs. standardization: an important trade off Fee-for-service incentives persist in shared savings Overhead allocation matters: more staff = less income Understanding total cost of care is difficult Timely actionable cost data is hard to come by Doctors and patients need to know prices ACO’s require new types of expertise The new infrastructure required by ACO’s is significant Coastal’s Perspective Value is being redefined in healthcare. That’s good. 30% waste in the system is a huge opportunity. Incentives matter. We think accountable care will work for us. Patients love it already. The long view: Work on health, not just healthcare