Xarelto 'From Strength 2 Strength' slide template
advertisement
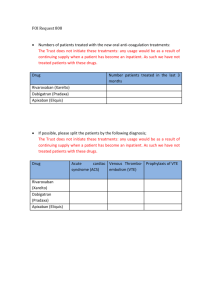
Rivaroxaban LCM studies program overview Martin van Eickels MD Head of Global Medical Affairs Thrombosis Bayer Healthcare Continued Success Through Scientific Endeavour 2013 2008 1993 1990 1975 1899 Rivaroxaban: From Clinical Studies to Real-World Patients Phase II studies Phase III studies Patients in LCM study programme Phase IV studies IIR projects Patients treated to date* *Estimate based on IMS data To Meet the Needs for Improved Treatments Options Our R&D Goals Predictable, once daily oral administration Broad therapeutic window Potent antithrombotic activity No routine coagulation monitoring Long-term anticoagulation therapy from hospital to home Scientific Research Center Bayer Pharma AG in Wuppertal The Vision was to Provide Patients with Improved Anticoagulation Options A good balance of efficacy and safety Wide therapeutic window Oral administration Fixed dosing regimens No need for routine coagulation monitoring Fast onset and offset of action Low risk of food and drug interactions Once-daily dosing if possible Factor Xa: A Key Factor in the Coagulation Cascade TF VIIa Initiation X IX IXa Xa Propagation Inactive factor II Prothrombin Factor Xa – The gate keeper IIa Active factor Thrombin Transformation Catalysis Adapted from Spyropoulos 2007 Fibrinogen Fibrin Clot formation 1998 High-Throughput Screening: 5 Promising ‘Lead Structures’ 1998 Bayer substance library 200,000 substances screened 1999 Identification of 5 lead compounds as a starting point for improvement Preclinical project Factor Xa Chemical optimization Discovery of rivaroxaban In vitro and in vivo animal models Roehrig et al, 2005; Perzborn et al, 2011 Crystal Structure of Rivaroxaban Revealed Rivaroxaban FXa Tyr228 Roehrig et al, 2005 2002 A Promising Pharmacological Profile Emerges Selective, direct Factor Xa inhibitor1 High oral bioavailability2 Rapid onset of action2 Half-life 5–13 hours2-4 66% metabolized 33% (unchanged drug) Limited drug–drug interactions 50% inactive metabolites Dual mode of elimination5 1. Perzborn et al, 2005; 2. Kubitza et al, 2005a; 3. Kubitza et al, 2005b; 4. Kubitza et al, 2008; 5. Weinz et al, 2009 2002 Extensive Phase I Programme Phase I programme Bioavailability/absorption PK/PD single-dose escalation Metabolism/excretion PK/PD multiple-dose escalation PK/PD in special populations DDI (PK interactions) Age Sex Body weight Renal impairment Hepatic impairment Ethnicity Heart failure patients Other studies Thrombin generation Perfusion chamber CYP3A4/P-gp inhibitors CYP3A4/P-gp inducers CYP3A4/P-gp substrates Ranitidine DDI (PD interactions) ASA Clopidogrel Enoxaparin Naproxen Warfarin (switching from/to) Early Evidence for Once-Daily Dosing between rivaroxaban 10 mg and enoxaparin 40 mg (phase I)1 Inhibition of thrombin generation Enoxaparin 40 mg Rivaroxaban 10 mg 3 2 1 0 0 Lasted ODIXa-HIP tested 30 mg od after THR Efficacy and safety well within the range predicted from twice-daily dosing and similar to enoxaparin (phase II)3 1. Kubitza et al, 2013; Graff et al, 2007; 3. Eriksson et al, 2007 VTE rate (%) for 24 h after a single dose of rivaroxaban 30 mg (phase I)2 8 16 24 32 Time (hours) 40 48 30 30 20 20 10 