Methadone
advertisement
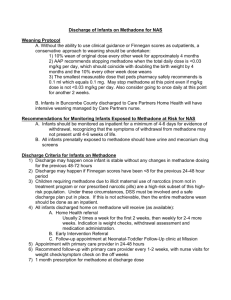
General Properties and Utility Identify the unique pharmacological properties of methadone that distinguish it from other opioids Learn key properties of methadone lending itself to treatment of cancer pain, neuropathy pain, and opioid addiction. Recognize potential side effects and unique challenges to properly managing methadone for analgesia Schedule II opioid developed in Germany in 1940s as spasmolytic Synthetically derived 6-dimethylamino-4,4-diphenyl-3-heptanone 1960s - usage in treatment of heroin addiction Mid 1970s - usage as general analgesic Today –treatment of opioid addiction, chronic pain, cancer pain, neuropathy, renal and hepatic failure. social stigma and lack of familiarity amongst physicians Differs from other opioids in terms of bioavailability, multiple receptor affinities, low cost, lack of toxic metabolites Structurally unrelated to other opioids Racemic mixture 2 isomers: D-isomer: (S-met) – NMDA receptor antagonist + inhibits uptake of norepi & serotonin L-isomeer (R-met) – mu and delta agonist High lipophilicity with oral bioavailability 40-99% Large tissue reservoir Acts as both IR (onset 20-30min) and SR Exists in all conventional formulations Pka 9.2 (basic) Highly bound to alpha-1-acid-glycoprotein, unbound fraction 12% highly variable Peak plasma conc 2.5-4 hrs T ½ 30 Analgesic 4-6 hrs initially, up to8-12 with repeated dosing Biphasic Elimination Alpha – 8-12 hr, rapid redistribution (analgesia) Beta – 30-60hrs, sufficient to prevent withdrawal only Extensive hepatic metabolism by cytochrome P450 family via N-methylation Traditionally attributed to CYP3A isoenzyme 2009 Evan et al. Demonstrated >90% inhibition of hepatic & intestinal CYP3A activity by ritonavir/indinavir lead to slighltly increased N-demethylation but no significant effect on methadone plasma concentration, bioavailability, hepatic extraction orsystemic clearance, suggesting little or no role of CYP3A in methadone clearance and metabolism Suggests CYP3A-based guidelines may be incorrect Totah et al. suggests CYP2B6 primary isoenzyme for bulk of methadone metabolism P450 metabolism Methadone metabolism produces no active metabolites! Fecal elimination (primary) Renal elimination (minor) Varies depending on urinary pH Cancer Pain Neuropathic Pain Drug interactions Opioid Addiction >80% Cancer pts require opioid analgesics for intractable pain prior to death No ceiling effect Efficacy limited by toxicity: N, V, constipation, sedation, hallucinations, myoclonus Opioid Rotation Indications: Toxicity Tolerance Refractory pain Advantages of Methadone Excellent oral & rectal bioavailability Incomplete cross tolerance Long T ½ with rapid onset No toxic metabolites Multpile Receptors involved Mu and delta agonist NMDA antagonist – hyperalgesia, chronic pain states, neuropathic pain Less constipation Methadone may be first-line opioid choice NMDA antagonism -neuropathic pain modulator -believed to attenuate development of morphine tolerance Inhibition of Seretonin & Norepi reuptake Ie TCA’s High lipophilicity = 3x bioavailability of MSO4 IR & SR action Duration up to 10h with chronic dosing Minimal renal excretion & lack of metabolites well suited for diabetic neuropathy w/ renal insufficiency Evidence of efficacy largely anecdotal Limited to case studies Nadege et al. retrospective study with questionair (n=13) patients with neuropathic pain poorly controlled on conventional analgesic. S/p 12 mo methadone therapy avg 43% pain relief, 47% improvement quality of life, 30% improvement quality of sleep. 62% experienced improvement all areas. Comprehensive literture review by Sandoval et all Clin. Jounal of pain 2005 1 randomized trial, 13 case reports, 7 case series, 545 pts “no consistent evidence-based substantiation of methadone’s clinical impact in the treatment of noncancer pain” Usage Trends: 1.) failed convention opioid therapy from toxicity, tolerance, side effects 2.) first-line tx for certain classes of chronic pain 3.) pain treatment in addicts Estimated 1 million long term opioid users in U.S.A. Methadone Maintenance Programs GOALS Block effect of other opiods Ie 80-120mg/day blocks effects of IV heroin, hydromorphone, methadone (“agonist blockade”) 10-20 