Cardiac Output
advertisement
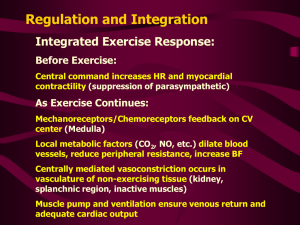
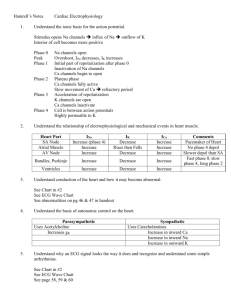
Cardiac Output When the heart contracts Cardiac Vocabulary • Contractility: Contractility is the intrinsic ability of cardiac muscle to develop force for a given muscle length. Cardiac Vocabulary • Preload: Preload is the muscle length prior to contractility, and it is dependent of ventricular filling (or end diastolic volume…EDV) • This value is related to right atrial pressure. • The most important determining factor for preload is venous return. Cardiac Vocabulary • Afterload: Afterload is the tension (or the arterial pressure) against which the ventricle must contract. • If arterial pressure increases, afterload also increases. • Afterload for the left ventricle is determined by aortic pressure • Afterload for the right ventricle is determined by pulmonary artery pressure. Cardiac Output Cardiac Output is the volume of blood pumped each minute, and is expressed by the following equation: • CO = SV x HR • Where: • CO is cardiac output expressed in L/min (normal ~5 L/min) • SV is stroke volume per beat • HR is the number of beats per minute Cardiac out put • CO is amount of blood pumped from each ventricle it means left ventricular out put through aorta into various organs of body • Stroke volume is defined as amount of blood pumped out by each ventricle during each beat ---normal value is 70ml Variations in cardiac out put • Age,less in chilren bc less blood volume • Sex,female less cardiac out put bc less body surface area • Body build,greater the body build more is cardiac outputs • Diurnal, increase in day time depend on basal conditions • Emotional condition,due to realse of catecolamine increase HR &force of contraction • After meal • Exercise,bc increase HR & force of contraction • Fever,increase oxidative process • Anemia,due to hypoxia • Hyperthyroidism bc increase basal metabolic rate Decrease in CO • Hypothyroidism • Atrial fibrillation bc of incomplete filling • Incomplete heart block,bc defective pumping action • Shock bc poor pumping actoin • Haemorrage bc of decrease blood volume Factor maintaining CO • Venous Return,this is amonut of blood returning to heart from diff part of body • Directly proportional • 5 factors • Respiratory pump • During inspiration intrapleural pressure become more negative,descent of diaphram incr intra abdominal pressure,compress abdominal veins,push the blood upward towards heart • So flow of blood in Right atrium increase • Muscle pump • During muscular activities veins are compressed so blood is moved towards heart,more venous return • Gravity,reduced venous return.person stand for long time gravity cause pooling of blood in legs so blood return to heart is dec • Smpathetic tone cause constriction of venules,constriction push blood toward heart • Vasomotor tone is continues discharge of impulse from vasoconstrictor center produced constant partial state of constriction of blood vessel so the arterial pressure is directly proportion to vasomotor(sympathetic)tone Force of contraction • This peroid depend upon diastolic peroid & ventricular filling muscle are stretched result increase in length of muscle fiber • Directly proportional Heart Rate • Directly proportional • Increase HR diastolic peroid is short and ventricle filling is decreased Peripheral Resistance • It resistance offered to blood flow at peripheral blood vessel • Inversely proportional Heart Rate (HR) Heart rate is directly proportional to cardiac output • Adult HR is normally 72 beats per minute (bpm.) • Heart rate is modified by autonomic, immune, and local factors. For example: 1. An increase in parasympathetic activity via M2 cholinergic receptors in the heart will decrease the heart rate. 2. An increase in sympathetic activity via B1 and B2 adrenergic receptors throughout the heart will increase the heart rate. Stroke Volume (SV) SV = EDV - ESV • Is determined by three factors: preload, afterload, and contractility. • Preload gives the volume of blood that the ventricle has available to pump • Contractility is the force that the muscle can create at the given length • Afterload is the arterial pressure against which the muscle will contract. • These factors establish the volume of blood pumped with each heart beat. Preload afterload Cardiac Volumes • SV = end diastolic volume (EDV) - end systolic volume (ESV) • EDV = amount of blood collected in a ventricle during diastole • ESV = amount of blood remaining in a ventricle after contraction Cardiac Reserve • Cardiac reserve is the difference between resting and maximal CO • Cardiac Output: Example CO (ml/min) = HR (75 beats/min) x SV (70 ml/beat) • CO = 5250 ml/min (5.25 L/min) Frank – Starling Principle • This principle illustrates the relationship between cardiac output and left ventricular end diastolic volume (or the relationship between stroke volume and right atrial pressure.) Frank – Starling Principle • The Frank Starling principle is based on the length-tension relationship within the ventricle. • If ventricular end diastolic volume (preload) is increased, it follows that the ventricular fiber length is also increased, resulting in an increased ‘tension’ of the muscle. • Cardiac output is directly related to venous return, the most important determining factor is preload. • The contraction and therefore stroke volume in response to changes in venous return is called the Frank-Starling mechanism (or Starling's Law of the heart). How (TPR)Total Peripheral Resistance effects CO Regulation of Heart Rate: Autonomic Nervous System • Sympathetic nervous system (SNS) stimulation is activated by stress, anxiety, excitement, or exercise • Parasympathetic nervous system (PNS) stimulation is mediated by acetylcholine and opposes the SNS slowing heart rate • Baroreceptors a. carotid sinus reflex - maintains BP in brain • b. Bainbridge reflex – maintains BP in heart • c. Aortic sinus reflex – maintains BP in aorta Bainbridge Reflex • Bainbridge (atrial) reflex – a sympathetic reflex initiated by increased blood in the atria • Causes stimulation of the SA node • Stimulates baroreceptors in the atria, causing increased SNS stimulation Cardiac Neurotransmitters & Receptors Chemical Regulation of the Heart • The hormones epinephrine and thyroxine (T4) increase heart rate • Hormonal Regulation of Blood Pressure 1. Renin 2. ADH 3. Aldosterone • Intra- & extracellular ion concentrations must be maintained for normal heart function Homeostatic Imbalances • Hypocalcemia – reduced ionic calcium depresses the heart • Hypercalcemia – dramatically increases heart irritability and leads to spastic contractions • Hypernatremia – blocks heart contraction by inhibiting ionic calcium transport • Hyperkalemia – leads to heart block and cardiac arrest Congestive Heart Failure (CHF) caused by: • Coronary atherosclerosis • Increased blood pressure in aorta • Successive myocardial infarcts • Dilated cardiomyopathy (DCM) Coronary Artery Bypass Surgery Heart Auscultation Aortic Stenosis Diastolic Murmur Mid Systolic Click Normal Heart Beat