10 0 0 10 20 30* 40 50 60 Total daily dose (mg) of rivaroxaban *Tested as 30 mg od Major bleeding rate (%) Similar 4 Anti-Factor Xa activity (change from baseline) Inhibition of Factor Xa 0 Enoxaparin 40 mg od The Extensive, Completed Phase III Studies of Rivaroxaban Patients with PE Patients with AF Patients with DVT Patients at risk of secondary VTE Patients undergoing major OS Patients with medical illness Patients with ACS Rivaroxaban: Worldwide Approvals Across the Breadth of Indications VTEx Pulmonary embolism Deep vein thrombosis Approved in 80 countries SPAF Ischaemic stroke Approved in 82 countries VTEp OS ACS Elective hip or knee replacement surgery Unstable angina and myocardial infarction Approved in 112 countries Approved in 46 countries Bayer is Committed to Improving Thrombosis Management Registries N≈97,000 Phase IV/NIS N≈47,000 Phase IIIb N≈2,400 Phase II/III N≈51,000 Completed Phase I–IIIb N≈86,000 Over 275,000 patients expected The Extensive, Ongoing Exploration of Rivaroxaban Patients with PE Patients with DVT Patients with AF Patients with ESUS Patients at risk of secondary VTE Patients with HF and CAD Paediatric patients with VTE Patients with ACS Patients undergoing major OS Patients with medical illness Patients with chronic CAD or PAD Patients with PAD COMPASS CAD/PAD Study Official study title: A Randomized Controlled Trial of Rivaroxaban for the Prevention of Major Cardiovascular Events in Patients With Coronary or Peripheral Artery Disease (COMPASS - Cardiovascular OutcoMes for People Using Anticoagulation StrategieS) Objective: efficacy and safety of rivaroxaban, low-dose rivaroxaban plus ASA or ASA alone for reducing risk of MI, stroke or cardiovascular death in CAD or PAD Rivaroxaban 2.5 mg bid + ASA 100 mg od ± pantoprazole 40 mg od N~21,000 Population: Documented CAD or PAD R 1:1:1 30-day washout period* Rivaroxaban 5.0 mg bid ± pantoprazole 40 mg od ASA 100 mg od ± pantoprazole 40 mg od 30-day run-in, ASA 100 mg Short design: Randomized, double-blind, controlled trial Final follow-up visit# Indication: CAD/PAD Final washout period visit Start: Q2-13 LPLV: Q1-18 *Patients treated according to local standard of care; #≤30 days of the required pre-specified number of events having occurred www.clinicaltrials.gov/show/NCT01776424 COMMANDER HF Chronic HF/CAD Study Official study title: A Randomized, Double-blind, Event-driven, Multicenter Study Comparing the Efficacy and Safety of Oral Rivaroxaban With Placebo for Reducing the Risk of Death, Myocardial Infarction or Stroke in Subjects With Chronic Heart Failure and Significant Coronary Artery Disease Following a Hospitalization for Exacerbation of Heart Failure Objective: efficacy and safety of rivaroxaban for reducing the risk of MI, stroke or death in HF with CAD Rivaroxaban 2.5 mg bid (single or dual antiplatelet therapy) N=5,000 Population: HF and CAD after recent hospitalization ~6–30 months R 15–45-day follow-up Placebo (single or dual antiplatelet therapy) Global treatment end date* Short design: Randomized, double-blind, placebocontrolled, parallel-group, multicenter, event-driven, superiority study *Date when 984 primary efficacy outcome events have occurred www.clinicaltrials.gov/ct2/show/NCT01877915 Indication: HF/CAD5 End of study