mg/day to stems withdrawal but not craving Reduced cravings Relieves withdrawal symptoms BENEFITS Mortality reduction: U.S. untreated heroin addicts 8.3% yearly mortality versus 0.8% treated. Morbidity reduction: ↓ IVDU, recidivism, crime, ↓ sexual risk behaviors Controversial – Trading one addiction for another? Methadone Maintenance Programs Heavily regulated By law, physician CANNOT prescribe methadone to tx opioid withdrawal from office Any M.D. with DEA # can prescribe “for pain” Methadone’s unique physical and pharmacological properties present unique challenges to proper management in the areas of: Overdose Equianalgesia Interindiviual variability of metabolism Dangerous side effects Primary danger in prescribing for analgesia is risk of delayed respiratory depression Variable but long T ½ → steady state my take >1 week to achieve Delayed side effects in outpatient setting Methadone for analgesia ↑ 1,300% 1997-2003 Adverse events ↑ 1800% 1997-2007 Fatalities ↑ 390% 1997-2007 Widely variable plasma concentrations with similar dosages Mechanism no clearly understood Possible explanations include Differences in alpha-1-glycoprotein binding Effects of urinary pH on renal clearance Multiple drugs can affect P450 system Methadone => hepatic autoinduction Morphine:Methadone ratios vary depending on prior opioid exposure. Highly tolerant individuals require LESS methadone for equianalgesia than opioid naïve pts incomplete cross tolerance Methadone is a mixed mu-delta agonist Methadone NMDA antagonism may also reduce cross tolerance END RESULT: patients tolerant to high dose opioids are at increased risk of toxicity Example of equianalgesia table Daily MSO4 <100mg 101-300mg 301-600mg 601-800mg 801-1,000mg >1,000mg Coversion Ratio to Methadone 3:1 5:1 10:1 12:1 15:1 20:1 QTc prolongation dose dependent at >60mg/day Advised to check QTc interval prior to and during methadone titration Pain Medications that Prolong QTc Interval Anticonvulsants Gabapentin Lyrica Fosphenytoin Pheytoin SSRI Citalopram Sertraline Fluoxetin Paroxetine Escitalopram TCA Amitriptyline Doxepin Nortiptyline Desipramine Clomipramine Imipramin Protriptyline mirtazapin Misc Antidepressants Duloxetine (cymbalta) Venlafaxine Muscle Relaxants Cyclobenzapine (Flexeril) Tizanidine NSAIDS Celecoxib Diclofenac Etodolac Ibuprofen Meloxicam Sulinda Ketoprofen OPIATES Fentanyl Sufentanil Alfentanil Hydromorphone Levorphanol Methadone Methadone is unique among opioids in terms of its high bioavailability, multiple receptor affinities , extended half-life, and lack of active metabolizes. These properties lend itself to the treatment of opioid tolerant pain syndromes such as cancer, potentially neuropathic pain, and treatment of opioid addiction. Aside from social stigma, the unpredictable nature of interindividual metabolism, counter intuitive equianalgesic dosing, and risk of delayed toxicity make methadone a challenging drug to manage in the outpatient setting. Benzon, HT. Essentials of Pain Medicine and Regional Anesthesia, Second Edition. Copyright 2005. Hayes, Lewis et al. Use of Methadone for the Treatment of Diabetic Neuropathy. Diabetes Care, Vol 28, No 2 February 2005, Pp 345-313 Mancini, Isabelle et al. Opioid Switch to Oral Methadone in Cancer Pain. Current Opinion in Oncology, Vol 12, 2000. Pp 308-313 Nadege, Altier et al. Management of Chronic Neuruopathic Pain with Methadone: A Review of 13 Cases. Clinical Journal of Pain, Vol 21, No 4, July/Aug 2005, Ps 364-369 Alberto, Juan et al. Oral Methadone for Chronic Noncancer Pain: A Systematic Literature Review of Reasons for Administration, Prescription Pattersn, Effectiveness, and Side Effects. Clinical Journal of Pain, Vol 21, No 6, Nov/Dec 2005, Pp503-512 Clifford Gevirtz, Methadone’s Role in Pain Management: New Dangers Revealed, Topics in Pain Management, Vol 23, No 5, December 2007, Pp 1-5 Vocci, Frank et al. Medication Development for Addictive Disorders: The State of Science. American Journal of Psychiatry, Vol 162, No 8, Aug 2008. Pp 1432-1440 Kharasch, Evan et al. Methadone Pharmacokinetic Are Independent of Cytochrome P450A (CYP3A) Activity and Gastrointestinal Drug Transport: Insights from Methadone Interactions with Ritonavir/Indinavir, Anesthesiology, Vol 110, No 3, March 2009, Pp660672