visit FPFV: Q3-13 LPLV: Q2-16 EINSTEIN CHOICE Long-Term Secondary VTE Prevention Study Official study title: Reduced-dosed Rivaroxaban and Standard-dosed Rivaroxaban Versus ASA in the Long-term Prevention of Recurrent Symptomatic Venous Thromboembolism in Patients With Symptomatic Deep-vein Thrombosis and/or Pulmonary Embolism Objective: efficacy and safety of reduced-dosed rivaroxaban, standard-dosed rivaroxaban versus ASA for the long-term secondary prevention of recurrent symptomatic VTE in patients with symptomatic DVT and/or PE Rivaroxaban 20 mg od Population: DVT and/or PE after 6–12 months of anticoagulation* N~2,850 Day 1 R n~950 Rivaroxaban 10 mg od n~950 ASA 100 mg od n~950 12-month treatment duration Short design: Multicentre, randomized, doubleblind, double-dummy, active-comparator, eventdriven, superiority study Indication: VTEx *Completed 6–12 months (±1 month) with interruption of anticoagulation ≤1 week at randomization www.clinicaltrials.gov/ct2/show/NCT02064439 1 month observation period FPFV: Q1-14 LPLV: Q4-16 Addressing the Unmet Medical Needs….. In Secondary Prevention of ACS rivaroxaban 2.5 mg twice daily in combination with a single antiplatelet agent, including the novel antiplatelets rivaroxaban 2.5 mg twice daily in combination with a single antiplatelet, a new Phase II study in >2,000 patients with ACS across >10 countries in Stroke Prevention ESUS accounts for about 25% of ischaemic strokes Clinical trials have addressed secondary prevention for all major types of ischaemic stroke except ESUS High likelihood that anticoagulants would be effective for secondary stroke prevention in patients with ESUS In PAD The PAD POST INTERVENTION Study Exploring the benefits of rivaroxaban in reducing thrombotic vascular complications in moderate to high risk patients undergoing either peripheral artery bypass graft or percutaneous peripheral artery interventions LCM Phase IV + NIS Programme Overview Study Indication Objective FPFV/ LPLV ACSsp Rivaroxaban plus dual antiplatelet therapy vs UFH during elective PCI (N=107)1 Q4-11 Q1-13 SPAF Efficacy and safety of rivaroxaban for prevention of CV events in Q4-12 non-valvular AF patients undergoing cardioversion vs VKA Q1-14 (N=1,504)2 SPAF Efficacy of rivaroxaban for LA thrombus resolution in nonvalvular AF/flutter patients (N~60)3 Q3-13 Q2-15* SPAF Safety of uninterrupted rivaroxaban vs VKA in non-valvular AF patients undergoing catheter ablation (N~250)4 Q1-13 Q4-14* SPAF/ ACSsp Safety of two rivaroxaban regimens vs VKA after PCI in nonvalvular AF patients (N~2,100)5 Q2-13 Q2-15* VTEp OS Safety and efficacy of rivaroxaban vs SOC in VTE prophylaxis after major orthopaedic surgery (N=17,701)6 Q1-09 Q4-12 VTEx Safety of rivaroxaban vs SOC for acute DVT treatment (N=4,800)7 Q2-12 Q1-15* SPAF Safety of rivaroxaban for stroke prevention in non-valvular AF. Region: Europe (N=6,000)8 Q2-12 EU: Q4-14* *Subject to change. Abbreviations and details of studies on www.clinicaltrials.gov are found in slide notes X-PLORER PCI Study Official study title: Prospective, Multi-center, Randomized, Heparin-controlled Dose-finding Trial to Evaluate the Efficacy and Safety of Rivaroxaban, a Direct Factor Xa Inhibitor, on the Background of Standard Dual Antiplatelet Therapy to Support Elective Percutaneous Coronary Intervention Objective: compare rivaroxaban with UFH therapy, on a background of dual antiplatelet therapy, for suppression of thrombosis and related ischaemic events during elective PCI Rivaroxaban 20 mg* N=107 Population: Symptomatic CAD undergoing elective PCI‡ Index PCI Rivaroxaban 10 mg* R Rivaroxaban 10 mg* plus UFH 50 IU/kg bolus# 30 + 7 days 2:2:2:1 UFH 70–100 IU/kg bolus# Follow-up Short design: Prospective, randomized, semiblinded study Indication: SPAF FPFV: Q4-11 LPLV: Q1-13 *Single dose 2–4 hours before index PCI procedure; #5 minutes before PCI (after catheter sheath insertion) to end of PCI; ‡All patients on stable dual antiplatelet therapy ≥5 days before PCI www.clinicaltrials.gov/ct2/show/NCT01442792 RIVAROXABAN AT THE DOSES TESTED, EFFECTIVELY SUPPRESSED THROMBIN GENERATION AND AMPLIFICATION UPON BALLOON DILATATION AND STENTING. A rebound phenomenon was noticed in the heparin (only) group, but not with rivaroxaban. 10 0.4 0.3 0.2 0.1 0.0 1-5 start 0.5 hrs 2 hrs 6-8 hrs 48 hrs days PCI TAT complex (mcg/L) F1+2 (nmol/L) Median vs. time curves plotted by individual treatment for median anti-Xa activity, pro-thrombin time, activated partial thromboplastin time, endogenous thrombin potential per treatment. 8 6 4 2 0 1-5 days 20 mg 10 mg + UFH 10 mg UFH 2.0 20.0 1.5 15.0 PT (seconds) Anti-Xa (U/mL) PCI prior prior 10 mg start 0.5 hrs 2 hrs 6-8 hrs 48 hrs 1.0 0.5 0.0 20 mg 10 mg + UFH UFH 10.0 5.0 0.0 1-5 start days PCI 0.5 hrs 2 hrs 6-8 hrs 48 hrs days prior 10 mg 1-5 start 0.5 hrs 2 hrs 6-8 hrs 48 hrs PCI prior 20 mg 10 mg + UFH UFH 10 mg 20 mg 10 mg + UFH FOR PRESENTATION PURPOSES ONLY. DO NOT DISTRIBUTE. UFH The results of Xplorer contrast with these of the Randomized, Open-label, DoseRanging study of Dabigatran Etexilate, a Novel, Oral, Direct Thrombin-inhibitor in clinical development, in Elective Percutaneous Coronary Intervention (D-fine) study. Vranckx P et al. Eurointervention 2013. Numerically, there were fewer thrombotic events and less bleeding complications with rivaroxaban. Major bleeding events did not occur in any treatment group. Overall the trial was too small to draw any conclusion regarding differences in clinical outcome. Rivaroxaban 10mg Rivaroxaban Rivaroxaban 20mg 10 or 20mg Rivaroxaban 10mg plus heparin Heparin (n:32) (n:62) (n:29) 0 (0) 0 (0) 0 (0) 0 (0) 1 (6.25) 0 (0) 3 (9.4) 3 (4.8) 4 (13.8) 5 (31.3) 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) 4 (13.3) 1 (3.1) 5(8.1) 5 (17.2) 4 (25.0) 3 (10.0) 1 (3.1) 4 (6.5) 4 (13.8) 3 (18.8) 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) (n:16) (n:30 ) Bailout AC therapy and/or flow limiting thrombotic event* MYOCARDIAL INFARCTION Peri-procedural Spontaneous, up to 30 days BLEEDING TIMI_class Significant (major or minor) Requiring medical attention BARC_class 2, 3 or 5 3 or 5 AC denotes anticoagulation therapy. TIMI denotes Thrombolysis In Myocardial Infarction, ARC denotes academic research consortium, ND denotes not done X-VERT Cardioversion Study Official study title: A Prospective, Randomized, Open-label, Parallel-group, Active-controlled, Multicenter Study Exploring the Efficacy and Safety of Once-daily Oral Rivaroxaban (BAY59-7939) Compared With That of Dose-adjusted Oral Vitamin K Antagonists (VKA) for the Prevention of Cardiovascular Events in Subjects With Nonvalvular Atrial Fibrillation Scheduled for Cardioversion Yes: direct cardioversion R Sufficient anticoagulation or immediate TEE 1–5 days 2:1 VKA (INR 2–3) N=1,500 No: delayed cardioversion Rivaroxaban 20 mg od* R ≥21 days (max. 56 days) 2:1 VKA (INR 2–3) Short design: Prospective, randomized, open-label, blinded endpoint evaluation, parallel-group, active controlled, multi-center study Indication: SPAF *CrCl 30–49 ml/min: 15 mg od http://www.clinicaltrials.gov/ct2/show/NCT01674647 Ezekowitz MD et al. Am Heart J 2014 Cardioversion Population: Non-valvular AF lasting >48 hours or unknown duration, scheduled for cardioversion (electrical or pharmacological) Rivaroxaban 20 mg od* Cardioversion Objective: efficacy and safety of rivaroxaban versus VKA for prevention of cardiovascular events in AF patients scheduled for cardioversion Rivaroxaban 20 mg od* SOC 42 days 30-day follow-up VKA (INR 2–3) SOC Rivaroxaban 20 mg od* SOC 42 days 30-day follow-up VKA (INR 2–3) SOC FPFV: Q4-12 LPLV: Q1-14 Time to cardioversion by cardioversion strategy Median time to cardioversion 100 Days 80 p<0.001 60 p=0.628 40 22 days 20 30 days Patients (%) Rivaroxaban VKA Patients cardioverted as scheduled* 100 Rivaroxaban VKA 80 77.0 p<0.001 60 1 patient with inadequate anticoagulation 40 36.3 20 95 patients with inadequate anticoagulation 0 0 Early Delayed Delayed group *Reason for not performing cardioversion as first scheduled from 21–25 days primarily due to inadequate anticoagulation (indicated by drug compliance <80% for rivaroxaban or weekly INRs outside the range of 2.0–3.0 for 3 consecutive weeks before cardioversion for VKA) X-TRA LA/LAA Thrombus Resolution Study Official study title: An Open-label, International, Multicenter, Interventional Study Exploring the Efficacy of Once-daily Oral Rivaroxaban (BAY 59-7939) for the Treatment of Left Atrial/Left Atrial Appendage Thrombus in Subjects With Nonvalvular Atrial Fibrillation or Atrial Flutter Objective: efficacy of rivaroxaban for resolution of LA/LAA thrombus (confirmed by TEE) in non-valvular AF or atrial flutter Rivaroxaban 20 mg od* Population: Non-valvular AF or atrial flutter with LA/LAA thrombus detected via TEE Standard of care N~60 6 weeks Treatment assignment (baseline data) Short design: Single arm, multicenter, prospective, open-label, interventional study *CrCl 15–49 ml/min: 15 mg od www.clinicaltrials.gov/show/NCT01839357 30 days End-of-treatment TEE Indication: SPAF FPFV: Q3-13 LPLV: Q2-15 End of follow-up VENTURE-AF Catheter Ablation Study Official study title: A Randomized, Open-label, Active-controlled Multi-center Study to Assess Safety of Uninterrupted Rivaroxaban vs. Usual Care in Subjects Undergoing Catheter Ablation Therapy for Atrial Fibrillation Rivaroxaban 20 mg od N~25,013 Population: Paroxysmal or persistent non-valvular AF, first ever catheter ablation R ≥28 days 1:1 VKA (INR 2–3) Day 1 Short design: Randomized, open-label, activecontrolled, multicenter study www.clinicaltrials.gov/ct2/show/NCT01729871 Catheter ablation procedure: Intravenous heparin (target ACT = 300–400 seconds) Objective: safety of rivaroxaban versus VKA in AF patients undergoing catheter ablation ≥4 weeks Indication: SPAF Rivaroxaban 20 mg od 30±5 days follow-up VKA (INR 2–3) ≥8 weeks FPFV: Q1-13 LPLV: Q4-14 PIONEER AF-PCI PCI Study Official study title: An Open-label, Randomized, Controlled, Multicenter Study Exploring Two Treatment Strategies of Rivaroxaban and a Dose-Adjusted Oral Vitamin K Antagonist Treatment Strategy in Subjects With Atrial Fibrillation Who Undergo Percutaneous Coronary Intervention Objective: safety of two rivaroxaban regimens versus VKA after PCI (with stent placement) in non-valvular AF Rivaroxaban 15 mg od*# + clopidogrel Population: Paroxysmal, persistent or permanent AF, undergoing PCI (with stent placement) N=2,100 Rivaroxaban 2.5 mg bid# + DAPT‡ Rivaroxaban 15 mg od* + low-dose ASA R 1:1:1 Intended DAPT duration of 1, 6 or 12 months VKA (INR 2.0–3.0)§ + DAPT‡ Short design: Open-label, randomized, multicenter study VKA + low-dose ASA End of treatment (12 months) Indication: SPAF/ACS FPFV: Q2-13 LPLV: Q2-15 *CrCl 30–49 ml/min: 10 mg od; #first dose 72–96 hours after sheath removal; ‡ASA (75–100 mg daily) + clopidogrel (75 mg daily) (alternative use of prasugrel or ticagrelor allowed, but capped at 15%); §first dose 12–72 hours after sheath removal www.clinicaltrials.gov/ct2/show/NCT01830543 Bayer is Committed to Improving Thrombosis Management Registries N≈97,000 Phase IV/NIS N≈47,000 Phase IIIb N≈2,400 Phase II/III N≈51,000 Completed Phase I–IIIb N≈86,000 Over 275,000 patients expected Clinical Trials vs Real-Life Experience Clinical study Strict inclusion and exclusion criteria Strict study protocol Objectively adjudicated event rates Strict guidance for problematic cases Real life Only indications and contra-indications regulated Dose recommendations for groups of patients only Over- and under-representation of events Limited guidance for problematic cases Capturing Real-Life Experience with Rivaroxaban/Novel OACs Non-interventional studies I and II (US) Bayer/Janssen support (Europe) Dresden NOAC (Dresden, Germany) Global AF registry Results of RECORD Studies Confirmed in Real-Life Practice Incidence (%) 2.0 10.0 8.0 1.5 1.3 7.0 Rivaroxaban Enoxaparin SOC 6.5 6.0 1.0 4.7 1.0 4.0 0.6 2.2 0.5 2.0 0.4 0.2 0.0 3.2 0.6 1.8 1.7 1.4 0.4 0.3 Major Major Any bleeding¹ Major Major Any bleeding² Symptomatic VTE¹ Symptomatic VTE² bleeding bleeding bleeding bleeding (RECORD)¹ (EMA)¹ (RECORD)² (EMA)² Different treatment durations in RECORD and XAMOS; all events treatment emergent. SOC, standard of care (82% LMWH) 1. Turpie et al, 2011; 2. Turpie et al, 2013 GARFIELD...Uptake of Novel OACs VKA, Vitamin K antagonists; FXa, Factor Xa inhibitors; DTI, Direct thrombin inhibitors; AP, Antiplatelets Bayer is Committed to Improving Thrombosis Management Registries N≈97,000 Phase IV/NIS N≈47,000 Phase IIIb N≈2,400 Phase II/III N≈51,000 Completed Phase I–IIIb N≈86,000 Over 275,000 patients expected Global Clinical IIR Status: 100 IIRs with Rivaroxaban Ongoing* Others 20 Device surgery Worldwide IIR network 1 ACS/atherosclerosis Europe 43 1 VTEp Americas 13 5 VTEx Asia 38 15 SPAF 58 Multinational 6 All 100 0 *Status Oct 2014 based on IMPACT 20 40 60 80 100 120 Responsible Use is Crucial The basics Right dose for the Right patient for the Right indication Practical questions Concomitant medications Transition to and from ‘Xarelto’ Management of bleeding To Meet the Needs for Improved Treatments Options Our R&D Goals Predictable, once daily oral administration Potent antithrombotic activity Scientific Research Continues in BAYER Broad therapeutic window No routine coagulation monitoring Long-term anticoagulation therapy from hospital to home Research in Indications with High Unmet Medical Needs Cardiology research covers diseases in: Blood Lung Heart Kidney Thrombosis Pulmonary hypertension Heart failure Chronic kidney disease Increased blood pressure in lung vessels leading to lung dysfunction and right heart insufficiency The heart fails to pump blood at a sufficient rate to meet the metabolic requirements of the body Impaired kidney function due to damage to fine capillaries in the glomeruli Development of arterial or venous thrombi preventing blood flow in vessels Anaemia Decreased erythropoiesis in chronic kidney disease Development Pipeline Phase I (14) Cardiovascular Phase III (16) Phase II (14) Cancer Roniciclib (BAY 1000394) (CDK-Inhibitor) Heart Failure BAY 86-8050 (Vasopr. Rec. Antag.) Diabetic Nephropathy Finerenone (MR-Antagonist) Heart Failure BAY 1067197 (Part. Aden. A1 Agonist) Skin and Lung Infections Tedizolid Cancer Anetumab ravtansine (BAY 94-9343) (Mesothelin-ADC) Cancer BAY 1125976 Allosteric AKT 1/2 - I. CHF Finerenone (BAY 94-8862) (MR-Antagonist) Additional Indications Sorafenib Hemophilia Damoctocog alfa pegol (BAY 94-9027) (peg rFVIII mutein) Sympt. Uterine Fibroids BAY 1002670 (S-PRAnt) Cancer BAY 1143572 PTEFb Inhibitor NHL Copanlisib (BAY 80-6946) (PI3k Inhibitor) Cancer BAY 2010112 PSMA BiTE Antibody. Cancer Bronchiectasis BAY 85-8501 Neutroph. Elastase Inhibit. Cancer BAY 1179470 FGFR2 Ab Contraception BAY1007626 (Progestin IUS) Cancer Heart failure BAY 1142524 Chymase Inhibitor Lung disease BAY 1097761 PEGylated Adrenomedullin Worsening chronic heart failure Vericiguat (BAY 1021189) (sGC Stimulator) Endometriose BAY 98-7196 Intravaginal ring Cancer BAY1163877 Pan-FGFR Inhibitor Anemia Molidustat (BAY 85-3934 (HIF-PH Inhibitor) BAY1082439 (PI3k Inhibitor) Refametinib (BAY 86-9766) Cancer Regorafenib Combination study in CRPC Radium-223-Dichloride Regorafenib Gram-negative Pneumonia Amikacin inhale Breast Cancer Sorafenib PH.IIP MACE prevention Riociguat (sGC Stimulator) Rivaroxaban Adjuvant RCC Sorafenib Diffuse Systemic sclerosis CHF and CAD Riociguat (sGC Stimulator) Rivaroxaban Raynaud's phenomenon Riociguat (sGC Stimulator) Long-term VTE prevention Rivaroxaban Contraception LCS 16 Cancer Medically ill Non-CF Bronchiectasis Radium-223-Dichlorid Rivaroxaban Cipro DPI HCC 2nd line RESPITE study (insuff. responders to PDE5-inhib.) Regorafenib Status April 2014 Selection of major Pharma pipeline projects in clinical Phase I to III Adjuvant CRC with resected liver metastases *Regorafenib is a Bayer compound developed solely by Bayer. In 2011, Bayer entered into an agreement with Onyx Pharmaceuticals, Inc. under which Onyx will receive a royalty on any future global net sales of regorafenib in oncology http://pharmatoday.bhc.cnb/APPS/BSP/DE/BSP-GPM/BSP-GPM.nsf/id/EN_Pipeline_external VV Atrophy Prasterone (Vaginorm) Riociguat New molecular entities (NME) Life cycle management (LCM) Thank you very much for your attention